Health
UK pediatrician who led review of child ‘transitions’ says US medical groups ‘misleading the public’

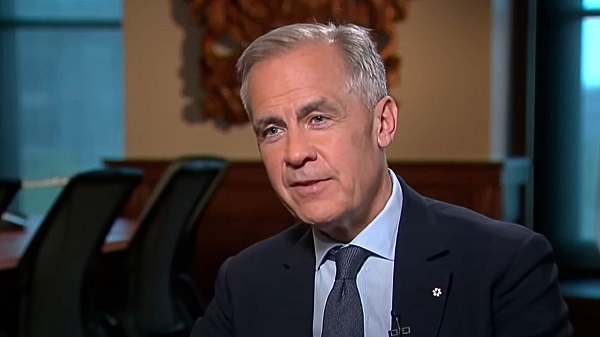
Dr. Hilary Cass, author of the Cass Review
From LifeSiteNews
The American Academy of Pediatrics’ support for surgically and chemically mutilating gender-confused children ‘is now demonstrated to be out of date by multiple systematic reviews,’ Dr. Hilary Cass told the New York Times.
The typically left-wing New York Times published an interview on Monday with consultant pediatrician Dr. Hilary Cass on her comprehensive review of so-called “gender medicine” in the United Kingdom, indicating that awareness of the damage due to surgical and chemical “transitioning” continues to spread despite the best efforts of LGBT activists.
Released in April, 366-page Cass Review was commissioned by National Health Service (NHS) England following ongoing scandals about the practices of British “gender clinics” such as the Gender Identity Development Service (GIDS), operated by the Tavistock and Portman NHS Foundation Trust. The four-year project consisted of comprehensive reviews of current research and international standards, as well as extensive interviews with gender-confused children and adults, family members, detransitioners, doctors, and activists.
It found that “gender medicine” is “built on shaky foundations” and that while such interventions require a great deal of caution, “quite the reverse happened in the field of [so-called] gender care for children,” and that “[w]hile a considerable amount of research has been published in this field, systematic evidence reviews demonstrated the poor quality of the published studies, meaning there is not a reliable evidence base upon which to make clinical decisions, or for children and their families to make informed choices.” Her findings led NHS to stop prescribing puberty blockers to children with gender confusion earlier this year.
Speaking to the Times, Cass explained that she was planning her retirement when she was first asked to tackle the project and was initially apprehensive about wading into the controversy.
“The most important concern for me is just how poor the evidence base is in this area,” she said. “Some people have questioned, ‘Did we set a higher bar for this group of young people?’ We absolutely didn’t. The real problem is that the evidence is very weak compared to many other areas of pediatric practice.”
The Times acknowledged that her “findings are in line with several European countries that have limited the treatments [sic] after scientific reviews. But in America, where nearly two dozen states have banned the care outright, medical groups have endorsed the treatments as evidence-based and necessary,” including groups the paper contacted for its latest story. Cass described American medical consensus as “out of date” on the issue.
“When I was president of the Royal College of Pediatrics and Child Health, we did some great work with the A.A.P. [American Academy of Pediatrics],” she elaborated. “They are an organization that I have enormous respect for. But I respectfully disagree with them on holding on to a position that is now demonstrated to be out of date by multiple systematic reviews.”
“It wouldn’t be too much of a problem if people were saying ‘This is clinical consensus and we’re not sure,” she added. “But what some organizations are doing is doubling down on saying the evidence is good. And I think that’s where you’re misleading the public. You need to be honest about the strength of the evidence and say what you’re going to do to improve it.”
A significant body of evidence shows that “affirming” gender confusion carries serious harms, especially when done with impressionable children who lack the mental development, emotional maturity, and life experience to consider the long-term ramifications of the decisions being pushed on them.
Studies find that more than 80% of children experiencing gender dysphoria outgrow it on their own by late adolescence, and that even full “reassignment” surgery often fails to resolve gender-confused individuals’ heightened tendency to engage in self-harm and suicide — and may even exacerbate it, including by reinforcing their confusion and neglecting the actual root causes of their mental strife.
Yet while mounting evidence against youth “gender transitions” is prompting European nations such as the United Kingdom and France, which are normally to the left of America, to move away from the practice, in America, the medical establishment and the Biden administration continues to dig in their heels, despite Biden’s own Substance Abuse & Mental Health Services Administration (SAMHSA) releasing a since-deleted report last year acknowledging that “lesbian, gay, and bisexual adults are more likely than straight adults to use substances, experience mental health conditions including major depressive episodes, and experience serious thoughts of suicide.”
The White House’s comprehensive pursuit of the transgender agenda has included reopening the military to recruits afflicted with gender dysphoria, promoting gender ideology within the military (including “diversity” and drag events on military bases), holding White House events to “affirm transgender kids,” condemning state laws against underage “transitions” as “close to sinful,” promoting underage “transitions” (potentially at taxpayer expense) as a “best practice,” and trying to force federally funded schools to let males into female athletic competitions and restrooms.
Health
‘Transgender’ males have 51% higher death rate than general population: study

From LifeSiteNews
Research found that men who underwent a ‘gender transition’ using hormones have a 51% higher mortality rate than the general population and a ‘threefold’ greater risk of cardiovascular deaths.
A newly published study has found that males’ use of estrogen to present as “female” triples their risk of cardiovascular disease, while also heightening the risk of stroke, blood clots, depression, and cognitive impairment.
The journal Discover Mental Health on June 12 released a variety of findings regarding the negative impacts of estrogen use in males attempting to transition to “female.” One of the most significant was that current estrogen use “was associated with a threefold increased risk of death from cardiovascular events.”
In fact, a study of 966 “female transitioned” males were found to have a mortality rate 51 percent higher than that of the general population. Their main causes of death included cardiovascular disease (21 percent), cancer (32 percent), suicide (7.5 percent), and infection-related disease (five percent).
Estrogen use by males amplified other cardiovascular risks, especially with prolonged use. One meta-analysis found a 30 percent higher rate of stroke among gender-confused men who took estrogen compared with men who did not.
A review also found “strong evidence” that estrogen use by men increases their risk for vein blood clots “over fivefold.”
Estrogen use was also found to have a detrimental cognitive impact on men. For example, so-called “female transitioned” males were found to have lower scores than both their other male counterparts and women in “information-processing speed and episodic memory.”
In addition, elevated symptoms of depression were “associated with increased serum levels of estradiol” for men under the age of 60.
This recent study confirms 2023 study that found that all gender-confused individuals, whether men attempting to present themselves as women or women attempting to present themselves as men, were at significantly increased risk for a range of deadly cardiovascular conditions, including strokes, heart attacks, high blood pressure, and elevated cholesterol levels.
A 2019 study published by the National Institutes of Health (NIH) National Library of Medicine also found:
Cardiovascular disease (CVD) is the leading disease-specific cause of death for [so-called] transgender people undergoing [transgender procedures], with only suicide claiming more lives as the leader of all cause mortality.
However, for [gender-confused males], the risk of death from CVD is 3-fold higher than for all other groups.
Research reported by both the British Heart Association and the American Heart Association that same year arrived at similar findings:
“We already know sex hormones are important to cardiovascular health, and now we have people being exposed to high levels of sex hormones they normally would not have, which could be associated with cardiovascular benefit or risk,” said Dr. Christian Delles, a professor at the Institute of Cardiovascular and Medical Sciences at the University of Glasgow.
Brownstone Institute
FDA Exposed: Hundreds of Drugs Approved without Proof They Work

From the Brownstone Institute
By
The US Food and Drug Administration (FDA) has approved hundreds of drugs without proof that they work—and in some cases, despite evidence that they cause harm.
That’s the finding of a blistering two-year investigation by medical journalists Jeanne Lenzer and Shannon Brownlee, published by The Lever.
Reviewing more than 400 drug approvals between 2013 and 2022, the authors found the agency repeatedly ignored its own scientific standards.
One expert put it bluntly—the FDA’s threshold for evidence “can’t go any lower because it’s already in the dirt.”
A System Built on Weak Evidence
The findings were damning—73% of drugs approved by the FDA during the study period failed to meet all four basic criteria for demonstrating “substantial evidence” of effectiveness.
Those four criteria—presence of a control group, replication in two well-conducted trials, blinding of participants and investigators, and the use of clinical endpoints like symptom relief or extended survival—are supposed to be the bedrock of drug evaluation.
Yet only 28% of drugs met all four criteria—40 drugs met none.
These aren’t obscure technicalities—they are the most basic safeguards to protect patients from ineffective or dangerous treatments.
But under political and industry pressure, the FDA has increasingly abandoned them in favour of speed and so-called “regulatory flexibility.”
Since the early 1990s, the agency has relied heavily on expedited pathways that fast-track drugs to market.
In theory, this balances urgency with scientific rigour. In practice, it has flipped the process. Companies can now get drugs approved before proving that they work, with the promise of follow-up trials later.
But, as Lenzer and Brownlee revealed, “Nearly half of the required follow-up studies are never completed—and those that are often fail to show the drugs work, even while they remain on the market.”
“This represents a seismic shift in FDA regulation that has been quietly accomplished with virtually no awareness by doctors or the public,” they added.
More than half the approvals examined relied on preliminary data—not solid evidence that patients lived longer, felt better, or functioned more effectively.
And even when follow-up studies are conducted, many rely on the same flawed surrogate measures rather than hard clinical outcomes.
The result: a regulatory system where the FDA no longer acts as a gatekeeper—but as a passive observer.
Cancer Drugs: High Stakes, Low Standards
Nowhere is this failure more visible than in oncology.
Only 3 out of 123 cancer drugs approved between 2013 and 2022 met all four of the FDA’s basic scientific standards.
Most—81%—were approved based on surrogate endpoints like tumour shrinkage, without any evidence that they improved survival or quality of life.
Take Copiktra, for example—a drug approved in 2018 for blood cancers. The FDA gave it the green light based on improved “progression-free survival,” a measure of how long a tumour stays stable.
But a review of post-marketing data showed that patients taking Copiktra died 11 months earlier than those on a comparator drug.
It took six years after those studies showed the drug reduced patients’ survival for the FDA to warn the public that Copiktra should not be used as a first- or second-line treatment for certain types of leukaemia and lymphoma, citing “an increased risk of treatment-related mortality.”
Elmiron: Ineffective, Dangerous—And Still on the Market
Another striking case is Elmiron, approved in 1996 for interstitial cystitis—a painful bladder condition.
The FDA authorized it based on “close to zero data,” on the condition that the company conduct a follow-up study to determine whether it actually worked.
That study wasn’t completed for 18 years—and when it was, it showed Elmiron was no better than placebo.
In the meantime, hundreds of patients suffered vision loss or blindness. Others were hospitalized with colitis. Some died.
Yet Elmiron is still on the market today. Doctors continue to prescribe it.
“Hundreds of thousands of patients have been exposed to the drug, and the American Urological Association lists it as the only FDA-approved medication for interstitial cystitis,” Lenzer and Brownlee reported.
“Dangling Approvals” and Regulatory Paralysis
The FDA even has a term—”dangling approvals”—for drugs that remain on the market despite failed or missing follow-up trials.
One notorious case is Avastin, approved in 2008 for metastatic breast cancer.
It was fast-tracked, again, based on ‘progression-free survival.’ But after five clinical trials showed no improvement in overall survival—and raised serious safety concerns—the FDA moved to revoke its approval for metastatic breast cancer.
The backlash was intense.
Drug companies and patient advocacy groups launched a campaign to keep Avastin on the market. FDA staff received violent threats. Police were posted outside the agency’s building.
The fallout was so severe that for more than two decades afterwards, the FDA did not initiate another involuntary drug withdrawal in the face of industry opposition.
Billions Wasted, Thousands Harmed
Between 2018 and 2021, US taxpayers—through Medicare and Medicaid—paid $18 billion for drugs approved under the condition that follow-up studies would be conducted. Many never were.
The cost in lives is even higher.
A 2015 study found that 86% of cancer drugs approved between 2008 and 2012 based on surrogate outcomes showed no evidence that they helped patients live longer.
An estimated 128,000 Americans die each year from the effects of properly prescribed medications—excluding opioid overdoses. That’s more than all deaths from illegal drugs combined.
A 2024 analysis by Danish physician Peter Gøtzsche found that adverse effects from prescription medicines now rank among the top three causes of death globally.
Doctors Misled by the Drug Labels
Despite the scale of the problem, most patients—and most doctors—have no idea.
A 2016 survey published in JAMA asked practising physicians a simple question—what does FDA approval actually mean?
Only 6% got it right.
The rest assumed that it meant the drug had shown clear, clinically meaningful benefits—such as helping patients live longer or feel better—and that the data was statistically sound.
But the FDA requires none of that.
Drugs can be approved based on a single small study, a surrogate endpoint, or marginal statistical findings. Labels are often based on limited data, yet many doctors take them at face value.
Harvard researcher Aaron Kesselheim, who led the survey, said the results were “disappointing, but not entirely surprising,” noting that few doctors are taught about how the FDA’s regulatory process actually works.
Instead, physicians often rely on labels, marketing, or assumptions—believing that if the FDA has authorized a drug, it must be both safe and effective.
But as The Lever investigation shows, that is not a safe assumption.
And without that knowledge, even well-meaning physicians may prescribe drugs that do little good—and cause real harm.
Who Is the FDA Working for?
In interviews with more than 100 experts, patients, and former regulators, Lenzer and Brownlee found widespread concern that the FDA has lost its way.
Many pointed to the agency’s dependence on industry money. A BMJ investigation in 2022 found that user fees now fund two-thirds of the FDA’s drug review budget—raising serious questions about independence.

Yale physician and regulatory expert Reshma Ramachandran said the system is in urgent need of reform.
“We need an agency that’s independent from the industry it regulates and that uses high-quality science to assess the safety and efficacy of new drugs,” she told The Lever. “Without that, we might as well go back to the days of snake oil and patent medicines.”
For now, patients remain unwitting participants in a vast, unspoken experiment—taking drugs that may never have been properly tested, trusting a regulator that too often fails to protect them.
And as Lenzer and Brownlee conclude, that trust is increasingly misplaced.
- Investigative report by Jeanne Lenzer and Shannon Brownlee at The Lever [link]
- Searchable public drug approval database [link]
- See my talk: Failure of Drug Regulation: Declining standards and institutional corruption
Republished from the author’s Substack
-

 COVID-199 hours ago
COVID-199 hours agoOntario man launches new challenge against province’s latest attempt to ban free expression on roadside billboards
-

 Energy17 hours ago
Energy17 hours agoThis Canada Day, Celebrate Energy Renewal
-

 Business1 day ago
Business1 day agoWhile China Hacks Canada, B.C. Sends Them a Billion-Dollar Ship Building Contract
-

 Alberta1 day ago
Alberta1 day agoSo Alberta, what’s next?
-

 Alberta8 hours ago
Alberta8 hours agoAlberta Next Takes A Look At Alberta Provincial Police Force
-

 Bjorn Lomborg1 day ago
Bjorn Lomborg1 day agoThe Physics Behind The Spanish Blackout
-

 Alberta10 hours ago
Alberta10 hours agoCanadian Oil Sands Production Expected to Reach All-time Highs this Year Despite Lower Oil Prices
-
 Business12 hours ago
Business12 hours agoPotential For Abuse Embedded In Bill C-5






