Fraser Institute
Enough talk, we need to actually do something about Canadian health care

From the Macdonald Laurier Institute
By J. Edward Les for Inside Policy
Canada spends more on health care as a percentage of GDP than almost all other OECD countries, yet we rank behind most of them when it comes to outcomes that matter.
I drove a stretch of road near Calgary’s South Health Campus the other day, a section with a series of three intersections in a span of less than a few hundred metres. That is, I tried to drive it – but spent far more time idling than moving.
At each intersection, after an interminable wait, the light turned green just as the next one flipped to red, grinding traffic to a halt just after it got rolling. It was excruciating; I’m quite sure I spied a snail on crutches racing by – no doubt making a beeline (snail-line?) for the ER a stone’s throw away.
The street’s sluggishness is perhaps reflective of the hospital next to it, given that our once-cherished universal health care system has crumbled into a universal waiting system – a system seemingly crafted (like that road) to obstruct flow rather than enable it. In fact, the pace of medical care delivery in this country has become so glacial that even a parking lot by comparison feels like the Indianapolis Speedway.
The health care crisis grows more dire by the day. Reforms are long overdue. Canada spends more on health care as a percentage of GDP than almost all other OECD countries, yet we rank behind most of them when it comes to outcomes that matter.
And we’re paying with our lives: according to the Canadian Institute for Health Information, thousands of Canadians die each and every year because of the inefficiencies of our system.
Yet for all that we are paralyzed by the enormity and complexity of the mushrooming disaster. We talk about solutions – and then we talk and talk some more. But for all the talking, precious little action is taken.
I’m reminded of an Anne Lamotte vignette, related in her bestselling book Bird By Bird:
Thirty years ago my older brother, who was ten years old at the time, was trying to get a report written on birds that he’d had three months to write, which was due the next day. We were out at our family cabin in Bolinas, and he was at the kitchen table close to tears, surrounded by binder paper and pencils and unopened books about birds, immobilized by the hugeness of the task ahead. Then my father sat down beside him, put his arm around my brother’s shoulder, and said, “Bird by bird, buddy. Just take it bird by bird.”
So it is with Canadian health care: we’ve wasted years wringing our hands about the woeful state of affairs, while doing precious little about it.
Enough procrastinating. It’s time to tackle the crisis, bird by bird.
One thing we can do is to let doctors be doctors. A few weeks ago, in a piece titled “Should Doctors Mind Their Own Business?”, I questioned the customary habit of doctors hanging out their shingles in small independent community practices. Physicians spend long years of training to master their craft, years during which they receive no training in business methods whatsoever, and then we expect them to master those skills off to the side of their exam rooms. Some do it well, but many do not – and it detracts from their attention to patients.
We don’t install newly minted teachers in classrooms and at the same time task them with the keeping the lights on, managing the supply chain, overseeing staffing and payroll, and all the other mechanics of running schools. Why do we expect that of doctors?
Keeping doctors embedded within large, expensive, inefficient, bureaucracy-choked hospitals isn’t the solution, either.
There’s a better way, I argued in my essay: regional medical centres – centres built and administered in partnership with the private sector.
Such centres would allow practitioners currently practicing in the community to ply their trade unencumbered by the nuts and bolts of running a business; and they would allow us to decant a host of services from hospitals, which should be reserved for what only hospitals can do: emergency services, inpatient care, surgeries, and the like.
In short, we should let doctors be doctors, and hospitals be hospitals.
To garner feedback, I dumped my musings into a couple of online physician forums to which I belong, tagged with the query: “Food for thought, or fodder for the compost bin?”
The verdict? Hands down, the compost bin.
I was a bit taken aback, initially. Offended, even – because who among us isn’t in love with their own ideas?
But it quickly became evident from my peers’ comments that I’d been misunderstood. Not because my doctor friends are dim, but because I hadn’t been clear.
When I proposed in my essay that we “leave the administration and day-to-day tasks of running those centres to business folks who know what they’re doing,” my colleagues took that to mean that doctors would be serving at the beck and call of a tranche of ill-informed government-enabled administrators – and they reacted to the notion with anaphylactic derision. And understandably so: too many of us have long and painful experience with thick layers of health care bureaucracy seemingly organized according to the Peter Principle, with people promoted to – and permanently stuck at – the level of their incompetence.
But I didn’t mean to suggest – not for a minute – that doctors shouldn’t be engaged in running these centres. I also wrote: “None of which is to suggest that doctors shouldn’t be involved, by aptitude and inclination, in influencing the set-up and management of regional centres – of course, they should.”
Of course they should. There are plenty of physicians equipped with both the skills and interest needed to administer these centres; and they should absolutely be front and centre in leading them.
But more than that: everyone should have skin in the game. All workers have the right to share in the success of an enterprise; and when they do, everybody wins. When everyone is pulling in the same direction because everyone shares in the wins, waste and inefficiencies are rooted out like magic.
Contrast that to how hospitals are run, with scarcely anyone aware of the actual cost of the blood tests or CT scans they order or the packets of suture and gauze they rip open, and with the motivations of administrative staff, nurses, doctors, and other personnel running off in more directions than a flock of headless chickens. The capacity for waste and inefficiencies is almost limitless.
I don’t mean to suggest that the goal of regional medical centres should be to turn a profit; but fiscal prudence and economic accountability are to be celebrated, because money not wasted is money that can be allocated to enhancing patient care.
Nor do I mean to intimate that sensible resource management should be the only parameter tracked; patient outcomes and patient satisfaction are paramount.
What should government’s role be in all this? Initially, to incentivize the creation of these centres via public-private partnerships; and then, crucially, to encourage competition among them and to reward innovation and performance, with optimization of the three key metrics – patient outcomes, patient satisfaction, and economic accountability – always in focus.
No one should be mandated to work in non-hospital regional medical centres. It’s a free country (or it should be): doctors should be free to hang out their own community shingles if they wish. But if we build the model correctly, my contention is that most medical professionals will prefer to work collaboratively under one roof with a diverse group of colleagues, unencumbered by the mundanities of running a business, but also free of choking hospital bureaucracy.
I connected a couple weeks ago with the always insightful economist Jack Mintz (who is also a distinguished fellow at the Macdonald-Laurier Institute). Mintz sits on the board of a Toronto-area hospital and sees first-hand “the problems with the lack of supply, population growth, long wait times between admission and getting a bed, emergency room overuse,” and so on.
“Something has to give,” he said. “Probably more resources but better managed. We really need major reform.”
On that we can all agree. We can’t carry on this way.
So, let’s stop idling; and let’s green-light some fixes.
As Samwise Gamgee said in The Lord of the Rings, “It’s the job that’s never started as takes longest to finish.”
Dr. J. Edward Les is a pediatrician in Calgary who writes on politics, social issues, and other matters.
Business
Municipal government per-person spending in Canada hit near record levels
From the Fraser Institute
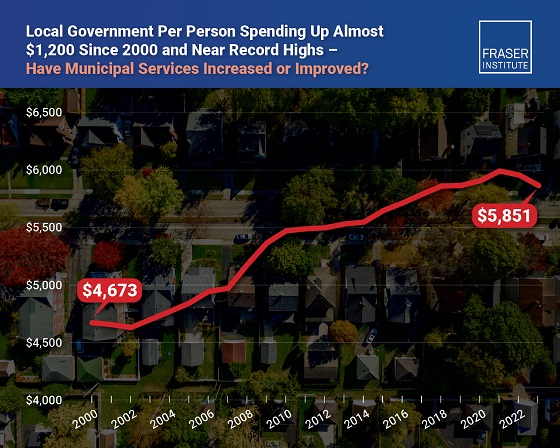
Municipal government spending in Canada hit near record levels in recent years, finds a new study by the Fraser Institute, an independent, non-partisan Canadian public policy think-tank.
“In light of record-high spending in municipalities across Canada, residents should consider whether or not crime, homelessness, public transit and other services have actually improved,” said Austin Thompson, senior policy analyst at the Fraser Institute and author of The Expanding Finances of Local Governments in Canada.
From 2000 to 2023, per-person spending (inflation-adjusted) increased by 25.2 per cent, reaching a record-high $5,974 per person in 2021 before declining slightly to $5,851 in 2023, the latest year of available data.
During that same period, municipal government revenue—generated from property taxes and transfers from other levels of government—increased by 33.7 per cent per person (inflation-adjusted).
And yet, among all three levels of government including federal and provincial, municipal government spending (adjusted for inflation) has actually experienced the slowest rate of growth over the last 10 years, underscoring the large spikes in spending at all government levels across Canada.
“Despite claims from municipal policymakers about their dire financial positions, Canadians should understand the true state of finances at city hall so they can decide whether they’re getting good value for their money,” said Jake Fuss, director of fiscal studies at the Fraser Institute.
The Expanding Finances of Local Governments in Canada, 1990–2023
- Canada’s local governments have experienced substantial fiscal growth in recent decades.
- Revenue and expenditure by local governments—including municipal governments, school boards, and Indigenous governments—have increased faster than population growth and inflation combined. From 1990 to 2023, real per-capita revenue rose by 32.7%, and expenditure by 30.0%.
- Local governments represent a significant component of Canada’s broader public sector. In 2023, net of inter-governmental transfers, municipal governments and school boards accounted for 18.6% of total government expenditure and 11.1% of revenue.
- Despite this growth, local governments’ share of overall government revenue and expenditure has declined over time—especially since the COVID-19 pandemic—as federal and provincial budgets have expanded even more rapidly.
- Nevertheless, between 2008 and 2023 the inflation-adjusted per-capita revenue of municipal governments in-creased by 10.1% and their expenditure by 12.4% , on average across the provinces.
- Over the same period, municipal governments recorded above-inflation increases in their combined annual operating surpluses, which contributed to an 88.1% inflation-adjusted rise in their net worth—raising important questions about the allocation of accumulated resources.
- In 2023, Ontario recorded the highest per-capita municipal revenue among the provinces ($4,156), while Alberta had the highest per-capita expenditure ($3,750). Prince Edward Island reported the lowest per-capita municipal revenue ($1,635) and expenditure ($1,186).
- Wide variation in per-capita municipal revenue and expenditure across the provinces reflects differences in the responsibilities provinces assign to municipalities, as well as possible disparities in the efficiency of service delivery—issues that warrant further scrutiny.
Click Here To Read The Full Study
Business
Massive government child-care plan wreaking havoc across Ontario

From the Fraser Institute
By Matthew Lau
It’s now more than four years since the federal Liberal government pledged $30 billion in spending over five years for $10-per-day national child care, and more than three years since Ontario’s Progressive Conservative government signed a $13.2 billion deal with the federal government to deliver this child-care plan.
Not surprisingly, with massive government funding came massive government control. While demand for child care has increased due to the government subsidies and lower out-of-pocket costs for parents, the plan significantly restricts how child-care centres operate (including what items participating centres may purchase), and crucially, caps the proportion of government funds available to private for-profit providers.
What have families and taxpayers got for this enormous government effort? Widespread child-care shortages across Ontario.
For example, according to the City of Ottawa, the number of children (aged 0 to 5 years) on child-care waitlists has ballooned by more than 300 per cent since 2019, there are significant disparities in affordable child-care access “with nearly half of neighbourhoods underserved, and limited access in suburban and rural areas,” and families face “significantly higher” costs for before-and-after-school care for school-age children.
In addition, Ottawa families find the system “complex and difficult to navigate” and “fewer child care options exist for children with special needs.” And while 42 per cent of surveyed parents need flexible child care (weekends, evenings, part-time care), only one per cent of child-care centres offer these flexible options. These are clearly not encouraging statistics, and show that a government-knows-best approach does not properly anticipate the diverse needs of diverse families.
Moreover, according to the Peel Region’s 2025 pre-budget submission to the federal government (essentially, a list of asks and recommendations), it “has maximized its for-profit allocation, leaving 1,460 for-profit spaces on a waitlist.” In other words, families can’t access $10-per-day child care—the central promise of the plan—because the government has capped the number of for-profit centres.
Similarly, according to Halton Region’s pre-budget submission to the provincial government, “no additional families can be supported with affordable child care” because, under current provincial rules, government funding can only be used to reduce child-care fees for families already in the program.
And according to a March 2025 Oxford County report, the municipality is experiencing a shortage of child-care staff and access challenges for low-income families and children with special needs. The report includes a grim bureaucratic predication that “provincial expansion targets do not reflect anticipated child care demand.”
Child-care access is also a problem provincewide. In Stratford, which has a population of roughly 33,000, the municipal government reports that more than 1,000 children are on a child-care waitlist. Similarly in Port Colborne (population 20,000), the city’s chief administrative officer told city council in April 2025 there were almost 500 children on daycare waitlists at the beginning of the school term. As of the end of last year, Guelph and Wellington County reportedly had a total of 2,569 full-day child-care spaces for children up to age four, versus a waitlist of 4,559 children—in other words, nearly two times as many children on a waitlist compared to the number of child-care spaces.
More examples. In Prince Edward County, population around 26,000, there are more than 400 children waitlisted for licensed daycare. In Kawartha Lakes and Haliburton County, the child-care waitlist is about 1,500 children long and the average wait time is four years. And in St. Mary’s, there are more than 600 children waitlisted for child care, but in recent years town staff have only been able to move 25 to 30 children off the wait list annually.
The numbers speak for themselves. Massive government spending and control over child care has created havoc for Ontario families and made child-care access worse. This cannot be a surprise. Quebec’s child-care system has been largely government controlled for decades, with poor results. Why would Ontario be any different? And how long will Premier Ford allow this debacle to continue before he asks the new prime minister to rethink the child-care policy of his predecessor?
-

 COVID-191 day ago
COVID-191 day agoOntario man launches new challenge against province’s latest attempt to ban free expression on roadside billboards
-

 COVID-1910 hours ago
COVID-1910 hours agoNew Peer-Reviewed Study Affirms COVID Vaccines Reduce Fertility
-

 Energy2 days ago
Energy2 days agoThis Canada Day, Celebrate Energy Renewal
-

 Alberta1 day ago
Alberta1 day agoAlberta Next Takes A Look At Alberta Provincial Police Force
-

 Business6 hours ago
Business6 hours agoOttawa Funded the China Ferry Deal—Then Pretended to Oppose It
-

 International1 day ago
International1 day agoPresident Xi Skips Key Summit, Adding Fuel to Ebbing Power Theories
-

 Alberta1 day ago
Alberta1 day agoCanadian Oil Sands Production Expected to Reach All-time Highs this Year Despite Lower Oil Prices
-

 MAiD8 hours ago
MAiD8 hours agoCanada’s euthanasia regime is not health care, but a death machine for the unwanted







