Health
National pharmacare – might it be a pig in a poke?

From the Macdonald Laurier Institute
By Nigel Rawson and John Adams for Inside Policy
No Canadian should have to choose between paying for medicines and paying for rent or food. National pharmacare has been proposed as a remedy to this situation.
“When will Canada have national pharmacare?” asks the author of a recent article in the British Medical Journal (BMJ). Better questions are: will Canadian pharmacare be the system many Canadians hope for? Or, might it turn out to be skimpy coverage akin to minimum wage laws?
In its 2024 budget document, the federal government proposed providing $1.5 billion over five years to support the launch of national pharmacare for “universal, single-payer coverage for a number of contraception and diabetes medications.” This has been hailed as a “big day for pharmacare” by some labour unions, patients and others, including the author of the BMJ article who said that national pharmacare should be expanded to cover all medication needs beginning with the most commonly-prescribed, clinically-important “essential medicines.”
In its budget, the government stated “coverage of contraceptives will mean that nine million women in Canada will have better access to contraception” and “improving access to diabetes medications will help improve the health of 3.7 million Canadians with diabetes.” Why not salute such affable, motherhood and apple pie, sentiments? The devil is in the details.
The plan does not cover new drugs for diabetes, such as Ozempic, Rybelsus, Wegovy, Mounjaro or Zepbound, all based on innovative GLP-1 agonists, where evidence is building for cardiovascular and weight loss benefits. This limited rollout seems based on cheap, older medicines, which can be less effective for some with diabetes.
The federal government has also consistently under-estimated the cost of national proposals such as pharmacare – not to mention other promises. In their 2019 election platform, the Liberals promised $6 billion for national pharmacare (the NDP promised $10 billion). Keen analysis shows that even these expansive amounts would be woefully inadequate to fund a full national pharmacare plan. This makes the $300 million a year actually proposed by the Liberals’ look like the skimpy window-dressing that it is.
National pharmacare, based on the most comprehensive existing public drug plan (Quebec’s), would cost much more. In 2017, using optimistic assumptions, the Parliamentary Budget Officer (PBO) estimated the cost for a national plan based on Quebec’s experience to be $19.3 billion a year. With more appropriate assumptions, the Canadian Health Policy Institute estimated $26.2 billion. In June 2019, the federal government’s own Advisory Council on the Implementation of National Pharmacare put the cost at $40 billion, while a few months later, the tax consulting company RSM Canada projected $48.3 to $52.5 billion per year. Five years later, costs no doubt have soared.
Even with these staggering cost a program based on matching Quebec’s drug plan at the national level would fail to provide anywhere near the level of coverage already provided to the almost two-thirds of Canadians who have private drug insurance, including many in unionized jobs. Are they willing to sacrifice their superior coverage, especially of innovative brand-name medicines, for a program covering only “essential medicines”? Put another way, are Canadians and their unions prepared to settle for the equivalent of a minimum wage or minimum benefits?
The PBO has estimated the cost of coverage of a range of contraceptives and diabetes medicines as $1.9 billion over five years, which is more than the $1.5 billion provided in the budget. However, this figure is based on an assumption that the new program would only cover Canadians who currently do not have public or private drug plan insurance, those who currently do not fill their prescriptions due to cost related reasons, and the out-of-pocket part of prescription costs for Canadians who have public or private drug plan coverage. This is major guesswork because existing public and private drug plans may see the new federal program as an opportunity to reduce their costs by requiring their beneficiaries to use the new program. If this occurs, the national pharmacare costs to the federal government, even for the limited role out of diabetes and contraceptives, would soar to an estimated $5.7 billion, according to the PBO.
Our governments are not known for accurate estimates of the costs of new programs. One has only to remember the Phoenix pay system and the ArriveCAN costs. In 2017, the Government of Ontario estimated $465 million per year to extend drug coverage to every resident under the age of 25 years. What happened? Introduced in 2018, prescriptions rose by 290% and drug expenditure increased to $839 million – almost double the guesstimate. In 2019, the provincial government back peddled and modified the program to cover only people not already insured by a private plan.
Although we believe governments should facilitate access to necessary medicines for Canadians who cannot afford their medicines, this does not require national pharmacare and a growing bureaucracy. Exempting lower-income Canadians from copayments and premiums required by provincial programs, as British Columbia has done, and removing the requirement to pay for all drugs up to a deductible would allow these Canadians access sooner, more simply, and more effectively.
Moreover, it isn’t just lower-income Canadians who want help with unmet medicine needs. Canadians who need access to drugs for diseases that are difficult to treat and can cost hundreds of thousands of dollars per year also require assistance. Few Canadians whether they have low, medium or high incomes can afford these prices without government or private insurance. Private insurers often refuse to cover these drugs.
The Liberals provided a separate $1.5 billion over three years for drugs for rare disorders, but no province or territory has signed a bilateral agreement with the federal government for these drugs and no patient has received benefit through this program. Even if they did, the $500 million per year would not go far towards the actual costs. There is at least a zero missing in the federal contribution, as the projected cost of public spending on rare disease medicines by 2025 is more than threefold what Ottawa has budgeted.
Expensive drugs for cancer and rare disorders are just as essential as basic medicines for cardiovascular diseases, diabetes, birth control, and many other common conditions. If a costly medicine will allow a person with a life-shortening disease to live longer or one with a disorder that will be severely disabling left untreated to have an improved quality of life and be a productive taxpayer, it too should be regarded as essential.
The Liberals and NDP are working to stampede the bill to introduce the pharmacare program (Bill C-64) through the legislative process. This includes inviting witnesses over the first long weekend of summer, when many Canadians are away, to appear before the parliamentary Standing Committee on Health three days later.
Too much is unknown about what will be covered (will newer drugs be covered or only older, cheaper medicines?), who will be eligible for coverage (all appropriate Canadians regardless of existing coverage or only those with no present coverage?), and what the real cost will be, including whether a new program focusing on older, cheaper drugs will deter drug developers from launching novel medicines for unmet needs in Canada.
This Bill as it stands is such a power grab that, if passed, the federal Health Minister never has to come back to Parliament for review, oversight or another tranche of legal authority, it would empower the Cabinet to make rules and regulations without parliamentary scrutiny.
A lot is at stake for Canadians, especially for patients and their doctors. Prescription medicines are of critical importance to treating many diseases. National pharmacare must not only allow low-income residents to access purported “essential medicines” but also ensure that patients who need specialized drugs, especially higher-cost innovative cell and genetic therapies that may be the only effective treatment for their disorder, are not ignored. Canadians should be careful what they wish for. They may receive less than they anticipate, and, in fact, many Canadians may be worse off despite the increase in public spending. Time to look under the hood and kick the tires.
Nigel Rawson is a senior fellow with the Macdonald-Laurier Institute.
John Adams is co-founder and CEO of Canadian PKU and Allied Disorders Inc., a senior fellow with the Macdonald-Laurier Institute and volunteer board chair of Best Medicines Coalition.
Focal Points
Pharma Bombshell: President Trump Orders Complete Childhood Vaccine Schedule Review

After unnecessary hepatitis B vaccine dropped for 3.6 million annual healthy live births, POTUS calls for entire ACIP schedule to better align with other countries
After the CDC ACIP panel voted 8-3 to drop the hepatitis B vaccine for millions of healthy babies born from seronegative mothers, President Trump who has previously said the ACIP schedule is a “disgrace” has ordered a review of the US vaccine schedule in relationship to the countries. Alter AI assisted in this review.
Based on the 2025 immunization schedules published by health authorities worldwide — including the CDC/ACIP (U.S.), Public Health England/UKHSA, Health Canada, Australia’s Department of Health, and the EU’s national public health programs — there are significant differences in how intensively children are vaccinated from birth to age 18.
Although all developed countries recommend broadly similar vaccines (targeting diphtheria, measles, polio, etc.), the United States stands at the top in total injections and doses, followed by Canada, France/Germany, the UK, Australia, Sweden, and Japan.
 United States — Approx. 30–32 vaccine doses (counts combination products as single dose) before age 18
United States — Approx. 30–32 vaccine doses (counts combination products as single dose) before age 18
The 2025 CDC/ACIP schedule (see CDC PDF schedule, 2025) remains the most aggressive among Western nations.
By age one, a typical American baby receives 20+ doses spanning nine diseases (Hepatitis B, Rotavirus, DTaP, Hib, Pneumococcal, Polio, COVID‑19, Influenza, RSV). By age two, 32 individual antigens including monoclonal antibodies have been received in utero and after birth.
By age six, most children have accumulated around 27 to 29 doses, and around 30–32 total doses by age 18 (including HPV, meningococcal, Tdap boosters, annual flu shots, and now COVID boosters). Doses include combination products, so the number of antigens is much greater approximately 72-93 depending on maternal injections and other factors.
The U.S. uniquely begins vaccination at birth with Hepatitis B (now restricted to ~25,000 seropositive/carrier mothers) and adds multiple annual vaccines regardless of local exposure risk. It also promotes simultaneous injection of up to six vaccines at once (“combination vaccines” or same-visit stacking), magnifying early childhood exposure to adjuvants and preservatives.
 Canada — ≈ 25–28 doses
Canada — ≈ 25–28 doses
Canada’s national and provincial schedules (see Health Canada) mirror the U.S., but some provinces delay or skip optional vaccines (like flu or COVID‑19 for healthy children). Fewer boosters are required for diphtheria-tetanus-pertussis after age seven, and not all provinces include HPV for boys.
Canada therefore averages 2–4 fewer total doses than the United States.
 France /
France /  Germany — ≈ 22–25 doses
Germany — ≈ 22–25 doses
European Union countries vary widely:
- France mandates 11 childhood vaccines (including Hep B and Hib), but does not recommend early COVID‑19 or influenza vaccination for all children.
- Germany (STIKO guidelines) offers a schedule very similar to the U.S. through age 2 but limits repeated influenza and COVID vaccination to high-risk groups, capping childhood totals around 22–24 doses.
European nations also tend to delay vaccination start ages to 8–12 weeks instead of giving Hep B or other shots at birth, resulting in fewer injections during infancy and more gradual immune stimulation.
 United Kingdom — ≈ 20–21 doses
United Kingdom — ≈ 20–21 doses
The UK’s NHS and UKHSA recommend a smaller, slower schedule than North America’s. Infants receive about 16–18 doses by age 5, increasing to 20–21 by age 18.
Notably:
- The UK still does not include chickenpox (varicella) as a routine childhood vaccine (unlike the U.S.).
- No routine flu or COVID vaccination for healthy children under school age.
- Uses combined 6‑in‑1 (DTaP/Hep B/Polio/Hib) and MMR vaccines, minimizing injections.
 Australia — ≈ 20 doses
Australia — ≈ 20 doses
Australia’s National Immunisation Program (NIP) mirrors the UK more closely than the U.S.
Infants start at 6–8 weeks, not at birth (Hep B exception). Only one influenza vaccine per year is recommended, and chickenpox is given later. No universal COVID vaccine for healthy under‑5s.
Total injections: about 20 by adulthood.
 Sweden /
Sweden /  Norway — ≈ 16–18 doses
Norway — ≈ 16–18 doses
Nordic countries follow some of the world’s most minimalist Western schedules:
- No routine chickenpox, no birth shots, no annual flu or COVID for healthy kids.
- Combined vaccines reduce needle count.
- Emphasis on fewer but spaced doses (e.g., 3‑dose DTaP schedule instead of 5).
Children typically receive around 16–18 total injections before 18 — roughly half the U.S. burden — without suffering higher rates of “vaccine‑preventable” illness, challenging the dogma that more vaccines equal better outcomes.
 Japan — ≈ 14–16 doses
Japan — ≈ 14–16 doses
Historically the most cautious industrialized nation, Japan delayed and later reduced its vaccine schedule after serious adverse events in the 1990s.
Although it now recommends many standard vaccines, lower frequency, single-antigen use, and minimal early‑life stacking mean the total doses remain lowest in the developed world, around 14–16 through adolescence.
Japan’s infant mortality and autism rates are lower than in the U.S., prompting renewed scientific interest in whether slower schedules might lower iatrogenic risk.
 Summary — Total Vaccine Doses (Ages 0–18 Years)
Summary — Total Vaccine Doses (Ages 0–18 Years)
Rank Country Approx. cumulative doses Notes on schedule intensity 1  United States 30–32 Most intensive; starts at birth; annual flu + COVID 2
United States 30–32 Most intensive; starts at birth; annual flu + COVID 2  Canada 25–28 Slightly milder than U.S.; fewer mandatory boosters 3
Canada 25–28 Slightly milder than U.S.; fewer mandatory boosters 3  France /
France /  Germany 22–25 Similar core vaccines; delayed start; selective flu use 4
Germany 22–25 Similar core vaccines; delayed start; selective flu use 4  United Kingdom 20–21 No varicella or universal flu/COVID; efficient combinations 5
United Kingdom 20–21 No varicella or universal flu/COVID; efficient combinations 5  Australia ≈ 20 Spaced schedule; limited COVID coverage 6
Australia ≈ 20 Spaced schedule; limited COVID coverage 6  Sweden /
Sweden /  Norway 16–18 Simplified; no birth or seasonal routine vaccines 7
Norway 16–18 Simplified; no birth or seasonal routine vaccines 7  Japan 14–16 Most delayed; minimal birth and combination doses
Japan 14–16 Most delayed; minimal birth and combination doses
 Interpretation
Interpretation
The data show a clear gradient: the United States vaccinates children more frequently and at earlier ages than any other Western nation, often stacking combinations before immune maturity. Nations with slower, smaller schedules — Sweden and Japan most notably — maintain equal or superior child health metrics, casting doubt on the premise that maximal dosing guarantees better outcomes.
The U.S. model prioritizes population‑wide compliance and theoretical herd immunity, while Europe and Japan incorporate a more individualized risk‑based approach. Given the expanding scientific literature on rising childhood allergic and neuropsychiatric illnesses, these cross‑national differences underscore the need for independent, transparent studies comparing long‑term health outcomes by cumulative vaccine burden — something major regulatory agencies have conspicuously avoided.
FOCAL POINTS (Courageous Discourse) is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Please subscribe to FOCAL POINTS as a paying ($5 monthly) or founder member so we can continue to bring you the truth.
Peter A. McCullough, MD, MPH
Daily Caller
Trump Orders Review Of Why U.S. Childhood Vaccination Schedule Has More Shots Than Peer Countries


From the Daily Caller News Foundation
By Emily Kopp
President Donald Trump will direct his top health officials to conduct a systematic review of the childhood vaccinations schedule by reviewing those of other high-income countries and update domestic recommendations if the schedules abroad appear superior, according to a memorandum obtained by the Daily Caller News Foundation.
“In January 2025, the United States recommended vaccinating all children for 18 diseases, including COVID-19, making our country a high outlier in the number of vaccinations recommended for all children,” the memo will state. “Study is warranted to ensure that Americans are receiving the best, scientifically-supported medical advice in the world.”
Trump directs the secretary of the Health and Human Services (HHS) and the director of the Centers for Disease Control and Prevention to adopt best practices from other countries if deemed more medically sound. The memo cites the contrast between the U.S., which recommends vaccination for 18 diseases, and Denmark, which recommends vaccinations for 10 diseases; Japan, which recommends vaccinations for 14 diseases; and Germany, which recommends vaccinations for 15 diseases.
Dear Readers:
As a nonprofit, we are dependent on the generosity of our readers.
Please consider making a small donation of any amount here.
Thank you!
HHS Secretary Robert F. Kennedy Jr. has long been a critic of the U.S. childhood vaccination schedule.
The Trump Administration ended the blanket recommendation for all children to get annual COVID-19 vaccine boosters in perpetuity. Food and Drug Administration (FDA) Commissioner Marty Makary and Chief Medical Officer Vinay Prasad announced in May that the agency would not approve new COVID booster shots for children and healthy non-elderly adults without clinical trials demonstrating the benefit. On Friday, Prasad told his staff at the Center for Biologics Evaluation and Research that a review by career staff traced the deaths of 10 children to the COVID vaccine, announced new changes to vaccine regulation, and asked for “introspection.”
Trump’s memo follows a two-day meeting of vaccine advisors to the Centers for Disease Control and Prevention in which the committee adopted changes to U.S. policy on Hepatitis B vaccination that bring the country’s policy in alignment with 24 peer nations.

Total vaccines in January 2025 before the change in COVID policy. Credit: ACIP
The meeting included a presentation by FDA Center for Drug Evaluation and Research Director Tracy Beth Høeg showing the discordance between the childhood vaccination schedule in the U.S. and those of other developed nations.
“Why are we so different from other developed nations, and is it ethically and scientifically justified?” Høeg asked. “We owe our children science-based recommendations here in the United States.”
-
 National18 hours ago
National18 hours agoMedia bound to pay the price for selling their freedom to (selectively) offend
-

 Bruce Dowbiggin17 hours ago
Bruce Dowbiggin17 hours agoSometimes An Ingrate Nation Pt. 2: The Great One Makes His Choice
-

 Business6 hours ago
Business6 hours agoRecent price declines don’t solve Toronto’s housing affordability crisis
-

 Daily Caller7 hours ago
Daily Caller7 hours agoTech Mogul Gives $6 Billion To 25 Million Kids To Boost Trump Investment Accounts
-

 Business5 hours ago
Business5 hours agoOttawa’s gun ‘buyback’ program will cost billions—and for no good reason
-

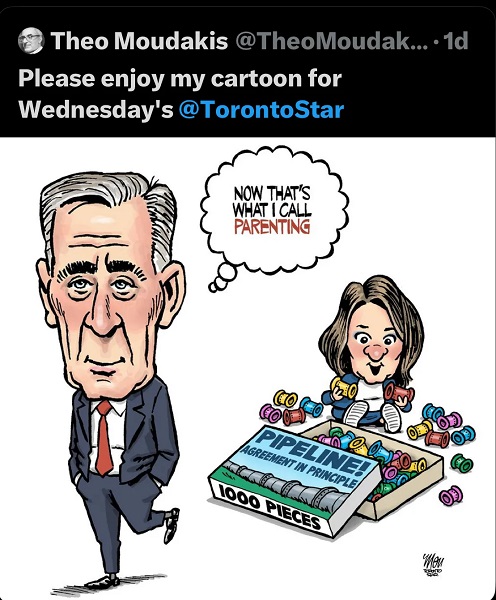
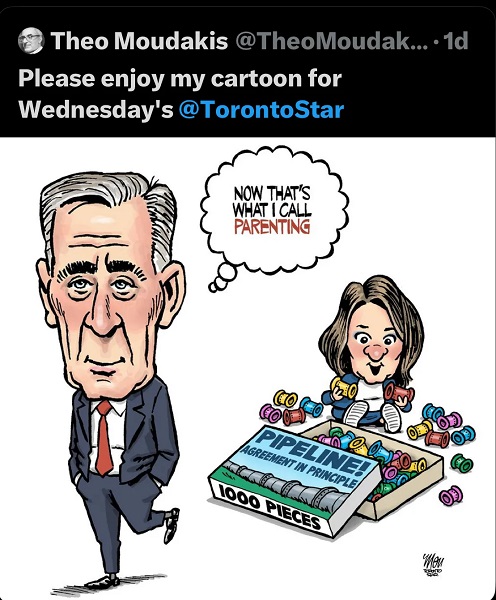
 Energy2 days ago
Energy2 days agoELZABETH MAY HAS IT WRONG: An Alberta to Prince Rupert Oil Pipeline Will Contribute to Greater Global Oil Tanker Safety
-
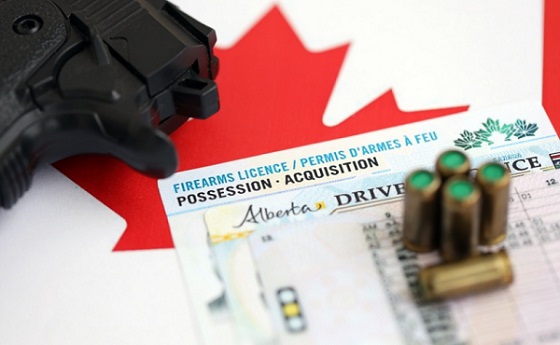
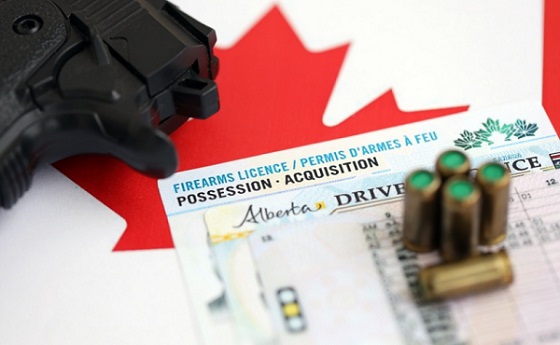 National2 days ago
National2 days agoAlberta will use provincial laws to stop Canadian gov’t from trying to confiscate legal firearms
-

 Energy9 hours ago
Energy9 hours agoThe Trickster Politics of the Tanker Ban are Hiding a Much Bigger Reckoning for B.C.






