Health
Looking to Quit Smoking? You Can Get Free Coaching & Support During National Non-Smoking Week!

If you’re hoping to quit smoking, you know that there’s not one definitive way to go about it and you know it won’t be easy.
From cold turkey, to hypnosis to medication, the options for quitting seem endless. And while there is much research about the various ways to quit, London Drugs says they stand behind the combination of quit medication and quit counselling.
As part of the Canadian Council on Tobacco Control’s National Non-Smoking Week, the retailer is offering free stop-smoking counselling at pharmacies from January 21st to January 27th, 2018. In addition to providing tips and advice for reduction and quitting, pharmacists with proper authorization can also prescribe oral medications such as Champix and Zyban.
And even if you don’t make it to a pharmacy though, you know you’re on the right track if you’re considering quitting for good! Here are a couple stop-smoking resources you can access anytime:
Alberta Quits is a portal for free, web-based support from Alberta Health Services.
Smokers’ Helpline from the Canadian Cancer Society offers free and personalized tools to help you quit.
Fraser Institute
Long waits for health care hit Canadians in their pocketbooks

From the Fraser Institute
Canadians continue to endure long wait times for health care. And while waiting for care can obviously be detrimental to your health and wellbeing, it can also hurt your pocketbook.
In 2024, the latest year of available data, the median wait—from referral by a family doctor to treatment by a specialist—was 30 weeks (including 15 weeks waiting for treatment after seeing a specialist). And last year, an estimated 1.5 million Canadians were waiting for care.
It’s no wonder Canadians are frustrated with the current state of health care.
Again, long waits for care adversely impact patients in many different ways including physical pain, psychological distress and worsened treatment outcomes as lengthy waits can make the treatment of some problems more difficult. There’s also a less-talked about consequence—the impact of health-care waits on the ability of patients to participate in day-to-day life, work and earn a living.
According to a recent study published by the Fraser Institute, wait times for non-emergency surgery cost Canadian patients $5.2 billion in lost wages in 2024. That’s about $3,300 for each of the 1.5 million patients waiting for care. Crucially, this estimate only considers time at work. After also accounting for free time outside of work, the cost increases to $15.9 billion or more than $10,200 per person.
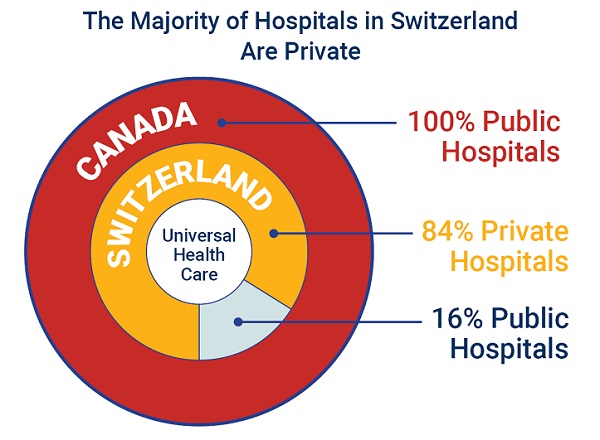
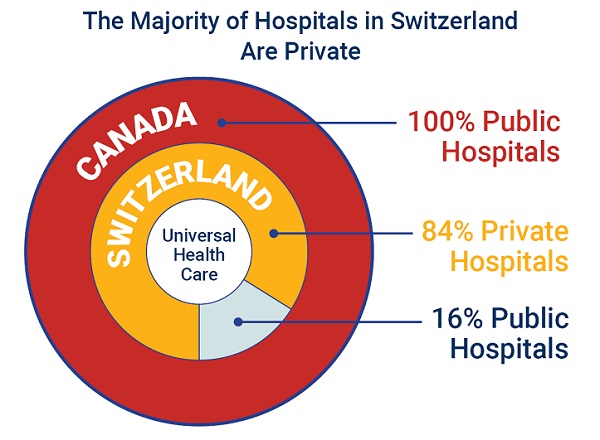
Of course, some advocates of the health-care status quo argue that long waits for care remain a necessary trade-off to ensure all Canadians receive universal health-care coverage. But the experience of many high-income countries with universal health care shows the opposite.
Despite Canada ranking among the highest spenders (4th of 31 countries) on health care (as a percentage of its economy) among other developed countries with universal health care, we consistently rank among the bottom for the number of doctors, hospital beds, MRIs and CT scanners. Canada also has one of the worst records on access to timely health care.
So what do these other countries do differently than Canada? In short, they embrace the private sector as a partner in providing universal care.
Australia, for instance, spends less on health care (again, as a percentage of its economy) than Canada, yet the percentage of patients in Australia (33.1 per cent) who report waiting more than two months for non-emergency surgery was much higher in Canada (58.3 per cent). Unlike in Canada, Australian patients can choose to receive non-emergency surgery in either a private or public hospital. In 2021/22, 58.6 per cent of non-emergency surgeries in Australia were performed in private hospitals.
But we don’t need to look abroad for evidence that the private sector can help reduce wait times by delivering publicly-funded care. From 2010 to 2014, the Saskatchewan government, among other policies, contracted out publicly-funded surgeries to private clinics and lowered the province’s median wait time from one of the longest in the country (26.5 weeks in 2010) to one of the shortest (14.2 weeks in 2014). The initiative also reduced the average cost of procedures by 26 per cent.
Canadians are waiting longer than ever for health care, and the economic costs of these waits have never been higher. Until policymakers have the courage to enact genuine reform, based in part on more successful universal health-care systems, this status quo will continue to cost Canadian patients.
Health
Just 3 Days Left to Win the Dream Home of a Lifetime!

|
|
|
|
|
-

 Alberta2 days ago
Alberta2 days agoOil prices are headed for a hard fall
-
 Health2 days ago
Health2 days agoRFK Jr. appoints Robert Malone, Martin Kulldorff, other COVID shot critics to overhauled CDC vaccine panel
-

 Business2 days ago
Business2 days agoOur addiction to dairy supply management is turning Canada into a trade pariah
-

 Business2 days ago
Business2 days agoThe carbon tax’s last stand – and what comes after
-
 Business2 days ago
Business2 days ago84% of Swiss hospitals and 60% of hospitalizations are in private facilities, and they face much lower wait times
-

 Bruce Dowbiggin2 days ago
Bruce Dowbiggin2 days agoCanadians Thinks America Owes Them. Trump Has Other Ideas
-

 conflict1 day ago
conflict1 day agoIsrael strikes Iran, targeting nuclear sites; U.S. not involved in attack
-

 Business1 day ago
Business1 day agoTrump: ‘Changes are coming’ to aggressive immigration policy after business complaints











