Alberta
Child and Youth Advocate says Pepper Spray is used far too often in Alberta Young Offender Centres

From the office of Alberta’s Child and Youth Advocate
Child and Youth Advocate releases special report on OC spray and segregation in Alberta’s young offender centres
Alberta’s Child and Youth Advocate has completed a special report on oleoresin capsicum spray (OC spray, commonly referred to as pepper spray) and segregation in young offender centres.
The Advocate is making four recommendations related to reducing the use of OC spray and segregation as well as increasing accountability measures.
“Young people in custody often have complex needs and may present with difficult and challenging behaviours,” said Del Graff, Child and Youth Advocate. “It is imperative that the Young Offender Branch explores approaches to improve the health and well-being of young people while ensuring a safe environment for everyone. I sincerely hope the recommendations from this report will be quickly acted on to improve the circumstances for youth in custody.”
From January to March 2019, the OCYA received input from over 100 stakeholders through community conversations and one-to-one interviews. Young people, youth justice stakeholders, and community stakeholders shared their perspectives and experiences.
The purpose of this report is to provide advice to government related to improving the safety and well-being of young people in custody.
A copy of the report: “Care in Custody: A Special Report on OC Spray and Segregation in Alberta’s Young Offender Centres” is available on our website:
http://www.ocya.alberta.ca/adult/publications/ocya-reports/
The Child and Youth Advocate has the authority under the Child and Youth Advocate Act to complete special reports on issues impacting children and youth who are receiving designated government services. This is the Advocate’s fourth special report.
The Office of the Child and Youth Advocate is an independent office of the Legislature, representing the rights, interests and viewpoints of children and young people receiving designated government services.
Executive Summary
In 2016, the Young Offender Branch, Ministry of Justice and Solicitor General, changed its policy, making it easier for correctional peace officers to use OC spray on incarcerated young people. Since then, the use of OC spray in youth justice facilities has steadily increased. By inflicting pain to control behaviour, the use of OC spray can damage relationships with youth justice staff, undermine rehabilitation efforts, and further traumatize young people.
The use of segregation in young offender centres is also a concern, as it can result in physical, psychological, and developmental harm to young people. Segregation is occurring without sufficient guidelines and safeguards to protect the well-being of young people. The current use of segregation undermines the Youth Criminal Justice Act’s (YCJA) principle of rehabilitation and reintegration. If segregation must occur for safety reasons, it should be short-term and must include meaningful interactions, mental health supports, and programming.
Further, complaints and review processes at young offender centres must be transparent and strengthened so that young people can challenge decisions without facing repercussions. They have the right to be supported through those processes by a person such as an advocate. Public reporting will also help ensure accountability and promote fair treatment of young people in custody.
Increased accountability changes behaviour and choices. Under the old policy, when the tactical team had to be called to use OC spray in youth justice facilities, it was only deployed once in approximately four years. Since correctional peace officers have been able to carry and use OC spray, it has been used on young people 60 times in the last three years. In the last four weeks of finalizing this report, OC spray was used 10 times. This example is alarming and highlights the importance and timeliness of this report.
The treatment of young people in custody should uphold their human rights, in alignment with the United Nations Convention on the Rights of the Child (UNCRC).The current use of OC spray and segregation contradict the intention of the UNCRCand other United Nations rules and conventions.1 The Advocate urges the Young Offender Branch to review its policies and practices to ensure they align with the goals of its legislation and support the human rights of the young people they serve.
The Advocate is making the following four recommendations:
- OC spray should only be used in exceptional circumstances, if there is an imminent risk of serious physical harm to a young person or others.
- The Young Offender Branch should review and update their policies and standards to reduce the number of hours a young person can be segregated, ensure that they receive appropriate programming and supports, and improve conditions within segregation.
- The Young Offender Branch should develop an impartial complaints and review process for young people. An impartial multi-disciplinary committee that includes external stakeholders should hear complaints and reviews, and young people should have access to a supportive adult.
- The Young Offender Branch should monitor and publicly report all incidents of OC spray use and segregation annually.
Alberta
Alberta Provincial Police – New chief of Independent Agency Police Service

Sat Parhar has been appointed as the first chief of the Independent Agency Police Service, marking the next step toward a new municipal policing option.
The appointment of a new chief for the Independent Agency Police Service (IAPS) marks the next step in giving municipalities a new option for local policing and builds on the work already underway for the agency to assume the police-like duties currently carried out by the Alberta Sheriffs. The IAPS will empower municipalities to adopt strategies that effectively respond to their specific safety concerns, enhancing public safety across the province.
Chief Parhar brings more than 25 years of policing experience, including senior roles with the Calgary Police Service, most recently as deputy chief. His frontline policing experience and deep understanding of Alberta’s complex and diverse public safety landscape positions him to lead the agency as it takes shape and begins its work as a new municipal policing option, keeping communities safe.
Once operational, the agency will strengthen Alberta’s existing policing model and complement the province’s current police services, which includes the RCMP, Indigenous policing services and municipal police. It will help fill gaps and ensure law enforcement resources are deployed efficiently to meet Alberta’s evolving public safety needs and improve law enforcement response times, particularly in rural communities.
“Appointing Chief Sat Parhar is a key milestone in Alberta’s plan to give municipalities a real choice in how their communities are kept safe. This is about building a modern police service that reflects the priorities of Albertans, strengthens local decision-making, and ensures every corner of our province, especially rural areas, can count on responsive, effective law enforcement. With his decades of experience and deep understanding of Alberta’s policing landscape, he is the right leader to bring this vision to life.”
“This appointment signifies a significant step forward in our efforts to establish a more robust, community-focused policing model that is better equipped to meet the unique needs of our local residents. Under Chief Parhar’s visionary leadership, we are confident that we will develop a modern, efficient police service that not only enhances public safety but also aligns closely with the priorities and values of Albertans. His experience and commitment are vital in shaping an IAPS that is responsive, transparent, and dedicated to fostering trust and collaboration within the community, ultimately ensuring a safer and more connected society for all.”
Chief Parhar’s immediate priorities will be to hire an executive team and commence organizational planning such as developing key recruitment, training and other operational policies. Chief Parhar’s appointment is the first step of many to establishing the IAPS.
“It’s an honour to take on this role and help shape a modern police service built for Alberta. My focus from day one will be on setting high standards for professionalism, building strong relationships with our partners and ensuring this service reflects the needs and priorities of the communities we serve.”
The Independent Agency Police Service was formally created through regulation following the passing of Public Safety Statutes Amendment Act, 2024. The agency will operate as an independent Crown corporation, and will be renamed the Alberta Sheriffs Police Service, with its head office located in Calgary. The IAPS will be operationally independent from the provincial government with civilian oversight, consistent with all police services in Alberta.
“When it comes to policing, municipalities like ours deserve a choice – especially when the current system leaves us disadvantaged simply because of our size. We look forward to learning more about what that alternative will look like once an Alberta police agency is fully established and the options are clear. For us, this is about fairness, sustainability, and ensuring municipalities have access to policing solutions that reflect both their needs and their realities.”
Quick facts
- The regulation establishes the IAPS Provincial Corporation and its governance structure including board of directors, board of director powers, financial responsibilities and accountabilities.
Related news
- Expanding municipal police service options (April 7, 2024)
Alberta
Pierre Poilievre – Per Capita, Hardisty, Alberta Is the Most Important Little Town In Canada

From Pierre Poilievre
-

 Business2 days ago
Business2 days agoOttawa Funded the China Ferry Deal—Then Pretended to Oppose It
-

 COVID-192 days ago
COVID-192 days agoNew Peer-Reviewed Study Affirms COVID Vaccines Reduce Fertility
-

 MAiD2 days ago
MAiD2 days agoCanada’s euthanasia regime is not health care, but a death machine for the unwanted
-
 Alberta2 days ago
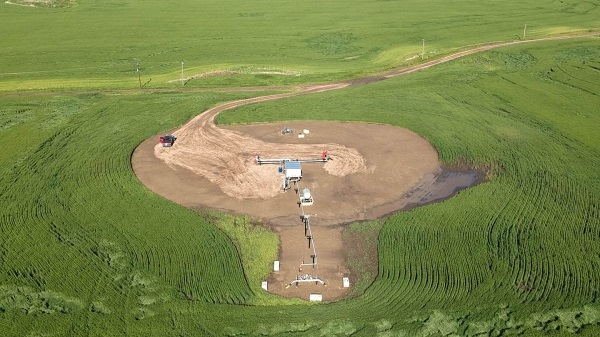
Alberta2 days agoThe permanent CO2 storage site at the end of the Alberta Carbon Trunk Line is just getting started
-
 Business1 day ago
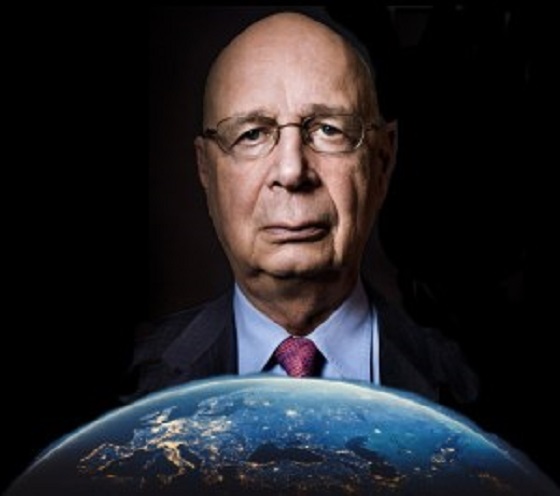
Business1 day agoWorld Economic Forum Aims to Repair Relations with Schwab
-

 Alberta2 days ago
Alberta2 days agoAlberta’s government is investing $5 million to help launch the world’s first direct air capture centre at Innisfail
-
 Business2 days ago
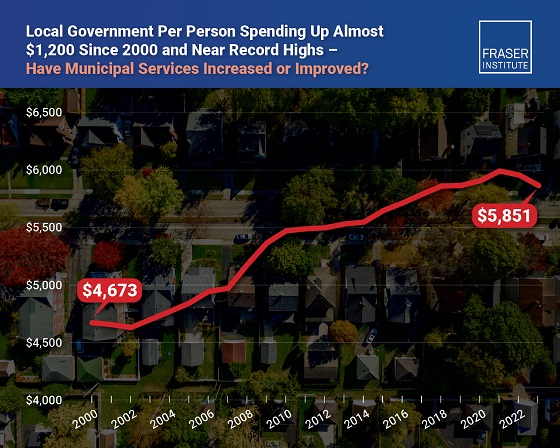
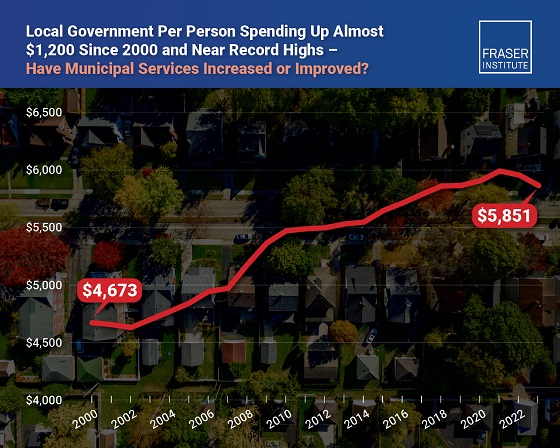
Business2 days agoMunicipal government per-person spending in Canada hit near record levels
-

 Business2 days ago
Business2 days agoA new federal bureaucracy will not deliver the affordable housing Canadians need






