Fraser Institute
Virtual care will break the Canada Health Act—and that’s a good thing

From the Fraser Institute
The leadership of the Canadian Medical Association (CMA) is facing sharp criticism for its recent proposal to effectively ban private payment for virtual care. In a clear example of putting politics before patients, this would only erect additional barriers for those seeking care.
Moreover, it’s a desperate bid to cling to an outdated—and failed—model of health care while underestimating modern-day innovations.
Virtual care—online video doctor consultations—is a private-sector innovation. In response to our government system’s inability to provide timely care, private companies such as Maple have been offering these services to Canadians for almost a decade. In fact, the public system only pushed meaningfully into the virtual space during COVID when it established partnerships with these private companies alongside setting up new fee codes for virtual consultations.
In return for improving access to physician consultations for thousands of Canadians, these virtual care companies have been rewarded with increased government scrutiny and red tape. The weapon of choice? The Canada Health Act (CHA).
Specifically, sections 18 to 21 of the CHA prohibit user fees and extra billing for “medically necessary” services. Further, the insurance plan of a province must be publicly administered and provide “reasonable access” to 100 per cent of insured services. Provinces found in violation are punished by the federal government, which withholds a portion (or all) of federal health-care transfer payments.
Until recently, there had been no obvious conflict between the CHA and privately paid-for virtual care—primarily because the provinces are free to determine what’s medically necessary. Until recently, many provinces did not even have billing codes for virtual care. As virtual services are increasingly provided by the public sector, however, the ability to innovatively provide care for paying patients (either out-of-pocket or through private insurance) becomes restricted further.
Within this context, the CMA recently recommended formally including virtual care services within the public system, alongside measures to ensure “equitable access.” At the same time, it reiterated its recommendation that private insurance to access medically necessary services covered by the CHA be prohibited.
See where this is going?
The kicker is an additional recommendation banning dual practice (i.e. physicians working in both the public and private sector) except under certain conditions. This means doctors in the public system who could otherwise allocate their spare hours to private appointments online would now have to choose to operate exclusively in either the public or private system.
The combined effect of these policies would ensure that innovative private options for virtual care—whether paid for out-of-pocket or though private insurance—will either be overtaken by bureaucracies or disappear entirely.
But what the CMA report fails to recognize is that virtual care has expanded access to services the government fails to provide—there’s little reason to suspect a government takeover of the virtual-care sector will make things better for patients. And even if governments could somehow prevent Canadian doctors and companies providing these services privately, virtual care is not beholden to Canada’s physical borders. Patients with a little bit of technical knowhow will simply bypass the Canadian system entirely by having virtual consultations with doctors abroad. If Canadians can figure out how to access their favourite show in another country, you can be sure they’ll find a way to get a consultation with a doctor in Mumbai instead of Montreal.
Instead of forcing physicians and patients to operate within the crumbling confines of government-run health care, the CMA’s leadership should be grateful for the pressure valve that the private sector has produced. We should celebrate the private innovators who have provided Canadians better access to health care, not finding ways to shut them down in favour of more government control.
Author:
Business
Clean energy transition price tag over $150 billion and climbing, with very little to show for it
From the Fraser Institute
By Jake Fuss, Julio Mejía, Elmira Aliakbari, Karen Graham and Jock Finlayson
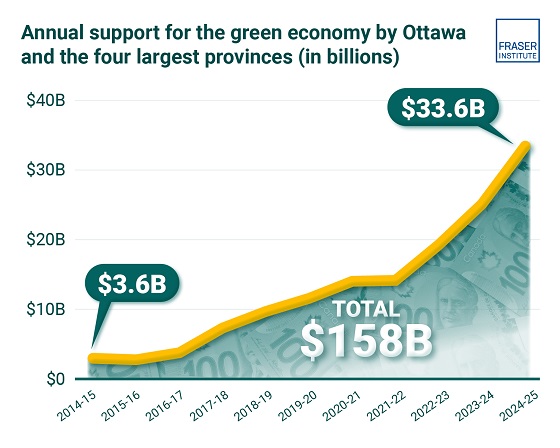
Ottawa and the four biggest provinces have spent (or foregone revenues) of at least $158 billion to create at most 68,000 “clean” jobs since 2014
Despite the hype of a “clean” economic transition, governments in Ottawa and in the four largest provinces have spent or foregone revenues of more than $150 billion (inflation-adjusted) on low-carbon initiatives since 2014/15, but have only created, at best, 68,000 clean jobs, according to two new studies published by the Fraser Institute, an independent, non-partisan Canadian public policy think-tank.
“Governments, activists and special interest groups have been making a lot of claims about the opportunities of a clean economic transition, but after a decade of policy interventions and more than $150 billion in taxpayers’ money, the results are
extremely underwhelming,” said Elmira Aliakbari, director of natural resource studies and co-author of The Fiscal Cost of Canada’s Low-Carbon Economy.
The study finds that since 2014/15, the federal government and provincial governments in the country’s four largest provinces (Ontario, Quebec, Alberta and British Columbia) combined have spent and foregone revenues of $158 billion (inflation adjusted to 2024 dollars) trying to create clean jobs, as defined by Statistics Canada’s Environmental and Clean Technology Products Economic Account.
Importantly, that cost estimate is conservative since it does not account for an exhaustive list of direct government spending and it does not measure the costs from Canada’s other six provinces, municipalities, regulatory costs and other economic
costs because of the low-carbon spending and tax credits.
A second study, Sizing Canada’s Clean Economy, finds that there was very little change over the 2014 to 2023 period in terms of the share of the total economy represented by the clean economy. For instance, in 2014, the clean economy represented 3.1 per cent of GDP compared to 3.6 per cent in 2023.
“The evidence is clear—the much-hyped clean economic transition has failed to fundamentally transform Canada’s $3.3 trillion economy,” said study co-author and Fraser Institute senior fellow Jock Finlayson.
State of the Green Economy
- The Fiscal Cost of Canada’s Low-Carbon Economy documents spending initiatives by the federal government and the governments of Ontario, British Columbia, Alberta, and Quebec since 2014 to promote the low-carbon economy, as well as how much revenue they have foregone through offering tax credits.
- Overall, the combined cost of spending and tax credits supporting a low-carbon economy by the federal government and the four provincial governments is estimated at $143.6 billion from 2014–15 to 2024–25, in nominal terms. When adjusted for inflation, the total reaches $158 billion in 2024 dollars.
- These estimates are based on very conservative assumptions, and they do not cover every program area or government-controlled expenditure related to the low-carbon economy and/or reducing greenhouse gas emissions.
- Sizing Canada’s Green Economy assesses the composition, growth, share of Gross Domestic Product (GDP) output, and employment of Canada’s “clean economy” from 2014 to 2023.
- Canada’s various environmental and clean technology industries collectively have accounted for between 3.07% and 3.62% of all-industry GDP over the 10-year period from 2014 to 2023. While it has grown, the sector as a whole has not been expanding at a pace that meaningfully exceeds the growth of the overall Canadian economy, despite significant policy attention and mounting public subsidies.
- The clean economy represents a respectable and relatively stable share of Canada’s $3.3 trillion economy. However, it remains a small part of Canada’s broader industrial mix, it is not a major source of export earnings, and it is not about to supplant the many other industries that underpin the country’s prosperity and dominate its international exports.
Alberta
Petition threatens independent school funding in Alberta

From the Fraser Institute
Recently, amid the backdrop of a teacher strike, an Alberta high school teacher began collecting signatures for a petition to end government funding of independent schools in the province. If she gets enough people to sign—10 per cent of the number of Albertans who voted in the last provincial election—Elections Alberta will consider launching a referendum about the issue.
In other words, the critical funding many Alberta families rely on for their children’s educational needs may be in jeopardy.
In Alberta, the provincial government partially funds independent schools and charter schools. The Alberta Teachers’ Association (ATA), whose members are currently on strike, opposes government funding of independent and charter schools.
But kids are not one-size-fits-all, and schools should reflect that reality, particularly in light of today’s increasing classroom complexity where different kids have different needs. Unlike government-run public schools, independent schools and charter schools have the flexibility to innovate and find creative ways to help students thrive.
And things aren’t going very well for all kids or teachers in government-run pubic school classrooms. According to the ATA, 93 per cent of teachers report encountering some form of aggression or violence at school, most often from students. Additionally, 85 per cent of unionized teachers face an increase in cognitive, social/emotional and behavioural issues in their classrooms. In 2020, one-quarter of students in Edmonton’s government-run public schools were just learning English, and immigration to Canada—and Alberta especially—has exploded since then. It’s not easy to teach a classroom of kids where a significant proportion do not speak English, many have learning disabilities or exceptional needs, and a few have severe behavioural problems.
Not surprisingly, demand for independent schools in Alberta is growing because many of these schools are designed for students with special needs, Autism, severe learning disabilities and ADHD. Some independent schools cater to students just learning English while others offer cultural focuses, expanded outdoor time, gifted learning and much more.
Which takes us back to the new petition—yet the latest attempt to defund independent schools in Alberta.
Wealthy families will always have school choice. But if the Alberta government wants low-income and middle-class kids to have the ability to access schools that fit them, too, it’s crucial to maintain—or better yet, increase—its support for independent and charter schools.
Consider a fictional Alberta family: the Millers. Their daughter, Lucy, is struggling at her local government-run public school. Her reading is below grade level and she’s being bullied. It’s affecting her self-esteem, her sleep and her overall wellbeing. The Millers pay their taxes. They don’t take vacations, they rent, and they haven’t upgraded their cars in many years. They can’t afford to pay full tuition for Lucy to attend an independent school that offers the approach to education she needs to succeed. However, because the Alberta government partially funds independent schools—which essentially means a portion of the Miller family’s tax dollars follow Lucy to the school of their choice—they’re able to afford the tuition.
The familiar refrain from opponents is that taxpayers shouldn’t pay for independent school tuition. But in fact, if you’re concerned about taxpayers, you should encourage school choice. If Lucy attends a government-run public school, taxpayers pay 100 per cent of her education costs. But if she attends an independent or charter school, taxpayers only pay a portion of the costs while her parents pay the rest. That’s why research shows that school choice saves tax dollars.
If you’re a parent with a child in a government-run public school in Alberta, you now must deal with another teacher strike. If you have a child in an independent or charter school, however, it’s business as usual. If Albertans are ever asked to vote on whether or not to end government funding for independent schools, they should remember that students are the most important stakeholder in education. And providing parents more choices in education is the solution, not the problem.
-

 Business2 days ago
Business2 days agoThe painful return of food inflation exposes Canada’s trade failures
-

 Business14 hours ago
Business14 hours agoTrans Mountain executive says it’s time to fix the system, expand access, and think like a nation builder
-

 Business2 days ago
Business2 days agoCBC uses tax dollars to hire more bureaucrats, fewer journalists
-
 Business1 day ago
Business1 day agoPaying for Trudeau’s EV Gamble: Ottawa Bought Jobs That Disappeared
-

 National2 days ago
National2 days agoElection Officials Warn MPs: Canada’s Ballot System Is Being Exploited
-

 Alberta2 days ago
Alberta2 days agoCoutts border officers seize 77 KG of cocaine in commercial truck entering Canada – Street value of $7 Million
-

 Bruce Dowbiggin2 days ago
Bruce Dowbiggin2 days agoIs Roundball A Square Game? Sports Betting Takes Another Hit
-

 Alberta1 day ago
Alberta1 day agoPremier Smith sending teachers back to school and setting up classroom complexity task force












