Brownstone Institute
The Vaccine Was “95% Effective” How?

From the Brownstone Institute
BY
The 1840 Treaty of Waitangi between the British Crown and Maori chiefs was a landmark event in the history of New Zealand. Drafted in English, a Maori translation was prepared, ostensibly to ensure that Maori could have an accurate understanding of the terms. In retrospect, it is less clear that a meeting of the minds was intended:
The English and Māori texts differ. As some words in the English treaty did not translate directly into the written Māori language of the time, the Māori text is not a literal translation of the English text. It has been claimed that Henry Williams, the missionary entrusted with translating the treaty from English, was fluent in Māori and that far from being a poor translator he had in fact carefully crafted both versions to make each palatable to both parties without either noticing inherent contradictions.
“The covid vaccine is 95% effective” is a contemporary Treaty of Waitangi. The original is in the language of clinical trials. It was never translated. The public interpreted this phrase in their native language, normal English. What Pfizer said and what the public heard were quite different. The public would have been far more skeptical of these products had the clinical trial results been translated into normal English.
What we need is a proper translation and an explanation of how miscommunication happened.
The Injections Did Not Stop Infection
By now, everyone knows that the Pfizer and Moderna products did not stop people from getting Covid. Covid disease has mowed a wide strip through the double and triple-masked talking heads who told everyone that the shots would make them immune.
What is less well known is that:
- The products were never expected to stop infection or transmission.
- The clinical trials did not test for their ability to do so.
A clinical trial is designed to test a drug for effectiveness, which is strictly defined by one or more endpoints. An endpoint is a measurable outcome that can be assessed for each participant. With that in mind, prevention of infection was not an endpoint of the BioNTech/Pfizer injection clinical trials. And, this was known in 2020 before the products were approved for emergency use and distributed to the public starting in 2021.
In this New England Journal of Medicine research summary, Safety and Efficacy of the BNT162b2 mRNA Covid-19 Vaccine, under Limitations and Remaining Questions, we find that “whether the vaccine protects against asymptomatic infection and transmission to unvaccinated persons” remains unanswered by the clinical trial.
What did the clinical trial test for, if not the ability of the mRNA vaccine to stop transmission and/or infection? The trial was designed to test the ability of the injections to prevent “symptomatic Covid 19 cases” defined as one or more of a number symptoms and a positive test (see page 7 of the supplementary appendix for details).
@pfizer tweeted in Jan 2021 that stopping transmission was their “highest priority”. Their product does not do that, nor did the tweet make a claim that it did so. But it was their highest priority nonetheless. That, and getting as many people injected as possible.

Failure to Prevent Infection Was Known Before the Rollout
In October 2022, a Pfizer executive testified to an EU body that Pfizer had not tested the ability of the vaccine to stop transmission. This story was shocking to some and generated accusations that Pfizer had lied about the capabilities of the shots. But this information had been available since the trial results were released early in 2021. Pfizer had already been criticized for this.
Dr William A Haseltine PhD, wrote in Forbes in September 2020:
What would a normal vaccine trial look like?
One of the more immediate questions a trial needs to answer is whether a vaccine prevents infection. If someone takes this vaccine, are they far less likely to become infected with the virus? These trials all clearly focus on eliminating symptoms of Covid-19, and not infections themselves. Asymptomatic infection is listed as a secondary objective in these trials when they should be of critical importance.
On October 21, 2020 the editor of the BMJ (British Medical Journal) Peter Doshi asked:
Will covid-19 vaccines save lives? Current trials aren’t designed to tell us
Peter Hotez, dean of the National School of Tropical Medicine at Baylor College of Medicine in Houston, said, “Ideally, you want an antiviral vaccine to do two things . . . first, reduce the likelihood you will get severely ill and go to the hospital, and two, prevent infection and therefore interrupt disease transmission.”
Yet the current phase III trials are not actually set up to prove either. None of the trials currently underway are designed to detect a reduction in any serious outcome such as hospital admissions, use of intensive care, or deaths. Nor are the vaccines being studied to determine whether they can interrupt transmission of the virus….
Is It Even a Vaccine?
A vaccine that prevents infection is known as “neutralizing” or “sterilizing”. I am a software engineer with no training in medicine, pharmacology or clinical trials. I consider myself a good barometer of what the average untrained person would think about such things. Prior to 2021 I had thought that immunity was a necessary condition for a drug to earn the title of “vaccine”. If anyone had asked me, I would have told them that the Covid injections were a treatment, not a vaccine.
The Wikipedia article about vaccines (Mar 5 2023) aligns with my untrained understanding:
A vaccine is a biological preparation that provides active acquired immunity to a particular infectious or malignant disease. … A vaccine typically contains an agent that resembles a disease-causing microorganism and is often made from weakened or killed forms of the microbe, its toxins, or one of its surface proteins. The agent stimulates the body’s immune system to recognize the agent as a threat, destroy it, and to further recognize and destroy any of the microorganisms associated with that agent that it may encounter in the future.
Cornell Law provides the following legal definition of vaccine, sourcing 26 USC § 4132(a)(2), which is consistent with the above:
The term “vaccine” means any substance designed to be administered to a human being for the prevention of 1 or more diseases.
The definition published by the CDC prior to 2021 said much the same. But the CDC website changed the definition on or after August 2021. The older version found on the internet archive is here (emphasis added):
Immunity: Protection from an infectious disease. If you are immune to a disease, you can be exposed to it without becoming infected.
Vaccine: A product that stimulates a person’s immune system to produce immunity to a specific disease, protecting the person from that disease.
Here is the new version (emphasis added):
Vaccine: A preparation that is used to stimulate the body’s immune response against diseases.
The earlier pair of definitions is quite easy to understand. The latter, much more difficult. What exactly is a “preparation”? Does a vaccine stimulate the body or only prepare the body? What is or is not a vaccine according to the new definition?
While the CDC may think that they can change the meanings of words whenever they like, public memory retains the original meaning. The assumption of immunity permeates almost all non-expert level discussion of vaccines. A web search for “why are vaccines good” shows results that assume or imply immunity.
Even the CDC did not finish the job of memory-holing the old language. On the very same CDC website, under 5 Reasons It Is Important for Adults to Get Vaccinated, we read “By getting vaccinated, you can protect yourself and also avoid spreading preventable diseases to other people in your community.” And then, “Vaccines Can Prevent Serious Illness”.
The timing of the CDC’s edit suggests to me that prior to 2021, the CDC had the same understanding of vaccines as I do. I believe that they wanted a new definition because they knew that the products being developed at warp speed were not vaccines in the original sense of the word. And it was important that those products be called “vaccines” for reasons that I will explain later. This incident brings to mind a meme that I no longer have a link to. captioned: “We changed what ‘definition’ means so you can’t say that we redefined anything.”
What Does “95% Effective” Mean?
The “95% effective” message was repeated in nearly all reporting on the clinical trials. But the question, “effective at doing what?” was rarely asked. To answer this requires walking down the links of a chain of terminology from the world of clinical trials.
The first link in the chain is “risk”. Risk is the probability of a bad outcome. These are assumed to happen randomly within a group. A clinical trial must define in advance the bad outcomes that the drug intends to avoid. The next link is “endpoint”. Each distinct bad outcome is an “endpoint”. The trial compares the endpoints between a control group who did not take the drug and a test group, who did.
The purpose of a clinical trial is to determine the ability of a drug to reduce risk. A drug that reduces risk is “effective”. There are two ways of quantifying risk reduction. From the NIH glossary:
Absolute risk reduction (ARR) or risk difference
the difference in the incidence of poor outcomes between the intervention group of a study and the control group. For example, if 20 per cent of people die in the intervention group and 30 per cent in the control group, the ARR is 10 per cent (30–20 per cent).
Relative risk (RR)
the rate (risk) of poor outcomes in the intervention group divided by the rate of poor outcomes in the control group. For example, if the rate of poor outcomes is 20 per cent in the intervention group and 30 per cent in the control group, the relative risk is 0.67 (20 per cent divided by 30 per cent).
The difference between the ARR and RR (also known as “RRR”, to align with ARR) is in the denominator. The ARR divides by the number of participants in one of the groups. The RRR divides by the number of people with bad outcomes in the control group – a necessarily much smaller number.
The ARR is the number most relevant for a drug – such as the Pfizer injections – that was to be given to everyone. But the RRR is the preferred method of presentation for pharma when they want to exaggerate the effectiveness of a drug because it will always be a much larger number. Would you take a drug that could reduce the incidence of a rare disease by 50%? From 10 per 1 million to 5 per 1 million is an 50% RRR and an 0.0005% ARR.
The 95% figure cited for the covid injections is the relative risk. The absolute risk reduction was 0.84%. In a slide deck from the Canadian Covid Care Alliance(CCCA), slide 11 shows how the 91% was achieved (it is 91%, not 95%, because the it refers to an earlier version of the study):

The research paper COVID-19 vaccine efficacy and effectiveness—the elephant (not) in the room puts the ARR in the 1% range. The CCCA slide deck gives an ARR of 0.84%, though it is not clear how they reached this number, based on the other numbers in their slides.
A clinical trial finding of a 1% ARR means that 99% of the people who take the drug either did not experience the condition that the drug treats, or they did experience it, but were not helped by the drug. The 1% both had the condition and were helped by the drug. Another way of saying this is the Number Needed to Treat (NNT). NNT is the reciprocal of the ARR and is the number of people who must take the drug to help one person reach the endpoint. An ARR of 1% corresponds to an NNT of 100 people.
We can now answer the question of the meaning of vaccine effectiveness. The endpoint of the trial was a severe confirmed case of covid at least 7 days after the second dose. This endpoint requires the participant in the trial to have covid symptoms and a positive covid test. “95% effective” means that 95% of the patients who had Covid symptoms and a positive test were in the control group. Five percent were in the test group.
Here’s what “95% effective” did not mean: if you take the shots, then you will have a 95% lower chance of getting covid. But that is how most people understood it because that is what the words mean in normal English.
Then the Lying Started
Once the public had their hopes raised by the false translation of the “95% effective” message, the pandemic-industrial-complex went into high gear to amplify it. They stated the incorrect message loudly, frequently, and as if it were fact. The injections would – with 100% certainty (perhaps 200%) – protect you from infection. Many of the people who said this were doctors or scientific researchers who must have understood how to interpret clinical trials.
Here are some choice quotes that did not age well:
- “You’re not going to get Covid if you have these vaccinations.” Joe Biden, CNN Town Hall July 2021
- “Now we know that the vaccines work well enough that the virus stops with every vaccinated person. A vaccinated person gets exposed to the virus, the virus does not infect them, the virus cannot then use that person to go anywhere else,” she added with a shrug. “It cannot use a vaccinated person as a host to go get more people. [Vaccines] will get us to the end of this.” – Rachel Maddow, March 2021
- “When people are vaccinated they can feel safe that they won’t get infected, whether they’re outdoors or indoors.” – Dr. Anthony Fauci, May 2021(outdoors: seriously?)
- “Vaccination against COVID-19 prevents breakthrough infections, Stanford researchers find.” – Stanford Medicine, July 2021
- Vaccinated people become “dead ends” for the virus – Anthony Fauci, May 2021
Demonizing the Unvaxxed
The public has consistently over-estimated the infection fatality rate of Covid. Some even believed the fatality rate to be above 10%. They believed that we were in great danger. They also believed that the “95% effective” vaccine would bring the pandemic to a quick end, once everyone had taken it. Anyone who refused to do so was therefore risking not only their own life, but everybody else’s as well.
Dr Anthony Fauci estimated herd immunity would emerge when around 60% of the population had taken the vaccine … or perhaps 70, 80, no wait … 85%. Or maybe 100% (which would include large numbers who already had natural immunity). Bill Gates extended that to everyone on earth.
The narrative then turned to demonization of those who refused to submit to vaccine coercion. The selfish anti-social behavior of the anti-vaxxers with their stubborn attachment to “free dumb” that was keeping everyone locked indoors and forcing us all to wear diapers on our faces. Yale University behavioral researchers tested messaging strategies to determine whether shame, embarrassment or fear was most effective.
President Biden said that we the nation was experiencing a “pandemic of the unvaccinated”. Later, Biden ominoulsy warned the unvaccinated that he had been waiting a long time for them to get injected, but “our patience is wearing thin”. In December of 2021 the White House issued a cheery year end greeting to the vaccinated. The unvaccinated, on the other hand, were “looking at a winter of severe illness and death.” Merry Christmas.
Even South Park, which I consider a reliable source of contrarian political opinion, ran a storyline set in the year 2050 in which every single character had to be vaccinated for the 30-year pandemic to end. This episode featured one lone holdout who would not get vaccinated due to a crustacean allergy i.e. for “shellfish reasons”. This gag took aim at people who considered the vaccine to be a violation of body autonomy, and those who objected to components used in its development for religious reasons, thereby scoring a “two for one”.
Volumes can, and will, be written about the intense onslaught of propaganda aimed at getting two needles in every deltoid. I will provide one more example that represents no more than the median level of insanity; plenty of people called for the same or worse. @ClayTravis, in February 2023, tweeted the results of a Rasmussen poll from 2022:
Last January 60% of Democrats wanted to lock everyone who didn’t get the covid shot in their houses. Over 40% of Democrats wanted those who rejected the covid shot sent to quarantine camps. Over 40% also wanted anyone who criticized the covid shot fined & imprisoned. Over a quarter wanted those who didn’t get the covid shot to have their kids seized.
While there were many agendas driving the madness, the Treaty of Waitangi effect was a critical part in carrying it out. If the message had been that “everyone is going to get exposed to covid – injected or not”, then it could not have happened. The misunderstanding convinced the public that mass vaccination would stop the pandemic; and that the holdouts were prolonging it. Without this belief, none of the coercion made any sense: employment mandates, school mandates, quarantine camps, or vaccine passports. As the hysteria fades, the last remaining mandates are being dropped as the reality sinks in that the shots do not stop the spread.
Welcome to Waitangi World. I hope that you have a pleasant stay.
Brownstone Institute
Bizarre Decisions about Nicotine Pouches Lead to the Wrong Products on Shelves

From the Brownstone Institute
A walk through a dozen convenience stores in Montgomery County, Pennsylvania, says a lot about how US nicotine policy actually works. Only about one in eight nicotine-pouch products for sale is legal. The rest are unauthorized—but they’re not all the same. Some are brightly branded, with uncertain ingredients, not approved by any Western regulator, and clearly aimed at impulse buyers. Others—like Sweden’s NOAT—are the opposite: muted, well-made, adult-oriented, and already approved for sale in Europe.
Yet in the United States, NOAT has been told to stop selling. In September 2025, the Food and Drug Administration (FDA) issued the company a warning letter for offering nicotine pouches without marketing authorization. That might make sense if the products were dangerous, but they appear to be among the safest on the market: mild flavors, low nicotine levels, and recyclable paper packaging. In Europe, regulators consider them acceptable. In America, they’re banned. The decision looks, at best, strange—and possibly arbitrary.
What the Market Shows
My October 2025 audit was straightforward. I visited twelve stores and recorded every distinct pouch product visible for sale at the counter. If the item matched one of the twenty ZYN products that the FDA authorized in January, it was counted as legal. Everything else was counted as illegal.
Two of the stores told me they had recently received FDA letters and had already removed most illegal stock. The other ten stores were still dominated by unauthorized products—more than 93 percent of what was on display. Across all twelve locations, about 12 percent of products were legal ZYN, and about 88 percent were not.
The illegal share wasn’t uniform. Many of the unauthorized products were clearly high-nicotine imports with flashy names like Loop, Velo, and Zimo. These products may be fine, but some are probably high in contaminants, and a few often with very high nicotine levels. Others were subdued, plainly meant for adult users. NOAT was a good example of that second group: simple packaging, oat-based filler, restrained flavoring, and branding that makes no effort to look “cool.” It’s the kind of product any regulator serious about harm reduction would welcome.
Enforcement Works
To the FDA’s credit, enforcement does make a difference. The two stores that received official letters quickly pulled their illegal stock. That mirrors the agency’s broader efforts this year: new import alerts to detain unauthorized tobacco products at the border (see also Import Alert 98-06), and hundreds of warning letters to retailers, importers, and distributors.
But effective enforcement can’t solve a supply problem. The list of legal nicotine-pouch products is still extremely short—only a narrow range of ZYN items. Adults who want more variety, or stores that want to meet that demand, inevitably turn to gray-market suppliers. The more limited the legal catalog, the more the illegal market thrives.
Why the NOAT Decision Appears Bizarre
The FDA’s own actions make the situation hard to explain. In January 2025, it authorized twenty ZYN products after finding that they contained far fewer harmful chemicals than cigarettes and could help adult smokers switch. That was progress. But nine months later, the FDA has approved nothing else—while sending a warning letter to NOAT, arguably the least youth-oriented pouch line in the world.
The outcome is bad for legal sellers and public health. ZYN is legal; a handful of clearly risky, high-nicotine imports continue to circulate; and a mild, adult-market brand that meets European safety and labeling rules is banned. Officially, NOAT’s problem is procedural—it lacks a marketing order. But in practical terms, the FDA is punishing the very design choices it claims to value: simplicity, low appeal to minors, and clean ingredients.
This approach also ignores the differences in actual risk. Studies consistently show that nicotine pouches have far fewer toxins than cigarettes and far less variability than many vapes. The biggest pouch concerns are uneven nicotine levels and occasional traces of tobacco-specific nitrosamines, depending on manufacturing quality. The serious contamination issues—heavy metals and inconsistent dosage—belong mostly to disposable vapes, particularly the flood of unregulated imports from China. Treating all “unauthorized” products as equally bad blurs those distinctions and undermines proportional enforcement.
A Better Balance: Enforce Upstream, Widen the Legal Path
My small Montgomery County survey suggests a simple formula for improvement.
First, keep enforcement targeted and focused on suppliers, not just clerks. Warning letters clearly change behavior at the store level, but the biggest impact will come from auditing distributors and importers, and stopping bad shipments before they reach retail shelves.
Second, make compliance easy. A single-page list of authorized nicotine-pouch products—currently the twenty approved ZYN items—should be posted in every store and attached to distributor invoices. Point-of-sale systems can block barcodes for anything not on the list, and retailers could affirm, once a year, that they stock only approved items.
Third, widen the legal lane. The FDA launched a pilot program in September 2025 to speed review of new pouch applications. That program should spell out exactly what evidence is needed—chemical data, toxicology, nicotine release rates, and behavioral studies—and make timely decisions. If products like NOAT meet those standards, they should be authorized quickly. Legal competition among adult-oriented brands will crowd out the sketchy imports far faster than enforcement alone.
The Bottom Line
Enforcement matters, and the data show it works—where it happens. But the legal market is too narrow to protect consumers or encourage innovation. The current regime leaves a few ZYN products as lonely legal islands in a sea of gray-market pouches that range from sensible to reckless.
The FDA’s treatment of NOAT stands out as a case study in inconsistency: a quiet, adult-focused brand approved in Europe yet effectively banned in the US, while flashier and riskier options continue to slip through. That’s not a public-health victory; it’s a missed opportunity.
If the goal is to help adult smokers move to lower-risk products while keeping youth use low, the path forward is clear: enforce smartly, make compliance easy, and give good products a fair shot. Right now, we’re doing the first part well—but failing at the second and third. It’s time to fix that.
Addictions
The War on Commonsense Nicotine Regulation

From the Brownstone Institute
Cigarettes kill nearly half a million Americans each year. Everyone knows it, including the Food and Drug Administration. Yet while the most lethal nicotine product remains on sale in every gas station, the FDA continues to block or delay far safer alternatives.
Nicotine pouches—small, smokeless packets tucked under the lip—deliver nicotine without burning tobacco. They eliminate the tar, carbon monoxide, and carcinogens that make cigarettes so deadly. The logic of harm reduction couldn’t be clearer: if smokers can get nicotine without smoke, millions of lives could be saved.
Sweden has already proven the point. Through widespread use of snus and nicotine pouches, the country has cut daily smoking to about 5 percent, the lowest rate in Europe. Lung-cancer deaths are less than half the continental average. This “Swedish Experience” shows that when adults are given safer options, they switch voluntarily—no prohibition required.
In the United States, however, the FDA’s tobacco division has turned this logic on its head. Since Congress gave it sweeping authority in 2009, the agency has demanded that every new product undergo a Premarket Tobacco Product Application, or PMTA, proving it is “appropriate for the protection of public health.” That sounds reasonable until you see how the process works.
Manufacturers must spend millions on speculative modeling about how their products might affect every segment of society—smokers, nonsmokers, youth, and future generations—before they can even reach the market. Unsurprisingly, almost all PMTAs have been denied or shelved. Reduced-risk products sit in limbo while Marlboros and Newports remain untouched.
Only this January did the agency relent slightly, authorizing 20 ZYN nicotine-pouch products made by Swedish Match, now owned by Philip Morris. The FDA admitted the obvious: “The data show that these specific products are appropriate for the protection of public health.” The toxic-chemical levels were far lower than in cigarettes, and adult smokers were more likely to switch than teens were to start.
The decision should have been a turning point. Instead, it exposed the double standard. Other pouch makers—especially smaller firms from Sweden and the US, such as NOAT—remain locked out of the legal market even when their products meet the same technical standards.
The FDA’s inaction has created a black market dominated by unregulated imports, many from China. According to my own research, roughly 85 percent of pouches now sold in convenience stores are technically illegal.
The agency claims that this heavy-handed approach protects kids. But youth pouch use in the US remains very low—about 1.5 percent of high-school students according to the latest National Youth Tobacco Survey—while nearly 30 million American adults still smoke. Denying safer products to millions of addicted adults because a tiny fraction of teens might experiment is the opposite of public-health logic.
There’s a better path. The FDA should base its decisions on science, not fear. If a product dramatically reduces exposure to harmful chemicals, meets strict packaging and marketing standards, and enforces Tobacco 21 age verification, it should be allowed on the market. Population-level effects can be monitored afterward through real-world data on switching and youth use. That’s how drug and vaccine regulation already works.
Sweden’s evidence shows the results of a pragmatic approach: a near-smoke-free society achieved through consumer choice, not coercion. The FDA’s own approval of ZYN proves that such products can meet its legal standard for protecting public health. The next step is consistency—apply the same rules to everyone.
Combustion, not nicotine, is the killer. Until the FDA acts on that simple truth, it will keep protecting the cigarette industry it was supposed to regulate.
-
 Alberta9 hours ago
Alberta9 hours agoFrom Underdog to Top Broodmare
-

 armed forces2 days ago
armed forces2 days ago2025 Federal Budget: Veterans Are Bleeding for This Budget
-

 Alberta1 day ago
Alberta1 day agoAlberta and Ottawa ink landmark energy agreement
-
 Artificial Intelligence2 days ago
Artificial Intelligence2 days agoTrump’s New AI Focused ‘Manhattan Project’ Adds Pressure To Grid
-
 International1 day ago
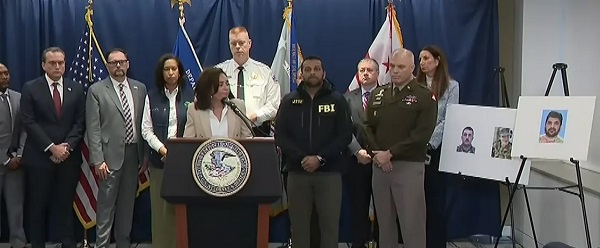
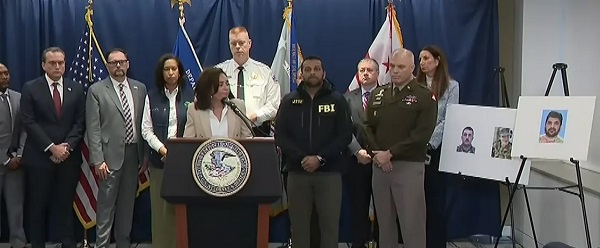
International1 day agoAfghan Ex–CIA Partner Accused in D.C. National Guard Ambush
-

 Carbon Tax1 day ago
Carbon Tax1 day agoCanadian energy policies undermine a century of North American integration
-

 International1 day ago
International1 day agoIdentities of wounded Guardsmen, each newly sworn in
-

 International2 days ago
International2 days agoTrump Admin Pulls Plug On Afghan Immigration Following National Guard Shooting










