Health
Canadian dentists desperate for details on federal dental care plan
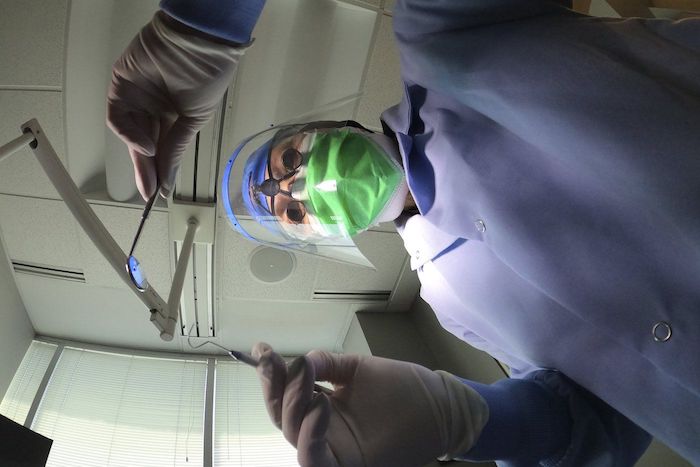
News release from Canada’s Provincial and Territorial Dental Associations
Canadian dentists to MPs: We need answers about the Canadian Dental Care Plan
Lack of consultation with provincial and territorial dental associations is worrying
There are only two months left before the Canadian Dental Care Plan (CDCP) becomes available to many more Canadians. Yet more than 25,000 dentists nationwide are in the dark about how the Government of Canada will safeguard access to dental care.
In a letter sent to Members of Parliament (MPs) this week, the presidents of provincial and territorial dental associations across the country asked how the government will:
- Safeguard employer-provided dental plans that two-thirds of Canadians currently have access to?
- Ensure that a strong federal program can be coordinated with existing provincial programs?
- Protect patient choice and maintain the patient-provider relationship?
- Ensure minimal, efficient administration that promotes timely access to care?
- Respect the costs of delivering dental care to maximize provider participation?
- Increase the number of dental assistants and dental hygienists to meet the demands of the CDCP?
Dentists want to champion a CDCP that will respect patients, providers, and taxpayers. The provincial and territorial dental associations are concerned that the CDCP has been compromised by a lack of meaningful consultation with dentists – who will be expected to deliver on the government’s promises.
The CDCP is currently in final planning stages, with a potential rollout in 2024 that will attempt to increase access to uninsured Canadians under 18, people with disabilities, and seniors who have an annual family income of less than $90,000. Dentists believe all Canadians need access to dental care. If not done properly, two-thirds of Canadians who have great employer-provided dental plans could lose their coverage and be forced into a worse plan. Costs would then skyrocket, which means the $13 billion over five years the government set aside would not be enough to sustain the plan.
Let’s take the time to get it right. We can increase access to dental care right now through an expansion of the interim measure already in place – the Canada Dental Benefit. This establishes a fixed dollar amount that a patient can use to be reimbursed for dental-related expenses.
Facts:
- Canada’s provincial and territorial dental associations represent more than 25,000 licensed dentists working in more than 16,000 offices. They treat more than 30 million Canadians every year and employ at least 50,0001 oral health care workers.
- Over 60 per cent of Canadians have a dentist they visit on a regular basis.2
- A recent survey commissioned by Health Canada found that nearly nine out 10 Canadians are satisfied with the Canada Dental Benefit.3
Quotes:
“To succeed, this plan needs to work for both patients and providers, and to work in each province. What we are recommending is based on decades of experience and caring for the oral health needs of the more than 30 million people that come into our dental offices across the country every year.” — Dr. Bruce Yaholnitsky, President, Alberta Dental Association
“Poorly designed programs do not improve access to care, and they leave the most vulnerable people in society behind. This is an historic opportunity, but only if the government gets it right. Dentists have the expertise, experience, and skills to know what it takes to ensure good oral and overall health.” — Dr. Rob Wolanski, President, British Columbia Dental Association
“As dentists we are excited to be a part of this Canadian dental care program, but there are key critical issues that need to be included for this program to be successful.” — Dr. Scott Leckie, President, Manitoba Dental Association
“New Brunswick dentists are already extremely busy with the recent spike in population and the backlog in demand for services related to Covid-19. This program was intended to provide dental care to the 35 per cent of Canadians who are uninsured. It needs to be easy to understand and to administer, and to be fair to all parties, including patients, dental care providers and taxpayers. Canadians need to know what benefits are being provided and which are not, before they arrive at the dental clinic.” — Dr. Joanah Campbell, President, New Brunswick Dental Society
“The new program must be sustainable in terms of funding, and easy to understand and access. It has to be patient-centred and work for everyone.” — Dr. Shane Roberts, President, Newfoundland & Labrador Dental Association
“While the CDCP has the potential to improve the lives of many Canadians, this can only be achieved if it’s done right. To ensure the greatest possible outcome, we must consider all of the moving pieces and take a patient-centred approach.” — Dr. Juli Waterbury, President, Nova Scotia Dental Association
“The CDCP could be a game-changer for Canadians’ access to dental care. But we have one chance to get it right. Here in Ontario, we have seen that dental care programs developed without the input of dentists are doomed to fail. Just look at the Ontario Seniors Dental Care Program, where waiting lists are up to two years long in some areas, and some patients have to travel ridiculously long distances to receive treatment.” — Dr. Brock Nicolucci, President, Ontario Dental Association
“This new program has the potential to improve access to care for many Canadians. It must be sustainable, patient-centred, and easy to access for patients. A poorly designed program will not improve access to care which is something we would like to avoid. We want this to work for Canadians.” — Dr. Derek Thiessen, President, College of Dental Surgeons of Saskatchewan
Brownstone Institute
Net Zero: The Mystery of the Falling Fertility

From the Brownstone Institute
By
If you want to argue that a mysterious factor X is responsible for the drop in fertility, you will have to explain (1) why the factor affected only the vaccinated, and (2) why it started affecting them at about the time of vaccination.
In January 2022, the number of children born in the Czech Republic suddenly decreased by about 10%. By the end of 2022, it had become clear that this was a signal: All the monthly numbers of newborns were mysteriously low.
In April 2023, I wrote a piece for a Czech investigative platform InFakta and suggested that this unexpected phenomenon might be connected to the aggressive vaccination campaign that had started approximately 9 months before the drop in natality. Denik N – a Czech equivalent of the New York Times – immediately came forward with a “devastating takedown” of my article, labeled me a liar and claimed that the pattern can be explained by demographics: There were fewer women in the population and they were getting older.
To compare fertility across countries (and time), the so-called Total Fertility Rate (TFR) is used. Roughly speaking, it is the average number of children that are born to a woman over her lifetime. TFR is independent of the number of women and of their age structure. Figure 1 below shows the evolution of TFR in several European countries between 2001 and 2023. I selected countries that experienced a similar drop in TFR in 2022 as the Czech Republic.

So, by the end of 2023, the following two points were clear:
- The drop in natality in the Czech Republic in 2022 could not be explained by demographic factors. Total fertility rate – which is independent of the number of women and their age structure – dropped sharply in 2022 and has been decreasing ever since. The data for 2024 show that the Czech TFR has decreased further to 1.37.
- Many other European countries experienced the same dramatic and unexpected decrease in fertility that started at the beginning of 2022. I have selected some of them for Figure 1 but there are more: The Netherlands, Norway, Slovakia, Slovenia, and Sweden. On the other hand, there are some countries that do not show a sudden drop in TFR, but rather a steady decline over a longer period (e.g. Belgium, France, UK, Greece, or Italy). Notable exceptions are Bulgaria, Spain, and Portugal where fertility has increased (albeit from very low numbers). The Human Fertility Project database has all the numbers.
This data pattern is so amazing and unexpected that even the mainstream media in Europe cannot avoid the problem completely. From time to time, talking heads with many academic titles appear and push one of the politically correct narratives: It’s Putin! (Spoiler alert: The war started in February 2022; however, children not born in 2022 were not conceived in 2021). It’s the inflation caused by Putin! (Sorry, that was even later). It’s the demographics! (Nope, see above, TFR is independent of the demographics).
Thus, the “v” word keeps creeping back into people’s minds and the Web’s Wild West is ripe with speculation. We decided not to speculate but to wrestle some more data from the Czech government. For many months, we were trying to acquire the number of newborns in each month, broken down by age and vaccination status of the mother. The post-socialist health-care system of our country is a double-edged sword: On one hand, the state collects much more data about citizens than an American would believe. On the other hand, we have an equivalent of the FOIA, and we are not afraid to use it. After many months of fruitless correspondence with the authorities, we turned to Jitka Chalankova – a Czech Ron Johnson in skirts – who finally managed to obtain an invaluable data sheet.
To my knowledge, the datasheet (now publicly available with an English translation here) is the only officially released dataset containing a breakdown of newborns by the Covid-19 vaccination status of the mother. We requested much more detailed data, but this is all we got. The data contains the number of births per month between January 2021 and December 2023 given by women (aged 18-39) who were vaccinated, i.e., had received at least one Covid vaccine dose by the date of delivery, and by women who were unvaccinated, i.e., had not received any dose of any Covid vaccine by the date of delivery.
Furthermore, the numbers of births per month by women vaccinated by one or more doses during pregnancy were provided. This enabled us to estimate the number of women who were vaccinated before conception. Then, we used open data on the Czech population structure by age, and open data on Covid vaccination by day, sex, and age.
Combining these three datasets, we were able to estimate the rates of successful conceptions (i.e., conceptions that led to births nine months later) by preconception vaccination status of the mother. Those interested in the technical details of the procedure may read Methods in the newly released paper. It is worth mentioning that the paper had been rejected without review in six high-ranking scientific journals. In Figure 2, we reprint the main finding of our analysis.

Figure 2 reveals several interesting patterns that I list here in order of importance:
- Vaccinated women conceived about a third fewer children than would be expected from their share of the population. Unvaccinated women conceived at about the same rate as all women before the pandemic. Thus, a strong association between Covid vaccination status and successful conceptions has been established.
- In the second half of 2021, there was a peak in the rate of conceptions of the unvaccinated (and a corresponding trough in the vaccinated). This points to rather intelligent behavior of Czech women, who – contrary to the official advice – probably avoided vaccination if they wanted to get pregnant. This concentrated the pregnancies in the unvaccinated group and produced the peak.
- In the first half of 2021, there was significant uncertainty in the estimates of the conception rates. The lower estimate of the conception rate in the vaccinated was produced by assuming that all women vaccinated (by at least one dose) during pregnancy were unvaccinated before conception. This was almost certainly true in the first half of 2021 because the vaccines were not available prior to 2021. The upper estimate was produced by assuming that all women vaccinated (by at least one dose) during pregnancy also received at least one dose before conception. This was probably closer to the truth in the second part of 2021. Thus, we think that the true conception rates for the vaccinated start close to the lower bound in early 2021 and end close to the upper bound in early 2022. Once again, we would like to be much more precise, but we have to work with what we have got.
Now that the association between Covid-19 vaccination and lower rates of conception has been established, the one important question looms: Is this association causal? In other words, did the Covid-19 vaccines really prevent women from getting pregnant?
The guardians of the official narrative brush off our findings and say that the difference is easily explained by confounding: The vaccinated tend to be older, more educated, city-dwelling, more climate change aware…you name it. That all may well be true, but in early 2022, the TFR of the whole population dropped sharply and has been decreasing ever since.
So, something must have happened in the spring of 2021. Had the population of women just spontaneously separated into two groups – rednecks who wanted kids and didn’t want the jab, and city slickers who didn’t want kids and wanted the jab – the fertility rate of the unvaccinated would indeed be much higher than that of the vaccinated. In that respect, such a selection bias could explain the observed pattern. However, had this been true, the total TFR of the whole population would have remained constant.
But this is not what happened. For some reason, the TFR of the whole population jumped down in January 2022 and has been decreasing ever since. And we have just shown that, for some reason, this decrease in fertility affected only the vaccinated. So, if you want to argue that a mysterious factor X is responsible for the drop in fertility, you will have to explain (1) why the factor affected only the vaccinated, and (2) why it started affecting them at about the time of vaccination. That is a tall order. Mr. Occam and I both think that X = the vaccine is the simplest explanation.
What really puzzles me is the continuation of the trend. If the vaccines really prevented conception, shouldn’t the effect have been transient? It’s been more than three years since the mass vaccination event, but fertility rates still keep falling. If this trend continues for another five years, we may as well stop arguing about pensions, defense spending, healthcare reform, and education – because we are done.
We are in the middle of what may be the biggest fertility crisis in the history of mankind. The reason for the collapse in fertility is not known. The governments of many European countries have the data that would unlock the mystery. Yet, it seems that no one wants to know.
Author
Addictions
More young men want to restrict pornography: survey

From LifeSiteNews
Nearly 64% of American men now believe online pornography should be more difficult to access, with even higher numbers of women saying the same thing.
A new survey has shown that an increasing number of young men want more restrictions on online pornography.
According to a survey by the American Enterprise Institute’s Survey Center on American Life, nearly 7 in 10 (69 percent) of Americans support the idea of making online pornography less accessible. In 2013, 65 percent expressed support for policies restricting internet pornography.
The most substantial increase in the support for restrictive measures on pornography could be observed in young men (age 18-24). In 2013, about half of young men favored restrictions, while 40 percent actively opposed such policies. In 2025, 64 percent of men believe accessing online pornography should be made more difficult.
The largest support for restriction on internet pornography overall could be measured among older men (65+), where 73 percent favored restrictions. An even larger percentage of women in each age group supported making online pornography less accessible. Seventy-two percent of young women (age 18-24) favored restriction, while 87 percent of women 55 years or older expressed support for less accessibility of internet pornography.
Viewing pornography is highly addictive and can lead to serious health problems. Studies have shown that children often have their first encounter with pornography at around 12 years old, with boys having a lower average age of about 10-11, and some encountering online pornography as young as 8. Studies have also shown that viewing pornography regularly rewires humans brains and that children, adolescents, and younger men are especially at risk for becoming addicted to online pornography.
According to Gary Wilson’s landmark book on the matter, “Your Brain on Porn,” pornography addiction frequently leads to problems like destruction of genuine intimate relationships, difficulty forming and maintaining real bonds in relationship, depression, social anxiety, as well as reduction of gray matter, leading to desensitization and diminished pleasure from everyday activities among many others.
-

 Also Interesting2 days ago
Also Interesting2 days ago9 Things You Should Know About PK/PD in Drug Research
-

 Business2 days ago
Business2 days ago‘Experts’ Warned Free Markets Would Ruin Argentina — Looks Like They Were Dead Wrong
-

 Business2 days ago
Business2 days agoCannabis Legalization Is Starting to Look Like a Really Dumb Idea
-

 Business2 days ago
Business2 days agoWEF-linked Linda Yaccarino to step down as CEO of X
-

 Media1 day ago
Media1 day agoCBC journalist quits, accuses outlet of anti-Conservative bias and censorship
-

 Business1 day ago
Business1 day agoCarney government should recognize that private sector drives Canada’s economy
-

 Bruce Dowbiggin1 day ago
Bruce Dowbiggin1 day agoThe Covid 19 Disaster: When Do We Get The Apologies?
-

 Automotive2 days ago
Automotive2 days agoAmerica’s EV Industry Must Now Compete On A Level Playing Field