Fraser Institute
Canadians are ready for health-care reform—Australia shows the way

From the Fraser Institute
By Bacchus Barua and Mackenzie Moir
Australia offers real-world examples of how public/private partnerships can be successfully integrated in a universal health-care framework. Not only does Australia prove it can be done without sacrificing universal coverage for all, Australia spends less money (as a share of its economy) than Canada and enjoys more timely medical care.
Canada’s health-care system is crumbling. Long wait times, hallway health care and burned-out staff are now the norm. Unsurprisingly, a new poll finds that the majority of Canadians (73 per cent) say the system needs major reform.
As noted in a recent editorial in the Globe and Mail, we can learn key lessons from Australia.
There are significant similarities between the two countries with respect to culture, the economy and even geographic characteristics. Both countries also share the goal of ensuring universal health coverage. However, Australia outperforms Canada on several key health-care performance metrics.
After controlling for differences in age (where appropriate) between the two countries, our recent study found that Australia’s health-care system outperformed Canada’s on 33 (of 36) performance measures. For example, Australia had more physicians, hospital beds, CT scanners and MRI machines per person compared to Canada. And among the 30 universal health-care countries studied, Canada ranked in the bottom quartile for the availability of these critical health-care resources.
Australia also outperforms Canada on key measures of wait times. In 2023 (the latest year of available data), 39.5 per cent of patients in Australia were able to make a same or next day appointment when they were sick compared to only 22.3 per cent in Canada. And 9.6 per cent of Canadians reported waiting more than one year to see a specialist compared to only 4.5 per cent of Australians. Similarly, almost one-in-five (19.9 per cent) Canadians reported waiting more than one year for non-emergency surgery compared to only 11.8 per cent of Australians.
So, what does Australia do differently to outperform Canada on these key measures?
Although the Globe and Mail editorial touches on the availability of private insurance in Australia, less attention is given to the private sector’s prominent role in the delivery of health care.
In 2016 (the latest year of available data) almost half of all hospitals in Australia (48.5 per cent) were private. And in 2021/22 (again, the latest year of available data), 41 per cent of all hospital care took place in a private facility. That percentage goes up to 70.3 per cent when only considering hospital admissions for non-emergency surgery.
But it’s not only higher-income patients who can afford private insurance (or those paying out of pocket) who get these surgeries. The Australian government encourages the uptake of private insurance and partially subsidizes private care (at a rate of 75 per cent of the public fee), and governments in Australia also regularly contract out publicly-funded care to private facilities.
In 2021/22, more than 300,000 episodes of publicly-funded care occurred in private facilities in Australia. Private hospitals also delivered 73.5 per cent of care funded by Australia’s Department of Veterans’ Affairs. And in 2019/20, government sources (including the federal government) paid for almost one-third (32.8 per cent) of private hospital expenditures.
Which takes us back to the new opinion poll (by Navigator), which found that 69 per cent of Canadians agree that health-care services should include private-sector involvement. While defenders of the status quo continue to criticize this approach, Australia offers real-world examples of how public/private partnerships can be successfully integrated in a universal health-care framework. Not only does Australia prove it can be done without sacrificing universal coverage for all, Australia spends less money (as a share of its economy) than Canada and enjoys more timely medical care.
While provincial governments remain stubbornly committed to a failed model, Canadians are clearly expressing their desire for health-care reforms that include a prominent role for private partners in the delivery of universal care.
Australia is just one example. Public/private partnerships are the norm in several more successful universal health-care systems (such as Germany and Switzerland). Instead of continuing to remain an outlier, Canada should follow the examples of Australia and other countries and engage with the private sector to fulfill the promise of universal health care.
Authors:
Community
Charitable giving on the decline in Canada

From the Fraser Institute
By Jake Fuss and Grady Munro
There would have been 1.5 million more Canadians who donated to charity in 2023—and $755.5 million more in donations—had Canadians given to the same extent they did 10 years prior
According to recent polling, approximately one in five Canadians have skipped paying a bill over the past year so they can buy groceries. As families are increasingly hard-pressed to make ends meet, this undoubtedly means more and more people must seek out food banks, shelters and other charitable organizations to meet their basic necessities.
And each year, Canadians across the country donate their time and money to charities to help those in need—particularly around the holiday season. Yet at a time when the relatively high cost of living means these organizations need more resources, new data published by the Fraser Institute shows that the level of charitable giving in Canada is actually falling.
Specifically, over the last 10 years (2013 to 2023, the latest year of available data) the share of tax-filers who reported donating to charity fell from 21.9 per cent to 16.8 per cent. And while fewer Canadians are donating to charity, they’re also donating a smaller share of their income—during the same 10-year period, the share of aggregate income donated to charity fell from 0.55 per cent to 0.52 per cent.
To put this decline into perspective, consider this: there would have been 1.5 million more Canadians who donated to charity in 2023—and $755.5 million more in donations—had Canadians given to the same extent they did 10 years prior. Simply put, this long-standing decline in charitable giving in Canada ultimately limits the resources available for charities to help those in need.
On the bright side, despite the worrying long-term trends, the share of aggregate income donated to charity recently increased from 0.50 per cent in 2022 to 0.52 per cent in 2023. While this may seem like a marginal improvement, 0.02 per cent of aggregate income for all Canadians in 2023 was $255.7 million.
The provinces also reflect the national trends. From 2013 to 2023, every province saw a decline in the share of tax-filers donating to charity. These declines ranged from 15.4 per cent in Quebec to 31.4 per cent in Prince Edward Island.
Similarly, almost every province recorded a drop in the share of aggregate income donated to charity, with the largest being the 24.7 per cent decline seen in P.E.I. The only province to buck this trend was Alberta, which saw a 3.9 per cent increase in the share of aggregate income donated over the decade.
Just as Canada as a whole saw a recent improvement in the share of aggregate income donated, so too did many of the provinces. Indeed, seven provinces (except Manitoba, Nova Scotia and Newfoundland and Labrador) saw an increase in the share of aggregate income donated to charity from 2022 to 2023, with the largest increases occurring in Saskatchewan (7.9 per cent) and Alberta (6.7 per cent).
Canadians also volunteer their time to help those in need, yet the latest data show that volunteerism is also on the wane. According to Statistics Canada, the share of Canadians who volunteered (both formally and informally) fell by 8 per cent from 2018 to 2023. And the total numbers of hours volunteered (again, both formal and informal) fell by 18 per cent over that same period.
With many Canadians struggling to make ends meet, food banks, shelters and other charitable organizations play a critical role in providing basic necessities to those in need. Yet charitable giving—which provides resources for these charities—has long been on the decline. Hopefully, we’ll see this trend turn around swiftly.
Alberta
Schools should go back to basics to mitigate effects of AI

From the Fraser Institute
Odds are, you can’t tell whether this sentence was written by AI. Schools across Canada face the same problem. And happily, some are finding simple solutions.
Manitoba’s Division Scolaire Franco-Manitobaine recently issued new guidelines for teachers, to only assign optional homework and reading in grades Kindergarten to six, and limit homework in grades seven to 12. The reason? The proliferation of generative artificial intelligence (AI) chatbots such as ChatGPT make it very difficult for teachers, juggling a heavy workload, to discern genuine student work from AI-generated text. In fact, according to Division superintendent Alain Laberge, “Most of the [after-school assignment] submissions, we find, are coming from AI, to be quite honest.”
This problem isn’t limited to Manitoba, of course.
Two provincial doors down, in Alberta, new data analysis revealed that high school report card grades are rising while scores on provincewide assessments are not—particularly since 2022, the year ChatGPT was released. Report cards account for take-home work, while standardized tests are written in person, in the presence of teaching staff.
Specifically, from 2016 to 2019, the average standardized test score in Alberta across a range of subjects was 64 while the report card grade was 73.3—or 9.3 percentage points higher). From 2022 and 2024, the gap increased to 12.5 percentage points. (Data for 2020 and 2021 are unavailable due to COVID school closures.)
In lieu of take-home work, the Division Scolaire Franco-Manitobaine recommends nightly reading for students, which is a great idea. Having students read nightly doesn’t cost schools a dime but it’s strongly associated with improving academic outcomes.
According to a Programme for International Student Assessment (PISA) analysis of 174,000 student scores across 32 countries, the connection between daily reading and literacy was “moderately strong and meaningful,” and reading engagement affects reading achievement more than the socioeconomic status, gender or family structure of students.
All of this points to an undeniable shift in education—that is, teachers are losing a once-valuable tool (homework) and shifting more work back into the classroom. And while new technologies will continue to change the education landscape in heretofore unknown ways, one time-tested winning strategy is to go back to basics.
And some of “the basics” have slipped rapidly away. Some college students in elite universities arrive on campus never having read an entire book. Many university professors bemoan the newfound inability of students to write essays or deconstruct basic story components. Canada’s average PISA scores—a test of 15-year-olds in math, reading and science—have plummeted. In math, student test scores have dropped 35 points—the PISA equivalent of nearly two years of lost learning—in the last two decades. In reading, students have fallen about one year behind while science scores dropped moderately.
The decline in Canadian student achievement predates the widespread access of generative AI, but AI complicates the problem. Again, the solution needn’t be costly or complicated. There’s a reason why many tech CEOs famously send their children to screen-free schools. If technology is too tempting, in or outside of class, students should write with a pencil and paper. If ChatGPT is too hard to detect (and we know it is, because even AI often can’t accurately detect AI), in-class essays and assignments make sense.
And crucially, standardized tests provide the most reliable equitable measure of student progress, and if properly monitored, they’re AI-proof. Yet standardized testing is on the wane in Canada, thanks to long-standing attacks from teacher unions and other opponents, and despite broad support from parents. Now more than ever, parents and educators require reliable data to access the ability of students. Standardized testing varies widely among the provinces, but parents in every province should demand a strong standardized testing regime.
AI may be here to stay and it may play a large role in the future of education. But if schools deprive students of the ability to read books, structure clear sentences, correspond organically with other humans and complete their own work, they will do students no favours. The best way to ensure kids are “future ready”—to borrow a phrase oft-used to justify seesawing educational tech trends—is to school them in the basics.
-

 Censorship Industrial Complex2 days ago
Censorship Industrial Complex2 days agoDeath by a thousand clicks – government censorship of Canada’s internet
-

 Daily Caller2 days ago
Daily Caller2 days agoChinese Billionaire Tried To Build US-Born Baby Empire As Overseas Elites Turn To American Surrogates
-

 Digital ID2 days ago
Digital ID2 days agoCanada releases new digital ID app for personal documents despite privacy concerns
-

 Community2 days ago
Community2 days agoCharitable giving on the decline in Canada
-

 Alberta19 hours ago
Alberta19 hours agoAlberta’s huge oil sands reserves dwarf U.S. shale
-
 Bruce Dowbiggin2 days ago
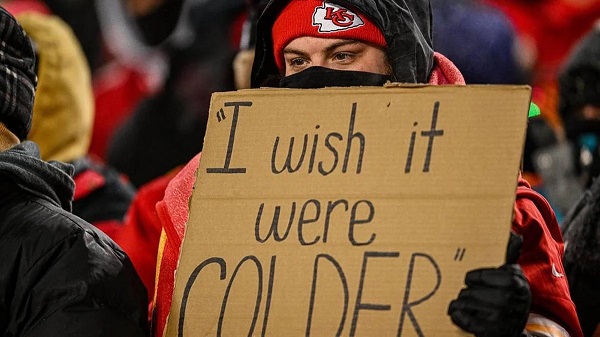
Bruce Dowbiggin2 days agoNFL Ice Bowls Turn Down The Thermostat on Climate Change Hysteria
-
 Energy15 hours ago
Energy15 hours agoCanada’s sudden rediscovery of energy ambition has been greeted with a familiar charge: hypocrisy
-

 Alberta22 hours ago
Alberta22 hours agoCanada’s New Green Deal





