Health
52-year-old grandfather the latest Canadian to choose euthanasia while waiting for cancer treatment

From LifeSiteNews
Dan Quayle’s wife believes that she could still have her husband today if he’d gotten the treatment he needed. In fact, wait times for cancer patients in Canada who are literally dying while waiting for treatment keep getting worse.
On October 7, 2023, Dan Quayle – a British Columbian, not the former vice president of the United States – turned 52. He was hoping to be told that he could begin chemotherapy after being diagnosed with esophageal cancer. It was not to be. “After 10 weeks in hospital, Quayle, a gregarious grandfather who put on his best silly act for his two grandkids, was in so much pain, unable to eat or walk, he opted for a medically assisted death on Nov. 24,” the National Post reported. “This was despite assurances from doctors that chemotherapy had the potential to prolong his life by a year.”
Throughout the agonizing wait, his family “prayed he would change his mind or get an 11th-hour call that chemo had been scheduled,” but were instead told consistently by the hospital that they were “backlogged.” The family is speaking out now “following the stories of two Vancouver Island women who went public with their decisions to seek treatment in the U.S. to avoid delays in B.C.” – and Dan’s wife believes that she could still have her husband today if he’d gotten the treatment he needed. In fact, wait times for cancer patients who are literally dying while waiting for treatment keep getting worse.
When Dan Quayle died by lethal injection, he still hadn’t been given a timeline for when he might get chemotherapy. It reminds me of the posthumously published obituary written by a Winnipeg woman who chose to die by assisted suicide after being refused the treatments she needed: “I could have had more time if I had more help.”
Indeed, one of the reasons Quayle felt that a lethal injection was his only option is because he didn’t have the financial resources to get help that was available elsewhere – but as a price. “If we had more money, we could have gone to the States,” his wife told the National Post sadly. “But we’re just regular people.”
She is likely referring to the two Vancouver Island women who decided to go public with their own experiences with the BC health care system. Global News published one story with the headline “B.C. woman gets surgery in U.S., says wait times at home could have cost her life” about Allison Ducluzeau, who paid $200,000 for surgery in the United States after she was told by a BC oncologist that she was not a candidate for the treatment that saved her life. After successfully getting treatment in the U.S., she recently got married – and is appalled by how she was treated in BC. In fact, she wasn’t offered life-saving treatment – but she was offered assisted suicide.
“There’s a lot of promises I’m hearing,” she told Global News. “But, you know, we need boots-on-the-ground action right now. What can you do to shorten these wait times? How can you prioritize cases so that people with aggressive stage four cancer get seen by someone and when they do get seen, they get offered treatment and not MAID like I was the first time?”
Another woman, 43-year-old Kristin Logan of Campbell River, was diagnosed with Stage 4 ovarian cancer – but faced a three or four month wait for treatment in British Columbia. She went to Washington State for chemotherapy, instead – she could afford it because the treatment was covered due to her dual citizenship and veteran status. When the health minister responded to her case by saying that the system “doesn’t always get it right,” she responded with fury: “To suggest that the system merely ‘doesn’t always get it right’ is a gross understatement, bordering on denial. Our healthcare system isn’t tripping over minor hurdles; it’s plummeting off a cliff. We’re not dealing with ‘occasional misses’; we’re grappling with a chronically diseased system where inefficiency and neglect have become the norm.”
What does this mean? It means that people are dying on waitlists – and while they suffer, often horribly, they are offered assisted suicide when they are their most vulnerable. And if the Trudeau Liberals get their way, in March of next year the floodgates will open and assisted suicide will also be available to those suffering with mental illness. Waitlists for mental health assistance and psychiatric care are even longer – I know people who have waited for years merely for an appointment. Many Canadians simply do not have access to this care. And so not only will Canadians die on waitlists; many will be offered assisted suicide while they are on waitlists, and many will, out of desperation, say yes.
Health
RFK Jr. Unloads Disturbing Vaccine Secrets on Tucker—And Surprises Everyone on Trump

The Vigilant Fox
This conversation with startle you, infuriate you—then lift your spirits
It’s not every day an active HHS Secretary sits down for 90 minutes straight with Tucker Carlson.
But that’s exactly what happened, and Kennedy instantly seized Carlson’s attention with a chilling story of CDC corruption.
He revealed that the health agency buried a 1999 internal study led by researcher Thomas Verstraten, which showed an alarming 1135% increase in autism risk from the hepatitis B vaccine.
Kennedy said the researchers were “shocked” by the findings.
So what did they do? They covered it up, according to Kennedy.
“They got rid of all the older children essentially and just had younger children who are too young to be diagnosed [with autism].”
RFK Jr. then explained the real reason why your pediatrician will kick you out of their practice for refusing vaccines.
“There’s a published article out there now that says that 50% of revenues to most pediatricians come from vaccines.”
It’s all about the money. The higher the vaccination rate, the bigger the bonus.
“And that’s why your pediatrician, if you say I want to go slow on the vaccines… will throw you out of his practice because you’re now jeopardizing that bonus structure.”
To the claim that the vaccine–autism link has been “debunked,” Kennedy had a message for Anderson Cooper, Jake Tapper, and everyone who smugly insists on it.
“None of the vaccines given to children in the first six months of life have ever been studied for autism.”
Let that sink in.
He went further, revealing that the CDC actually did find a link when they studied the DTaP vaccine.
But they dismissed it. Kennedy said they claimed it “didn’t count” because the data came from VAERS—the very system they use to track vaccine injuries.
So when the evidence pointed to harm, they simply claimed their own system wasn’t reliable enough and took no steps to fix it.
The vaccine corruption didn’t end there. Kennedy attested that the CDC killed off a vaccine injury reporting system that actually worked—because it worked too well.
It showed that 1 in 37 vaccines caused an injury.
Tucker was stunned.
“Of all vaccines?” he asked.
“Yeah,” Kennedy confirmed.
RFK Jr. explained that the CDC funded a study led by researcher Ross Lazarus. It compared a sophisticated machine-counting system to VAERS.
What did they find? VAERS was failing to catch over 99% of vaccine injuries.

The new system also revealed that 2.6% of all vaccinations resulted in an injury.
So what did the CDC do? They shut it down in 2010. And they’re still using VAERS today—even though it’s a completely inadequate system.

But Kennedy didn’t stop at old vaccine scandals. He also broke down Pfizer’s own COVID vaccine trial data. That trial showed a 23% higher death rate in the vaccinated group.
• Pfizer gave 21,720 people the vaccine and 21,728 the placebo.
• One vaccinated person died of COVID. Two placebo recipients died. They used this tiny difference to claim “100% effective” based on relative risk reduction.
• But in absolute terms, it took 22,000 vaccinations to save one life.
• Over six months, 21 vaccinated participants died of all causes, compared to 17 in the placebo group—a 23.5% higher death rate.
And then there’s vaccine spokesperson Paul Offit, often seen on CNN and other mainstream networks.
Kennedy shared an infuriating story about how he literally “voted himself rich” on the rotavirus vaccine.
While serving on the CDC’s ACIP committee, Offit voted to add rotavirus vaccination to the childhood schedule—even as he was developing his own competing vaccine. He guaranteed demand for his product.
The first approved rotavirus vaccine, RotaShield, was yanked from the market for causing dangerous intussusception. Offit’s vaccine, RotaTeq, eventually replaced it.
He and his partners later sold their rights to Merck for $186 million. As RFK Jr. said, Offit literally “voted himself rich.”
When Carlson mentioned Fauci, Kennedy revealed how Fauci funded research that helped scientists hide evidence of lab-made viruses.
The technique, called “seamless ligation,” allowed researchers to engineer viruses in a lab without leaving telltale genetic fingerprints.
RFK Jr. explained:
“One of his fundees, Ralph Baric, from the University of North Carolina, developed a technique called the seamless ligation technique, which is a technique for hiding the laboratory origins of a manipulated virus.”
“… normally if there’s a virus manipulated, researchers can look at the DNA sequences and they can say this thing was created in a lab. Ralph Baric had developed a technique that he called the no-see technique and its technical name was seamless ligation, and it was a way of hiding evidence of human tampering.”
He called it the exact opposite of what real public health work should be. Carlson cut in, saying, “That’s what you would do if you’re creating viruses for biological warfare.”
The conversation shifted to Trump, leading to one of the biggest highlights of the entire interview.
First, Kennedy explained that Trump chose his cabinet in an unorthodox way: he wanted to see three clips of each candidate performing on TV before considering them for the job.
“One of the things with President Trump is that he really knows how to pick talent… For every one of the positions that he picked, he wanted to see three clips of them performing on TV. He’s very conscious of the fact that these people are going to be out selling his program to the public,” Kennedy said.
That’s when Kennedy ended the interview with a bang, sharing his genuine thoughts about Trump for three straight minutes. It was one of the standout moments of the entire conversation.
If you’re on the fence about Trump, listen to Kennedy here. It might just change how you see him.
“I had him pegged as a narcissist, when narcissists are incapable of empathy. And he’s one of the most empathetic people that I’ve met,” Kennedy said.
“He’s immensely curious, inquisitive, and immensely knowledgeable. He’s encyclopedic in certain areas that you wouldn’t expect,” he continued.
Kennedy added that Trump genuinely cares about soldiers who go to war, citing how Trump “always talks about the casualties on both sides” of the Russia–Ukraine conflict.
“Whether it’s vaccines or Medicaid or Medicare, he’s always thinking about how this impacts the little guy. And the Democrats have him pegged as a guy who’s sort of sitting in the Cabinet meeting talking about how can we make billionaires richer. He’s the opposite of that. He’s a genuine populist,” Kennedy said.
There’s so much more in this conversation, and it might change the way you think about vaccines forever.
For the full picture, watch the entire interview below.
I also wanted to let you know I’m sharing a lot more than just posts like this throughout the day.
For quick clips and updates, check out my Substack Notes page.
Alongside my top 10 daily roundup, it’s one of the best ways to keep up with the news cycle.
Just download the Substack app and follow my page there to see content that doesn’t appear on this main page.
Subscribe to The Vigilant Fox
Business
National dental program likely more costly than advertised

From the Fraser Institute
By Matthew Lau
At the beginning of June, the Canadian Dental Care Plan expanded to include all eligible adults. To be eligible, you must: not have access to dental insurance, have filed your 2024 tax return in Canada, have an adjusted family net income under $90,000, and be a Canadian resident for tax purposes.
As a result, millions more Canadians will be able to access certain dental services at reduced—or no—out-of-pocket costs, as government shoves the costs onto the backs of taxpayers. The first half of the proposition, accessing services at reduced or no out-of-pocket costs, is always popular; the second half, paying higher taxes, is less so.
A Leger poll conducted in 2022 found 72 per cent of Canadians supported a national dental program for Canadians with family incomes up to $90,000—but when asked whether they would support the program if it’s paid for by an increase in the sales tax, support fell to 42 per cent. The taxpayer burden is considerable; when first announced two years ago, the estimated price tag was $13 billion over five years, and then $4.4 billion ongoing.
Already, there are signs the final cost to taxpayers will far exceed these estimates. Dr. Maneesh Jain, the immediate past-president of the Ontario Dental Association, has pointed out that according to Health Canada the average patient saved more than $850 in out-of-pocket costs in the program’s first year. However, the Trudeau government’s initial projections in the 2023 federal budget amounted to $280 per eligible Canadian per year.
Not all eligible Canadians will necessarily access dental services every year, but the massive gap between $850 and $280 suggests the initial price tag may well have understated taxpayer costs—a habit of the federal government, which over the past decade has routinely spent above its initial projections and consistently revises its spending estimates higher with each fiscal update.
To make matters worse there are also significant administrative costs. According to a story in Canadian Affairs, “Dental associations across Canada are flagging concerns with the plan’s structure and sustainability. They say the Canadian Dental Care Plan imposes significant administrative burdens on dentists, and that the majority of eligible patients are being denied care for complex dental treatments.”
Determining eligibility and coverage is a huge burden. Canadians must first apply through the government portal, then wait weeks for Sun Life (the insurer selected by the federal government) to confirm their eligibility and coverage. Unless dentists refuse to provide treatment until they have that confirmation, they or their staff must sometimes chase down patients after the fact for any co-pay or fees not covered.
Moreover, family income determines coverage eligibility, but even if patients are enrolled in the government program, dentists may not be able to access this information quickly. This leaves dentists in what Dr. Hans Herchen, president of the Alberta Dental Association, describes as the “very awkward spot” of having to verify their patients’ family income.
Dentists must also try to explain the program, which features high rejection rates, to patients. According to Dr. Anita Gartner, president of the British Columbia Dental Association, more than half of applications for complex treatment are rejected without explanation. This reduces trust in the government program.
Finally, the program creates “moral hazard” where people are encouraged to take riskier behaviour because they do not bear the full costs. For example, while we can significantly curtail tooth decay by diligent toothbrushing and flossing, people might be encouraged to neglect these activities if their dental services are paid by taxpayers instead of out-of-pocket. It’s a principle of basic economics that socializing costs will encourage people to incur higher costs than is really appropriate (see Canada’s health-care system).
At a projected ongoing cost of $4.4 billion to taxpayers, the newly expanded national dental program is already not cheap. Alas, not only may the true taxpayer cost be much higher than this initial projection, but like many other government initiatives, the dental program already seems to be more costly than initially advertised.
-

 Alberta12 hours ago
Alberta12 hours agoAlberta Independence Seekers Take First Step: Citizen Initiative Application Approved, Notice of Initiative Petition Issued
-
 Crime11 hours ago
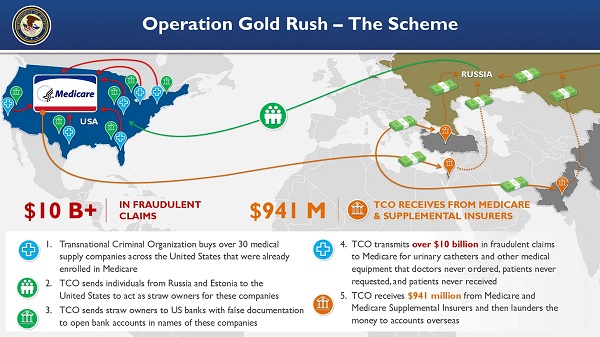
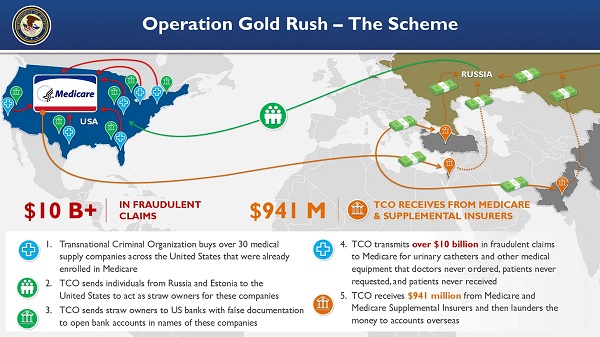
Crime11 hours agoNational Health Care Fraud Takedown Results in 324 Defendants Charged in Connection with Over $14.6 Billion in Alleged Fraud
-

 Health10 hours ago
Health10 hours agoRFK Jr. Unloads Disturbing Vaccine Secrets on Tucker—And Surprises Everyone on Trump
-

 Bruce Dowbiggin13 hours ago
Bruce Dowbiggin13 hours agoThe Game That Let Canadians Forgive The Liberals — Again
-

 Alberta1 day ago
Alberta1 day agoCOVID mandates protester in Canada released on bail after over 2 years in jail
-

 Business1 day ago
Business1 day agoCanada’s loyalty to globalism is bleeding our economy dry
-

 Crime2 days ago
Crime2 days agoProject Sleeping Giant: Inside the Chinese Mercantile Machine Linking Beijing’s Underground Banks and the Sinaloa Cartel
-

 armed forces1 day ago
armed forces1 day agoCanada’s Military Can’t Be Fixed With Cash Alone










