Health
WHO’s Global Digital Health Certification Network

With notes from the World Health Organization website, Dr. John Campbell explains the WHO’s Global Digital Health Certification Network. To see the WHO’s press release click here or scroll below the video where it is attached.
From the youtube channel of  Dr. John Campbell
Dr. John Campbell
Press release from the World Health Organization
The European Commission and WHO launch landmark digital health initiative to strengthen global health security
The World Health Organization (WHO) and European Commission have announced today the launch of a landmark digital health partnership.
In June 2023, WHO will take up the European Union (EU) system of digital COVID-19 certification to establish a global system that will help facilitate global mobility and protect citizens across the world from on-going and future health threats, including pandemics. This is the first building block of the WHO Global Digital Health Certification Network (GDHCN) that will develop a wide range of digital products to deliver better health for all.
“Building on the EU’s highly successful digital certification network, WHO aims to offer all WHO Member States access to an open-source digital health tool, which is based on the principles of equity, innovation, transparency and data protection and privacy,” said Dr Tedros Adhanom Ghebreyesus, WHO Director-General. “New digital health products in development aim to help people everywhere receive quality health services quickly and more effectively”.
Based on the EU Global Health Strategy and WHO Global strategy on digital health, the initiative follows the 30 November 2022 agreement between Commissioner Kyriakides and Dr Tedros to enhance strategic cooperation on global health issues. This further bolsters a robust multilateral system with WHO at its core, powered by a strong EU.
“This partnership is an important step for the digital action plan of the EU Global Health Strategy. By using European best practices we contribute to digital health standards and interoperability globally—to the benefit of those most in need. It is also a powerful example of how alignment between the EU and the WHO can deliver better health for all, in the EU and across the world. As the directing and coordinating authority on international health work, there is no better partner than the WHO to advance the work we started at the EU and further develop global digital health solutions,” said Stella Kyriakides, Commissioner for Health and Food Safety.
This partnership will include close collaboration in the development, management and implementation of the WHO GDHCN system, benefitting from the European Commission’s ample technical expertise in the field. A first step is to ensure that the current EU digital certificates continue to function effectively.
“With 80 countries and territories connected to the EU Digital COVID-19 Certificate, the EU has set a global standard. The EU certificate has not only been an important tool in our fight against the pandemic, but has also facilitated international travel and tourism. I am pleased that the WHO will build on the privacy-preserving principles and cutting-edge technology of the EU certificate to create a global tool against future pandemics,” added Thierry Breton, Commissioner for Internal Market.
A global WHO system building on EU legacy
One of the key elements in the European Union’s work against the COVID-19 pandemic has been digital COVID-19 certificates. To facilitate free movement within its borders, the EU swiftly established interoperable COVID-19 certificates (entitled ‘EU Digital COVID-19 Certificate’ or ‘EU DCC’). Based on open-source technologies and standards it allowed also for the connection of non-EU countries that issue certificates according to EU DCC specifications, becoming the most widely used solution around the world.
From the onset of the pandemic, WHO engaged with all WHO Regions to define overall guidelines for such certificates. To help strengthen global health preparedness in the face of growing health threats, WHO is establishing a global digital health certification network which builds upon the solid foundations of the EU DCC framework, principles and open technologies. With this collaboration, WHO will facilitate this process globally under its own structure with the aim to allow the world to benefit from convergence of digital certificates. This includes standard-setting and validation of digital signatures to prevent fraud. In doing so, WHO will not have access to any underlying personal data, which would continue to be the exclusive domain of governments.
The first building block of the global WHO system becomes operational in June 2023 and aims to be progressively developed in the coming months.
A long-term digital partnership to deliver better health for all
To facilitate the uptake of the EU DCC by WHO and contribute to its operation and further development, WHO and the European Commission have agreed to partner in digital health.
This partnership will work to technically develop the WHO system with a staged approach to cover additional use cases, which may include, for example, the digitisation of the International Certificate of Vaccination or Prophylaxis. Expanding such digital solutions will be essential to deliver better health for citizens across the globe.
This cooperation is based on the shared values and principles of transparency and openness, inclusiveness, accountability, data protection and privacy, security, scalability at a global level, and equity. The WHO and the European Commission will work together to encourage maximum global uptake and participation. Particular attention will be paid to equitable opportunities for the participation by those most in need: low and middle-income countries.
Dr. John Campbell’s Presentation notes:
WHO’s Global Digital Health Certification Network https://www.who.int/initiatives/globa…
WHO has established the Global Digital Health Certification Network (GDHCN). Open-source platform, built on robust & transparent standards, that establishes the first building block of digital public health infrastructure, for developing a wide range of digital products, for strengthening pandemic preparedness
Background Member States used digital COVID-19 test and vaccine certificates As the directing and coordinating authority on international health work, at the onset of the pandemic, WHO engaged with all WHO Regions to define overall guidance for such certificates and published the Digital Documentation of COVID-19 Certificates
https://www.who.int/publications/i/it… https://www.who.int/publications/i/it… there is a recognition of an existing gap, and continued need for a global mechanism, that can support bilateral verification of the provenance of health documents
The GDHCN may include Digitisation of the International Certificate of Vaccination or Prophylaxis, verification of prescriptions across borders
International Patient Summary Verification of vaccination certificates within and across borders Certification of public health professionals (through WHO Academy) Expanding such digital solutions will be essential to deliver better health for people across the globe.
The GDHCN has been designed to be interoperable with other existing regional networks EU-WHO digital partnership https://www.who.int/news/item/05-06-2… ![]() • LIVE: WHO and @EU… https://commission.europa.eu/strategy… WHO and the European Commission have agreed to partner in digital health.
• LIVE: WHO and @EU… https://commission.europa.eu/strategy… WHO and the European Commission have agreed to partner in digital health.
This partnership will work to technically develop the WHO system with a staged approach to cover additional use cases, In June 2023, WHO will take up the European Union (EU) system of digital COVID-19 certification to establish a global system, that will help facilitate global mobility
This is the first building block of the WHO Global Digital Health Certification Network (GDHCN)
Dr Tedros Adhanom Ghebreyesus WHO aims to offer all WHO Member States access, On the principles of equity, innovation, transparency and data protection and privacy Stella Kyriakides, Commissioner for Health and Food Safety
This partnership is an important step for the digital action plan of the EU Global Health Strategy, we contribute to digital health standards and interoperability globally
Thierry Breton, Commissioner for Internal Market The EU certificate … has also facilitated international travel and tourism I am pleased that the WHO will build on …. cutting-edge technology … to create a global tool against future pandemics
One of the key elements in the European Union’s work against the COVID-19 pandemic has been digital COVID-19 certificates. WHO will facilitate this process globally under its own structure … allow the world to benefit from convergence of digital certificates. Expanding such digital solutions will be essential to deliver better health for citizens across the globe.
The WHO and the European Commission will work together to encourage maximum global uptake and participation.
Business
RFK Jr. says Hep B vaccine is linked to 1,135% higher autism rate

From LifeSiteNews
By Matt Lamb
They got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data
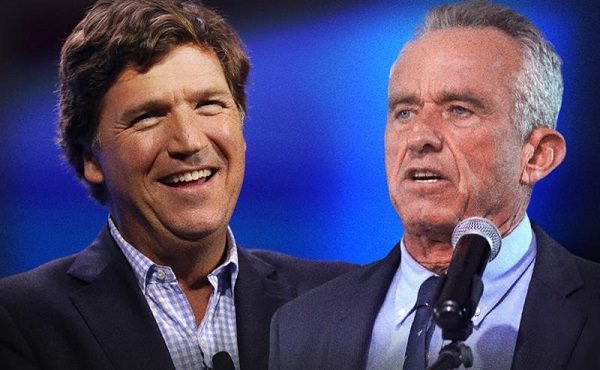
The Centers for Disease Control and Prevention (CDC) found newborn babies who received the Hepatitis B vaccine had 1,135-percent higher autism rates than those who did not or received it later in life, Robert F. Kennedy Jr. told Tucker Carlson recently. However, the CDC practiced “trickery” in its studies on autism so as not to implicate vaccines, Kennedy said.
RFK Jr., who is the current Secretary of Health and Human Services, said the CDC buried the results by manipulating the data. Kennedy has pledged to find the causes of autism, with a particular focus on the role vaccines may play in the rise in rates in the past decades.
The Hepatitis B shot is required by nearly every state in the U.S. for children to attend school, day care, or both. The CDC recommends the jab for all babies at birth, regardless of whether their mother has Hep B, which is easily diagnosable and commonly spread through sexual activity, piercings, and tattoos.
“They kept the study secret and then they manipulated it through five different iterations to try to bury the link and we know how they did it – they got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data,” Kennedy told Carlson for an episode of the commentator’s podcast. “And they did a lot of other tricks and all of those studies were the subject of those kind of that kind of trickery.”
But now, Kennedy said, the CDC will be conducting real and honest scientific research that follows the highest standards of evidence.
“We’re going to do real science,” Kennedy said. “We’re going to make the databases public for the first time.”
He said the CDC will be compiling records from variety of sources to allow researchers to do better studies on vaccines.
“We’re going to make this data available for independent scientists so everybody can look at it,” the HHS secretary said.
— Matt Lamb (@MattLamb22) July 1, 2025
Health and Human Services also said it has put out grant requests for scientists who want to study the issue further.
Kennedy reiterated that by September there will be some initial insights and further information will come within the next six months.
Carlson asked if the answers would “differ from status quo kind of thinking.”
“I think they will,” Kennedy said. He continued on to say that people “need to stop trusting the experts.”
“We were told at the beginning of COVID ‘don’t look at any data yourself, don’t do any investigation yourself, just trust the experts,”‘ he said.
In a democracy, Kennedy said, we have the “obligation” to “do our own research.”
“That’s the way it should be done,” Kennedy said.
He also reiterated that HHS will return to “gold standard science” and publish the results so everyone can review them.
International
RFK Jr. tells Tucker how Big Pharma uses ‘perverse incentives’ to get vaccines approved
From LifeSiteNews
By Matt Lamb
Kennedy defended his decision to fire all 17 members of the Advisory Committee on Immunization Practices, which he decried as a tool used to “rubber stamp” vaccines.
The vaccine approval process is a “bundle of perverse incentives” since pharmaceutical companies stand to make billions of dollars in revenue from it, Secretary of Health and Human Services Robert F. Kennedy Jr. told Tucker Carlson recently.
Kennedy appeared on Carlson’s show yesterday to discuss a variety of issues, including the potential link between autism and vaccines and his overhauling of the vaccine advisory committee at the Centers for Disease Control and Prevention last month.
Twenty years ago, Bobby Kennedy was exiled from polite society for suggesting a link between autism and vaccines. Now he’s a cabinet secretary, and still saying it.
(0:00) The Organized Opposition to RFK’s Mission
(6:46) Uncovering the Reason for Skyrocketing Rates of Autism… pic.twitter.com/g8T8te3kNC— Tucker Carlson (@TuckerCarlson) June 30, 2025
Kennedy began by explaining that Big Pharma has been targeting academic journals to ensure its products receive favorable reviews.
“The journals won’t publish anything critical of vaccines … there’s so much pressure on them. They’re funded by pharmaceutical companies, and they’ll lose advertising and revenue from reprints,” Kennedy said.
Kennedy then noted that Big Pharma will “pay to get something published in these journals,” before accusing industry leaders of pushing drugs on doctors and of hiring “mercenary scientists” to manipulate data until their product is deemed safe and effective.
The entire complex is broken due to the “perverse incentives,” he lamented.
Later in the interview, Kennedy defended his decision to fire all 17 members of the Advisory Committee on Immunization Practices (ACIP) in June, which he decried as a mere tool to “rubber stamp” vaccines.
It served as “a sock puppet for the industry that it was supposed to regulate,” Kennedy exclaimed, citing conflicts of interest for the overwhelming majority of its board members.
This sort of “agency capture” explains the lucrative nature of vaccines, he added.
— Matt Lamb (@MattLamb22) July 1, 2025
Kennedy then summarized the “perverse” process as follows:
First of all, the federal government often times actually designs the vaccine, [the National Institutes of Health] would design it, would hand it over to the pharmaceutical company. The pharmaceutical company then runs it … first through [the] FDA, then through [the] ACIP, and gets it recommended.
If you can get that recommendation you now got a billion dollars in — at least — revenues by the end of the year, every year, forever. So, there was a gold rush to add new vaccines to the schedule and ACIP never turned away a single vaccine … that came to them they recommended, and a lot of these vaccines are for diseases that are not even casually contagious.
Kennedy further pointed to the Hepatitis B shot for newborns as an example of how the industry has been corrupted.
In 1999, the CDC “looked at children who had received the hepatitis vaccine within the first 30 days of life and compared those children to children who had received the vaccine later — or not at all. And they found an 1,135% elevated risk of autism among the vaccinated children. It shocked them. They kept the study secret and manipulated it through five different iterations to try to bury the link,” he said.
“We want to protect public health,” Kennedy explained, but “these vaccines … can cause chronic disease, chronic injuries that last a lifetime.”
-

 COVID-191 day ago
COVID-191 day agoOntario man launches new challenge against province’s latest attempt to ban free expression on roadside billboards
-

 Energy2 days ago
Energy2 days agoThis Canada Day, Celebrate Energy Renewal
-

 COVID-1912 hours ago
COVID-1912 hours agoNew Peer-Reviewed Study Affirms COVID Vaccines Reduce Fertility
-

 Business8 hours ago
Business8 hours agoOttawa Funded the China Ferry Deal—Then Pretended to Oppose It
-

 Alberta1 day ago
Alberta1 day agoAlberta Next Takes A Look At Alberta Provincial Police Force
-

 MAiD10 hours ago
MAiD10 hours agoCanada’s euthanasia regime is not health care, but a death machine for the unwanted
-

 Alberta1 day ago
Alberta1 day agoCanadian Oil Sands Production Expected to Reach All-time Highs this Year Despite Lower Oil Prices
-

 Alberta11 hours ago
Alberta11 hours agoThe permanent CO2 storage site at the end of the Alberta Carbon Trunk Line is just getting started





