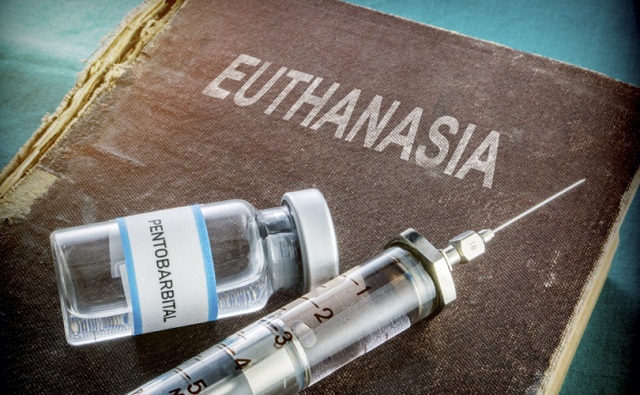
MAiD
Official data shows euthanasia deaths in Canada rose significantly in 2023
From LifeSiteNews
Medical Assistance in Dying (MAiD) increased 42% in 2023 in Quebec alone.
Deaths of Canadians by state-approved euthanasia have risen sharply in most provinces according to recent data, with approximately 16,000 people dying in 2023 alone, a significant increase from 2022 and an “out of control” rate, the nation’s leading anti-euthanasia advocacy group warned.
Official MAiD data from Ontario, Quebec, and Alberta shows the shocking level of deaths. In 2022, there were 13,241 Canadians who died by MAiD.
According to data from the Quebec Commission on End-of-Life Care’s eighth annual report, 5,211 people died by MAiD from April 1, 2022, to March 31, 2023, which is a large increase from 3,663 in the previous reporting period.
Alex Schadenberg, executive director of the Euthanasia Prevention Coalition (EPC), wrote in a recent blog that he predicts that 60,000 Canadians have died by MAiD since the deadly practice was legalized in 2016, with the rate increasing every year.
“Euthanasia is out of control in Canada,” Schadenberg said.
The EPC noted that deaths in Quebec from MAiD increased 42% in 2023, accounting for 6.8% of all deaths in the province. The report also shows that from April 1 to June 30, 2023, the number of MAiD deaths in the province went up 24%, which the EPC noted is “a slower pace of growth, but substantial considering the massive number of euthanasia deaths.”
The EPC also reflected that “Shockingly, 15% of those who died by euthanasia in Quebec were not terminally ill.”
MAiD data from Ontario released late last year shows there were 4,641 deaths in 2023, an 18% increase from 3,924 in 2022.
Data from Alberta shows that since June 2016 there have been 3,914 reported deaths by MAiD. However, 977 were in 2023, which is an 18% increase from 836 in 2022, or 594 in 2021.
Most MAiD deaths in Canada are done by a “doctor or nurse injecting a person, usually upon request, with a lethal poison cocktail,” the EPC noted.
Assisted suicide, the EPC says, is much less common and “is done by a doctor or nurse prescribing a person, usually upon request, a lethal poison cocktail that the person would take themselves.”
Last week, notably after pushback from pro-life, medical, and mental health groups as well as most of Canada’s provinces, the federal government under Prime Minister Justin Trudeau delayed its planned expansion of euthanasia to those suffering solely from mental illness to 2027.
Canadian Health Minister Mark Holland and Justice Minister Arif Virani announced the delay but said the government is still fully committed to expanding MAiD.
The delay was welcomed by the Euthanasia Prevention Coalition, but Schadenberg told LifeSiteNews that euthanasia “should be scrapped altogether.”
“We will be active in the next election reminding voters of the Members of Parliament who voted against Bill C-314 last fall, a bill that would have scrapped euthanasia for mental illness,” Schadenberg said.
Campaign Life Coalition (CLC) said that Canadians need “compassionate care, not killing,” and has urged Trudeau’s federal government to permanently scrap, not just delay, its planned expansion of euthanasia to those suffering from mental illness.
The Conservative Party of Canada (CPC) under leader Pierre Poilievre is supportive of the pause but wants the expansion of MAiD to be dropped altogether.
The CPC has opposed the expansion of MAiD, but recent attempts to stop the grim procedure, such as through Bill C-314, have failed.
The current delay is the second time the expansion has been put on hold.
Originally set to go into effect in March 2023, pressure from the same groups led the Liberals under Trudeau to delay Bill C-39.
The original delay in expanding MAiD until 2024 also came after numerous public scandals, including the surfacing of reports that Canadian veterans were being offered the fatal procedure by workers at Veterans Affairs Canada (VAC).
MAiD
Canada’s euthanasia regime is not health care, but a death machine for the unwanted

From LifeSiteNews
After ten years of assisted suicide, Canada has become synonymous with grim stories of death by lethal injection, with the regime’s net growing ever wider.
When Justin Trudeau took power in 2015, he announced that Canada was back and that his election was a harbinger of “sunny ways” and a new era for the country.
It was a new era, alright, but the ways turned out not to be sunny. In his ten years in office, over 60,000 Canadians were euthanized under the regime that his government brought in, and overnight, Canada became an international cautionary tale.
International headlines highlighted the grim story of Canada, where people were getting lethal injections because they were disabled; because they couldn’t get cancer treatment; because they were veterans with PTSD. As the U.K.’s Spectator asked in a chilling 2022 headline: “Why is Canada euthanizing the poor?”
READ: New Conservative bill would ban expansion of euthanasia to Canadians suffering mental illness
Indeed, in the United Kingdom – where Labour MP Kim Leadbeater’s dystopian assisted suicide bill passed last week – Canada was seen as so objectively horrifying that euthanasia advocates insisted that comparisons to their Commonwealth neighbor constituted fearmongering. Leadbeater, in fact, stated that her bill is “worlds apart” from Canada’s euthanasia regime. Anyone advocating for euthanasia must now reckon with Canada, which highlights how short and slick the slope really is.
Earlier this month, the New York state legislature also passed a bill legalizing assisted suicide; assisted suicide laws are also being considered in Maryland and Illinois. On June 14, the New York Times published a powerful op-ed by Ross Douthat titled “Why the Euthanasia Slope Is Slippery.” As is now standard in the international press, Canada’s euthanasia regime came up.
“A few days before the vote, my colleague Katie Engelhart published a report on the expansive laws allowing ‘medical assistance in dying’ in Canada,” Douthat wrote, “which were widened in 2021 to allow assisted suicide for people without a terminal illness, detailing how they worked in the specific case of Paula Ritchie, a chronically ill Canadian euthanized at her own request.”
“Many people who support assisted suicide in terminal cases have qualms about the Canadian system,” Douthat continued. “So it’s worth thinking about what makes a terminal-illness-only approach to euthanasia unstable, and why the logic of what New York is doing points in a Canadian direction even if the journey may not be immediate or direct.”
Notice, here, that a columnist can refer to the “Canadian direction” with the assumption that everybody recognizes, without question, that this a particularly bad direction to be heading in. Even euthanasia advocates, while privately admiring the scale and efficiency of the Canadian killing fields, feel it necessary to distance themselves from Canada publicly.
Douthat noted that the Canadian example reveals why the slippery slope is inevitable; that people have essentially come to expect that doctors “always need to offer something,” and that when no further care or treatment is possible, that assisted suicide should be available. This logic “assumes that the dying have entered a unique zone where the normal promises of medicine can no longer be kept, a state of exception where it makes sense to license doctors to deliver death as a cure.” But Douthat observes:
The problem is that a situation where the doctor tells you that there’s nothing more to be done for you is not really exceptional at all. Every day, all kinds of people are told that their suffering has no medical solution: people with crippling injuries, people with congenital conditions and people … with an array of health problems whose etiology science does not even understand.
READ: Cardinal Dolan denounces New York assisted suicide bill as ‘cheapening of human life’
The logic of assisted suicide means that inevitably, eligibility will expand to all kinds of suffering.
“Suffering is general and not limited, the dying are not really a category unto themselves, and the case for a lethal solution will creep beyond the bounds you set,” Douthat concluded. “In the end, you can have a consensus that suicide is intrinsically wrong, that suffering should be endured to whatever end and that doctors shouldn’t kill you. Or you can have an opening to death that will be narrow only at the start – and in the end, a wide gate through which many, many people will be herded.”
How do we know? Well, Douthat writes, “The Canadian experience shows this clearly.” After ten years of sunny ways, “Canada” has become synonymous with grim stories of death by lethal injection.
Indigenous
Carney’s Throne Speech lacked moral leadership

This article supplied by Troy Media.
 By Susan Korah
By Susan Korah
Carney’s throne speech offered pageantry, but ignored Indigenous treaty rights, MAID expansion and religious concerns
The Speech from the Throne, delivered by King Charles III on May 27 to open the latest session of Parliament under newly elected Prime Minister Mark Carney, was a confident assertion of Canada’s identity and outlined the government’s priorities for the session. However, beneath the
pageantry, it failed to address the country’s most urgent moral and constitutional responsibilities.
It also sent a coded message to U.S. President Donald Trump, subtly rebuking his repeated dismissal of Canada as a sovereign state. Trump has
previously downplayed Canada’s independence in trade talks and public statements, often treating it as economically subordinate to the U.S.
Still, a few discordant notes—most visibly from a group of First Nations chiefs in traditional headdresses—cut through the welcoming sounds that greeted the King and Queen Camilla on the streets of the capital.
The role of the Crown in Canada’s history sparked strong reactions from some Indigenous leaders who had travelled from as far as Alberta and Manitoba to voice their concerns.
“It’s time the Crown paid more than lip service to the Indigenous people of this country,” Chief Billy-Joe Tuccaro of the Mikisew Cree First Nation told me as he and his colleagues posed for photographs requested by several parade spectators. “We have been ignored and marginalized for far too long.”
He added that he and fellow chiefs from other First Nations were standing outside the Senate chamber as a symbol of their status as “outsiders,” despite being the land’s original inhabitants.
Shortly after Carney’s election, Tuccaro and Chief Sheldon Sunshine of the Sturgeon Lake Cree Nation sent him a joint letter stating: “As you
know, Canada is founded on Treaties that were sacred covenants between the Crown and our ancestors to share the lands. We are not prepared to accept any further Treaty breaches and violations.” They added that they looked forward to working with the new government as treaty partners.
Catholics, too, are being urged to remain vigilant about aspects of the government’s agenda that were either only briefly mentioned in the throne
speech or omitted altogether. On April 23, just days before Carney and the Liberals were returned to power, the Permanent Council of the Canadian Conference of Catholic Bishops issued a statement outlining what Catholics should expect from the new government.
“Our Catholic faith provides essential moral and social guidance, helping us understand and respond to the critical issues facing our country,” they wrote. “As the Church teaches, it is the duty of the faithful ‘to see that the divine law is inscribed in the life of the earthly city (Gaudium et Spes, n. 43.2).’”
The bishops expressed concern about the lack of legal protection for the unborn, the expansion of eligibility for medical assistance in dying (MAID)—which allows eligible Canadians to seek medically assisted death under specific legal conditions—and inadequate access to quality palliative care. They also reaffirmed the Church’s responsibility to walk “in justice and truth with Indigenous peoples.”
Although the speech emphasized tariffs, the removal of trade barriers and national security, it made no mention of the right to life, MAID or the charitable status of churches and church-related charities—a status the Trudeau government had considered revoking for some groups.
On Indigenous issues, the government pledged to be a reliable partner and to double the Indigenous Loan Guarantee Program from $5 billion to $10 billion. The program supports Indigenous equity participation in natural resource and infrastructure projects.
Canada deserves more than symbolic rhetoric—it needs a government that will confront its moral obligations head-on and act decisively on the challenges facing Indigenous peoples, faith communities, and the most vulnerable among us.
Susan Korah is Ottawa correspondent for The Catholic Register, a Troy Media Editorial Content Provider Partner.
Troy Media empowers Canadian community news outlets by providing independent, insightful analysis and commentary. Our mission is to support local media in helping Canadians stay informed and engaged by delivering reliable content that strengthens community connections and deepens understanding across the country.
-

 Business1 day ago
Business1 day agoLatest shakedown attempt by Canada Post underscores need for privatization
-

 Business1 day ago
Business1 day agoWhy it’s time to repeal the oil tanker ban on B.C.’s north coast
-
 Aristotle Foundation2 days ago
Aristotle Foundation2 days agoHow Vimy Ridge Shaped Canada
-

 Alberta1 day ago
Alberta1 day agoPierre Poilievre – Per Capita, Hardisty, Alberta Is the Most Important Little Town In Canada
-

 Alberta1 day ago
Alberta1 day agoAlberta Provincial Police – New chief of Independent Agency Police Service
-

 Energy1 day ago
Energy1 day agoIf Canada Wants to be the World’s Energy Partner, We Need to Act Like It
-

 MxM News1 day ago
MxM News1 day agoUPenn strips Lia Thomas of women’s swimming titles after Title IX investigation
-
 International2 days ago
International2 days agoCBS settles with Trump over doctored 60 Minutes Harris interview







