Health
Canadian dentists desperate for details on federal dental care plan
News release from Canada’s Provincial and Territorial Dental Associations
Canadian dentists to MPs: We need answers about the Canadian Dental Care Plan
Lack of consultation with provincial and territorial dental associations is worrying
There are only two months left before the Canadian Dental Care Plan (CDCP) becomes available to many more Canadians. Yet more than 25,000 dentists nationwide are in the dark about how the Government of Canada will safeguard access to dental care.
In a letter sent to Members of Parliament (MPs) this week, the presidents of provincial and territorial dental associations across the country asked how the government will:
- Safeguard employer-provided dental plans that two-thirds of Canadians currently have access to?
- Ensure that a strong federal program can be coordinated with existing provincial programs?
- Protect patient choice and maintain the patient-provider relationship?
- Ensure minimal, efficient administration that promotes timely access to care?
- Respect the costs of delivering dental care to maximize provider participation?
- Increase the number of dental assistants and dental hygienists to meet the demands of the CDCP?
Dentists want to champion a CDCP that will respect patients, providers, and taxpayers. The provincial and territorial dental associations are concerned that the CDCP has been compromised by a lack of meaningful consultation with dentists – who will be expected to deliver on the government’s promises.
The CDCP is currently in final planning stages, with a potential rollout in 2024 that will attempt to increase access to uninsured Canadians under 18, people with disabilities, and seniors who have an annual family income of less than $90,000. Dentists believe all Canadians need access to dental care. If not done properly, two-thirds of Canadians who have great employer-provided dental plans could lose their coverage and be forced into a worse plan. Costs would then skyrocket, which means the $13 billion over five years the government set aside would not be enough to sustain the plan.
Let’s take the time to get it right. We can increase access to dental care right now through an expansion of the interim measure already in place – the Canada Dental Benefit. This establishes a fixed dollar amount that a patient can use to be reimbursed for dental-related expenses.
Facts:
- Canada’s provincial and territorial dental associations represent more than 25,000 licensed dentists working in more than 16,000 offices. They treat more than 30 million Canadians every year and employ at least 50,0001 oral health care workers.
- Over 60 per cent of Canadians have a dentist they visit on a regular basis.2
- A recent survey commissioned by Health Canada found that nearly nine out 10 Canadians are satisfied with the Canada Dental Benefit.3
Quotes:
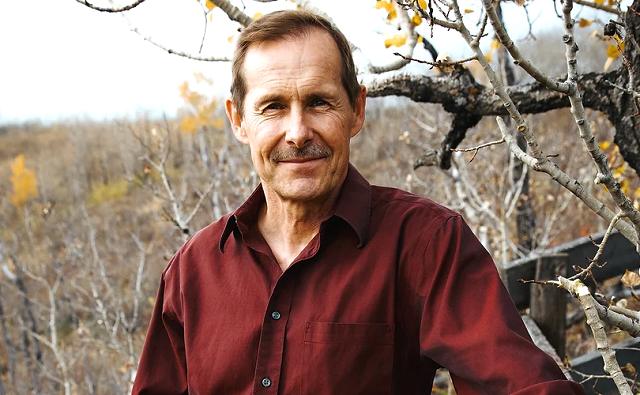
“To succeed, this plan needs to work for both patients and providers, and to work in each province. What we are recommending is based on decades of experience and caring for the oral health needs of the more than 30 million people that come into our dental offices across the country every year.” — Dr. Bruce Yaholnitsky, President, Alberta Dental Association
“Poorly designed programs do not improve access to care, and they leave the most vulnerable people in society behind. This is an historic opportunity, but only if the government gets it right. Dentists have the expertise, experience, and skills to know what it takes to ensure good oral and overall health.” — Dr. Rob Wolanski, President, British Columbia Dental Association
“As dentists we are excited to be a part of this Canadian dental care program, but there are key critical issues that need to be included for this program to be successful.” — Dr. Scott Leckie, President, Manitoba Dental Association
“New Brunswick dentists are already extremely busy with the recent spike in population and the backlog in demand for services related to Covid-19. This program was intended to provide dental care to the 35 per cent of Canadians who are uninsured. It needs to be easy to understand and to administer, and to be fair to all parties, including patients, dental care providers and taxpayers. Canadians need to know what benefits are being provided and which are not, before they arrive at the dental clinic.” — Dr. Joanah Campbell, President, New Brunswick Dental Society
“The new program must be sustainable in terms of funding, and easy to understand and access. It has to be patient-centred and work for everyone.” — Dr. Shane Roberts, President, Newfoundland & Labrador Dental Association
“While the CDCP has the potential to improve the lives of many Canadians, this can only be achieved if it’s done right. To ensure the greatest possible outcome, we must consider all of the moving pieces and take a patient-centred approach.” — Dr. Juli Waterbury, President, Nova Scotia Dental Association
“The CDCP could be a game-changer for Canadians’ access to dental care. But we have one chance to get it right. Here in Ontario, we have seen that dental care programs developed without the input of dentists are doomed to fail. Just look at the Ontario Seniors Dental Care Program, where waiting lists are up to two years long in some areas, and some patients have to travel ridiculously long distances to receive treatment.” — Dr. Brock Nicolucci, President, Ontario Dental Association
“This new program has the potential to improve access to care for many Canadians. It must be sustainable, patient-centred, and easy to access for patients. A poorly designed program will not improve access to care which is something we would like to avoid. We want this to work for Canadians.” — Dr. Derek Thiessen, President, College of Dental Surgeons of Saskatchewan
Alberta
Red Deer Hospital Lottery – Second Chance Early Bird Prize!!!

|
|
|
|
|
Health
Private Footage Reveals Leading Medical Org’s Efforts To ‘Normalize’ Gender Ideology

 From the Daily Caller News Foundation
From the Daily Caller News Foundation
By MEGAN BROCK AND KATE ANDERSON
I have developed a part of my brain that’s very fluid around with some of my folks asking them each week, what name are you going by? What pronouns are we using today? So it keeps us flexible to be doing this work.
This is the seventh article in the “WPATH Tapes” series on the World Professional Association for Transgender Health and the gender medical industry. Read the overview of our investigation here.
Members of the world’s most prominent transgender medical organization encouraged fellow doctors to push transgender ideology beyond the healthcare field into schools and their communities, according to internal recordings obtained by the Daily Caller News Foundation.
In September 2022, the World Professional Association of Transgender Health (WPATH) Global Education Institute (GEI) hosted an event that included a series of education sessions for certification in transgender medicine. The event coincided with the release of WPATH’s updated medical guidance, called the Standards of Care Version 8 (SOC 8), and provided additional insights on its clinical applications.
During the sessions WPATH members were encouraged to “normalize” preferred pronoun use as a way to “create societal change” and behave in a way that “affirms” their patients’ gender identity, such as by asking female patients if they have a penis.
Psychologist Ren Massey, the co-chair of WPATH GEI, said clinicians should be ready to act as advocates for “gender diversity” in school settings. Massey earned a Ph.D. in clinical psychology from University of South Florida and is not a physician.
“We want to have the skills to negotiate multiple roles,” Massey said. “Because I have both had to be the therapist and then go talk to the school and be an advocate, or do a talk to the whole community of a school. So, I’m in multiple hats that we get to navigate, if we are advocating and helping and supporting our trans and gender diverse folks we are working with.”
Massey did not respond to requests for comment, and neither did Massey’s psychology practice.
Transgender ideology includes the belief that a person’s sex can be different from their “gender identity,” which SOC 8 defines as “a person’s deeply felt, internal, intrinsic sense of their own gender.” It’s a rejection of long-established scientific understanding of biology that there are only two sexes based on the fact there are only two types of reproductive cells — sperm and ova.
The term “gender identity” was popularized in the 1960s by controversial sexologist John Money, who’s most high-profile experiment involved advising parents of a boy whose penis was damaged in a botched circumcision to cut the rest of it off and raise him as a girl. At age 15, the boy — who was raised as “Brenda” — discovered the truth and rejected further hormone treatments. He eventually committed suicide at age 38.
The very concept of “gender identity” creates the possibility of changing one’s sex — a biological impossibility — through medical interventions, therefore creating a demand for medical sex reassignment interventions.
SOC 8 recommends that gender dysphoric minors be given the opportunity to “change” their sex through medical interventions. The guidance has been used to inform government regulations, insurance policies, and recommendations by numerous medical organizations, increasing minors access to sex reassignment procedures.
‘We Will Facilitate Changes’
The call for clinicians to be involved in local schools was echoed by WPATH-affiliated psychologist Dr. Wallace Wong in a presentation titled “Foundations in Gender Affirming Mental Health Care in Childhood and Adolescence.” Wong explained how therapists can play a pivotal role in facilitating change by helping schools embrace transgenderism and explained that schools need to embrace the use of preferred pronouns.
“A lot of time we will facilitate changes. It’s not unusual that you will go to the school with the parents together and educate the school what to do,” said Wong. “A lot of the times, some school they say, ‘we don’t know what to do.’ You say, ‘that doesn’t fly, I will teach you how to do,’” Wong said.
Wong did not respond to requests for comment, and the Diversity and Emotional Wellness Centre, where Wong works, provided additional contact information but did not provide comment.
SOC 8 recommends that “health care professionals work with families, schools, and other relevant settings to promote acceptance of gender diverse expressions of behavior and identities of the adolescent.”
“Using different pronouns for children is a step towards their social transition. It is now well established that social transition leads to the medicalization of their care,” Dr. Stanley Goldfarb of Do No Harm, a watchdog organization focused on keeping identity politics out of healthcare and medical schools, told the DCNF.
“It is inappropriate for anyone to advocate gender transition in gender dysphoric children unless they have had extensive psychological counseling and are part of some formal research protocol,” Goldfarb said. “This is the new policy in the United Kingdom and in multiple European countries.”
Without naming a specific doctor, Goldfarb said that “for a physician to speak to untrained personnel given the psychological difficulties that these children often experience along with their gender dysphoria, is bordering on malpractice.”
‘The Face Of The Enemy’
As European nations such as Norway, Sweden, Denmark, and the U.K. have restricted or halted the use of cross-sex hormones and puberty blockers in minors, WPATH has rallied against similar bans in the United States.
The WPATH GEI educational event dedicated an entire session to transgender legal and policy issues. Paula Neira, a biological man who identifies as a woman and is program director of LGBTQ Equity & Education at Johns Hopkins Medicine, gave a presentation titled “Legal Issues & Policy.” During the talk, Neira criticized legislative efforts aimed at stopping child sex changes and protecting women’s sports.
“Numerous states have either engaged in having litigation and legislation proposed or the government has taken actions that are targeting the LGBTQ+ community broadly, and then at least half of these bills are specifically targeting transgender people, particularly transgender youth. The way that these bills are being played out is, one is attempts to ban gender affirming care,” Neira said.
“In Alabama they’re trying to criminalize, by making it a felony, to provide gender-affirming care to transgender youth. The bill is called the “Alabama Child Compassion and Protection Act” so the height of cynicism and hypocrisy,” Neira said.
Neira ended the session by calling on WPATH members to band together and stand firm against “attacks” on the transgender community.
“Being defiant in the face of the enemy is not something that’s unfamiliar to me,” Neria said. “It’s going to take a lot of resolve. It’s going take a lot of resilience. It’s going take a lot of mutual support, to stand firm under these attacks. And that’s what we have to do. And we have to do it with a clear strategic eye. And that means banding together. It means being strategic in how we challenge policy, how we advocate and make persuasive arguments.”
“And together we’re gonna get back to making progress no matter how bleak it looks now, as long as we never give in. And we never surrender,” Neira told the audience, prompting applause.
Neira did not respond to requests for comment. Johns Hopkins Medicine, where Neira works, responded but did not provide comment.
‘Helps All Humans’
Throughout the 30 hours of WPATH GEI recordings reviewed by the DCNF, speakers cast a vision of moving gender ideology beyond sex change procedures and promoting it in other domains such as schools, communities and public policy.
Dr. Scott Leibowitz, a WPATH board member and SOC 8 co-author, said it “helps all humans” to promote the acceptance of transgender ideology in a diversity of settings.
“We recommend health care professionals who work with families. They should work with families, schools, and other relevant settings to promote acceptance of gender diverse expressions of behavior and identities of the adolescent,” Leibowitz said.
“Notice, we don’t say: ‘work with these settings to promote acceptance of transgender people,’” Leibowitz told the audience. “We actually think it’s broader than that because by helping promote acceptance of gender diversity as a whole, we believe that helps all humans, including trans people. It doesn’t reinforce the notion of boxes, which is what we’re trying to move away from.”
Leibowitz declined an interview request through a Nationwide Children’s Hospitals spokesperson.
WPATH’s commitment to social change is captured in its own guidelines.
“WPATH recognizes that health is not only dependent upon high-quality clinical care but also relies on social and political climates that ensure social tolerance, equality, and the full rights of citizenship,” the guidelines read. “Health is promoted through public policies and legal reforms that advance tolerance and equity for gender diversity and that eliminate prejudice, discrimination, and stigma. WPATH is committed to advocacy for these policy and legal changes.”
‘Creating Change By Using Different Language’
WPATH members were also encouraged to use preferred pronouns in healthcare practices, with Massey describing the use of preferred pronouns as a way to create social change.
“I would encourage you in your practices to have universal approaches to correct pronouns. So, training your staff so they’re aware and have good interaction skills. Maybe even have role plays with them,” Massey said.
“We are creating change by using different language,” said Massey.
Massey, who maintains an active psychology practice, said it’s “good clinical practice” to let clients dictate terminology used to describe their sex and gender.
“I’ve had folks that within the same day or within the same week may shift from feeling masculine, feminine, both, neither,” Massey said.
“And so that’s a thing like I have developed a part of my brain that’s very fluid around with some of my folks asking them each week, what name are you going by? What pronouns are we using today? So it keeps us flexible to be doing this work. There is so much evolution and so much exciting work developing.”
SOC 8 recommends that healthcare professionals use the “language or terminology” preferred by the patient.
‘Normalize It’
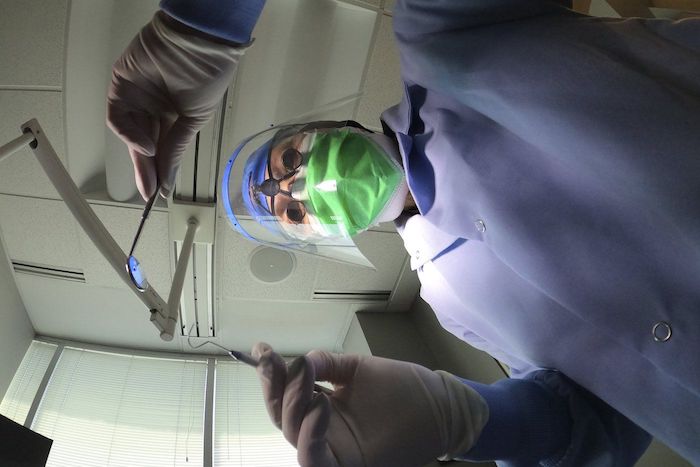
Dr. Jennifer Slovis, the medical director of the Oakland Kaiser Permanente Gender Clinic, promoted the use of an electronic medical database that collects sexual orientation and gender identity information for all patients. On the form, healthcare providers were expected to indicate a patient’s preferred pronouns and gender identity, as well as take an “organ inventory” for the patient.
The organ inventory asks both men and women to indicate their reproductive organs on a list that includes the cervix, breasts, uterus, vagina, testes, prostate and penis. Clinicians were also asked to indicate which organs were present at birth, had been surgically constructed, or developed by hormones.
Slovis explained that to “normalize” the organ inventory, this data needs to be collected for all patients, including “cisgender” patients.
“Cisgender people too, we should be doing this for everybody. That’s the only way we’re going to normalize it, if we do it for everybody,” said Slovis.
Slovis did not respond to requests for comment, and neither did Kaiser Permanente, where Slovis works.
In a presentation titled “Foundations in Primary Care,” Dr. Erika Sullivan said organ inventories needed to be constantly taken because patients’ organs “change.”
“One of the things I always like to illustrate with this is that you don’t just ask this question once, right? Because this changes. And so sexual practices change, pronouns change, organs change,” said Sullivan.
“You kind of have to constantly take that inventory to find out like, what’s what, what’s where, what are we doing?” Sullivan said.
WPATH’s SOC 8 supports the use of organ inventories.
“In electronic health records, organ/anatomical inventories can be standardly used to inform appropriate clinical care, rather than relying solely on assigned sex at birth and/ or gender identity designations,” the guidelines read.
Sullivan also explained the importance of using preferred pronouns and not assuming a patient’s pronouns based on outward appearance.
“I should be asking this of everybody and introducing myself this way, ‘Hi, I’m Erica, I use she/her pronouns,’” Sullivan said. “Because I think if we are going by sort of presentation, we are taking so much bias and so much judgment into that space. It’s really important to just wipe that away. So asking everyone’s pronouns is important because really, ultimately, you have to question your assumptions.”
Sullivan did not respond to requests for comment, and neither did the University of Utah, where Sullivan works.
Goldfarb said doctors should focus on patient care, not promoting gender ideology.
“It is not the job of physicians to create a culture of gender ideology. The job of physicians is to care for ill people,” Goldfarb said. “The proper care for children with gender dysphoria is intensive psychological treatment. The idea that all this should be normalized represents pure ideology and is not based on hard science or valid clinical research.”
WPATH did not respond to multiple requests for comment.
-

 Brownstone Institute2 days ago
Brownstone Institute2 days agoMedical Elites’ Disgrace Over Ivermectin
-

 COVID-191 day ago
COVID-191 day agoThe New York Times Admits Injuries from COVID-19 Shots
-

 Opinion2 days ago
Opinion2 days agoThe American Experiment Has Gone Down In Flames
-

 National15 hours ago
National15 hours agoDespite claims of 215 ‘unmarked graves,’ no bodies have been found at Canadian residential school
-

 Energy1 day ago
Energy1 day agoBuckle Up for Summer Blackouts: Wind Is Already Failing Texas in Spring
-

 Energy1 day ago
Energy1 day agoFederal government continues to reject golden opportunities to export LNG
-

 conflict1 day ago
conflict1 day ago‘It Makes No Sense’: Experts Puzzled By Biden Admin’s Claim That Rafah Invasion Wouldn’t Help Israel Defeat Hamas
-

 COVID-191 day ago
COVID-191 day agoFormer COVID coordinator Deborah Birx now admits jabs could have injured ‘thousands’