Community
Quitting gave me better health, my dignity and more cash

Quitting gave me better health, my dignity and more cash
I had this terrible constant cough. It was like I had a cold that never went away. When I did actually get a cold it was like I was never getting any better. I also began noticing that when I would cough I would release a small amount of urine. After a while as the cough progressed the urine would come out in larger quantities. I could no longer wear just a panty liner I was wearing full sized extra absorbent pads. When I was out with family and friends having a good time, I would laugh and start choking uncontrollably forcing so much urine out that I would wet through my pants and have to go home. Even if I just went to the bathroom I would still wet myself. I thought at 38 I would be in Depends.
I had thought about quitting smoking many times but I think stress was my number one deterrent from quitting. Every time I was gonna try, something would cause me stress, I had myself tricked into thinking that smoking was the only way I could deal with stress. Stress came from everywhere, work home and finances.
I tried to quit before on two occasions however, I was not successful on either one. The first time I used the patch, but couldn’t break the habit. The second time was with Champix and I was smoke-free for approximately 2 and a half months when I said to a friend that smokes that I was having a craving. She said sometimes you just need one to take the edge off and gave me a cigarette. I stopped and bought a pack on my way home.
This time I used the Champix again. I stopped constant communication with friends and family who smoke. I misplaced the last 2 weeks of the Champix program and had no clue where the pills went, but I just keep telling myself I can do it. When I have a craving I give myself something to do so I don’t think about it- shift the focus. Also in the past I noticed that when I have cigarettes I don’t crave as much and when I was almost out or out, I smoked what I had quickly or felt like I was dying until I could get some. My other secret is I still have an opened package of cigarettes to help curb cravings. I don’t want to get rid of them or I’ll want them.
Now, I feel like I can breathe better, smell better and everything tastes better. That nasty constant cough was gone about 2 weeks after I quit. I still have a bit of a cough but no longer pee when I cough. I hated the life that whenever I coughed I peed. All I had to do was stop smoking. I can laugh and enjoy myself without choking. It’s amazing! I wish I never started smoking. I used to use a ton of salt on my food now I can enjoy a meal without any salt, food tastes so much better. When a smoker is sitting next to me I don’t want to be rude but they stink so bad I gag. I feel so bad that my boyfriend had to smell that on me every day.
I suggest any smoker Quits! If there is anything you can change about yourself for the better its quit smoking. I wish I would have the first time because my health was heading on a downward slope and now I feel more alive and energetic like I was when I was a kid. Distance yourself from others who smoke or that aren’t supportive. I started the Champix late December 2019 and started back at school on January 6, 2020. I said I wouldn’t smoke on that day but I did have just one, so January 7, 2020 became my quit date. It was hard at first but I stuck it out and I am glad I did. The PCN Family Nurse gave me good advice and support; I really appreciate that!
Community
Support local healthcare while winning amazing prizes!

|
|
|
|
|
|
|
Community
SPARC Caring Adult Nominations now open!

Check out this powerful video, “Be a Mr. Jensen,” shared by Andy Jacks. It highlights the impact of seeing youth as solutions, not problems. Mr. Jensen’s patience and focus on strengths gave this child hope and success.
👉 Be a Mr. Jensen: https://buff.ly/8Z9dOxf
Do you know a Mr. Jensen? Nominate a caring adult in your child’s life who embodies the spirit of Mr. Jensen. Whether it’s a coach, teacher, mentor, or someone special, share how they contribute to youth development. 👉 Nominate Here: https://buff.ly/tJsuJej
Nominate someone who makes a positive impact in the live s of children and youth. Every child has a gift – let’s celebrate the caring adults who help them shine! SPARC Red Deer will recognize the first 50 nominees. 💖🎉 #CaringAdults #BeAMrJensen #SeePotentialNotProblems #SPARCRedDeer
s of children and youth. Every child has a gift – let’s celebrate the caring adults who help them shine! SPARC Red Deer will recognize the first 50 nominees. 💖🎉 #CaringAdults #BeAMrJensen #SeePotentialNotProblems #SPARCRedDeer
-

 COVID-192 days ago
COVID-192 days agoOntario man launches new challenge against province’s latest attempt to ban free expression on roadside billboards
-

 COVID-1920 hours ago
COVID-1920 hours agoNew Peer-Reviewed Study Affirms COVID Vaccines Reduce Fertility
-

 Alberta2 days ago
Alberta2 days agoAlberta Next Takes A Look At Alberta Provincial Police Force
-

 Business16 hours ago
Business16 hours agoOttawa Funded the China Ferry Deal—Then Pretended to Oppose It
-

 Alberta2 days ago
Alberta2 days agoCanadian Oil Sands Production Expected to Reach All-time Highs this Year Despite Lower Oil Prices
-
 Alberta19 hours ago
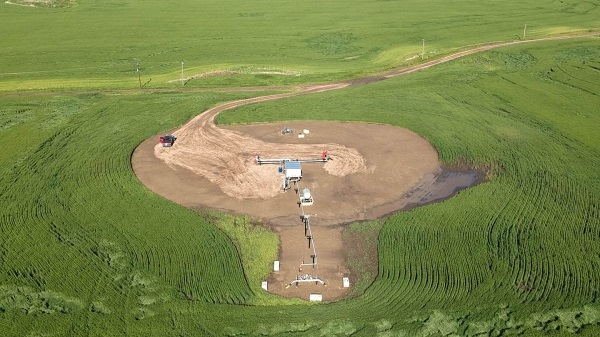
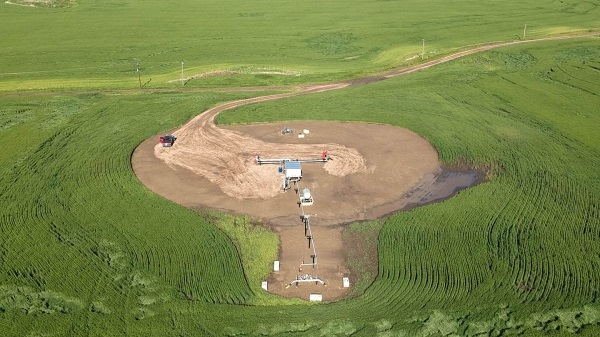
Alberta19 hours agoThe permanent CO2 storage site at the end of the Alberta Carbon Trunk Line is just getting started
-

 MAiD18 hours ago
MAiD18 hours agoCanada’s euthanasia regime is not health care, but a death machine for the unwanted
-

 International2 days ago
International2 days agoPresident Xi Skips Key Summit, Adding Fuel to Ebbing Power Theories








