COVID-19
COVID cases and hospitalizations down in Central Alberta for first time in two weeks.





COVID-19
Ontario man launches new challenge against province’s latest attempt to ban free expression on roadside billboards

The Justice Centre for Constitutional Freedoms announces that Ontario resident George Katerberg has launched a legal challenge against the Ontario Ministry of Transportation for banning roadside billboards with social or political messages. Mr. Katerberg believes that the Ministry’s policies go too far and undermine the freedom of expression of all Ontarians.
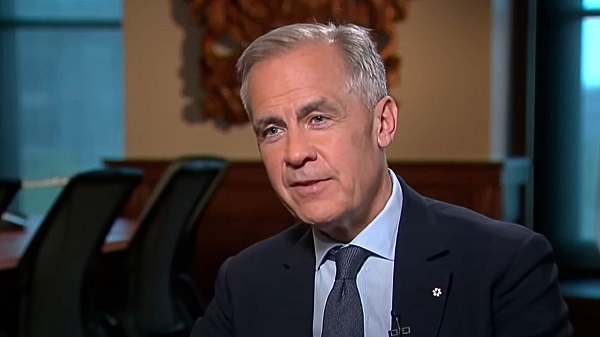
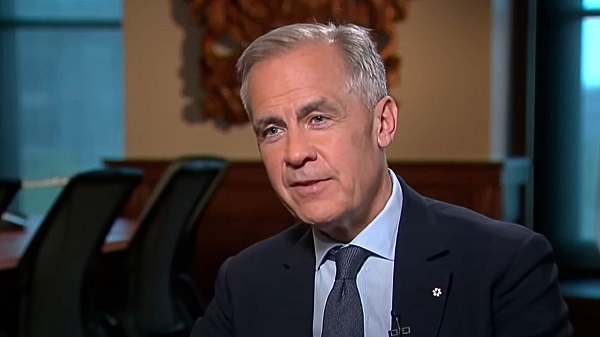
This case goes back to March 2024, when Mr. Katerberg, a retired HVAC technician, rented a billboard on Highway 17 near Thessalon, Ontario, that featured images of public health officials and politicians alongside a message critical of their statements about vaccines.
After the Ministry rejected his proposed billboard several times on the grounds it promoted hatred, a constitutional challenge was launched with lawyers provided by the Justice Centre. Mr. Katerberg’s lawyers argued that the Ministry’s position was unreasonable, and that it did not balance Charter rights with the purposes of relevant legislation.
The Ministry later admitted that the sign did not violate hate speech guidelines and agreed to reconsider erecting the billboard.
However, in April 2025, the Ministry quietly amended its policy manual to restrict signs along “bush highways” to those only promoting goods, services, or authorized community events.
The new guidelines are sweeping and comprehensive, barring any messaging that the Ministry claims could “demean, denigrate, or disparage one or more identifiable persons, groups of persons, firms, organizations, industrial or commercial activities, professions, entities, products or services…”
Relying on this new policy, the Ministry once again denied Mr. Katerberg’s revised billboard.
Constitutional lawyer Chris Fleury explains, “By amending the Highway Corridor Management Manual to effectively prohibit signage that promotes political and social causes, the Ministry of Transportation has turned Mr. Katerberg’s fight to raise his sign into a fight on behalf of all Ontarians who wish to express support for a political or social cause.”
No date has yet been assigned for a hearing on this matter.
COVID-19
New Peer-Reviewed Study Affirms COVID Vaccines Reduce Fertility

Here’s what the numbers reveal, and what it could mean for humanity
What was once dismissed as a “conspiracy theory” now has hard data behind it.
A new peer-reviewed study out of the Czech Republic has uncovered a disturbing trend: in 2022, women vaccinated against COVID-19 had 33% FEWER successful conceptions per 1,000 women compared to those who were unvaccinated.
A “successful conception” means a pregnancy that led to a live birth nine months later.
The study wasn’t small. It analyzed data from 1.3 million women aged 18 to 39.
Here’s what the numbers reveal, and what it could mean for humanity.
First, let’s talk about the study.
It was published by Manniche and colleagues in the International Journal of Risk & Safety in Medicine, a legitimate, peer-reviewed journal respected for its focus on patient safety and pharmacovigilance.
The study was conducted from January 2021 to December 2023 and examined 1.3 million women aged 18–39. By the end of 2021, approximately 70% of them had received at least one COVID-19 vaccination, with 96% of the vaccinated cohort having received either the Pfizer or Moderna vaccine.
By 2022, a stark difference was clear.
The vaccinated cohort averaged around 4 successful conceptions per 1,000 women per month.
That’s a staggering 33% LESS than the 6 per 1,000 seen in the unvaccinated group.
This means that for every 2 vaccinated women who successfully conceived and delivered a baby, 3 unvaccinated women did the same.
In 2022, unvaccinated women were 1.5 times MORE likely to have a successful conception.
Again, that’s a conception that led to a live birth nine months later.
The authors did not jump to the conclusion that their study proved causation. They cited that other factors may have played a role, such as self-selection bias
However, the researchers noted that self-selection bias does not explain the timing and scale of the observed drop in fertility.
Moreover, birth rates in the Czech Republic dropped from 1.83 per 1,000 women in 2021 to 1.37 in 2024, adding further evidence that the COVID-19 vaccines may be contributing to the decline in fertility.
That downward trend, the researchers argue, supports the hypothesis that something beyond individual decision-making may be affecting conception rates.
As such, they argue that the study’s results warrant a closer and more thorough examination of the impact of mass vaccination.
If this study holds true, and vaccinated women are really much less likely to have successful conceptions, the implications for humanity are massive.
Millions of babies could be missing each year as a result of COVID vaccination, and recent data from Europe and beyond already point to a deeply disturbing trend.
NOTE: Europe experienced a sharper decline in births than usual from 2021 to 2023.
Live births fell from 4.09 million in 2021 to 3.67 million in 2023, marking a 10.3% decline in just two years.
The new Czech study adds to growing evidence that COVID vaccines may be contributing to a dramatic decline in fertility, just as many feared all along.
As Elon Musk warns, “If there are no humans, there’s no humanity.”
Whether the shots are the cause or not, the trend is real—and it’s accelerating.
It’s time to stop dismissing the signals and start investigating the cause.
Thanks for reading. I hope this report gave you real value. This is a critically important topic that deserves attention.
If you appreciate my work and want to help keep it going, consider becoming a paid subscriber.
99% of readers get this content for free. But just $5/month from the 1% keeps it flowing for everyone else.
If this work matters to you, this is the best way to support it.
Be the 1% who makes it possible.
Catch the rest of today’s biggest headlines at VigilantFox.com.
-

 COVID-1910 hours ago
COVID-1910 hours agoOntario man launches new challenge against province’s latest attempt to ban free expression on roadside billboards
-

 Energy18 hours ago
Energy18 hours agoThis Canada Day, Celebrate Energy Renewal
-

 Business2 days ago
Business2 days agoWhile China Hacks Canada, B.C. Sends Them a Billion-Dollar Ship Building Contract
-

 Alberta1 day ago
Alberta1 day agoSo Alberta, what’s next?
-

 Alberta9 hours ago
Alberta9 hours agoAlberta Next Takes A Look At Alberta Provincial Police Force
-

 Bjorn Lomborg1 day ago
Bjorn Lomborg1 day agoThe Physics Behind The Spanish Blackout
-

 Alberta11 hours ago
Alberta11 hours agoCanadian Oil Sands Production Expected to Reach All-time Highs this Year Despite Lower Oil Prices
-
 Business13 hours ago
Business13 hours agoPotential For Abuse Embedded In Bill C-5

















