COVID-19
Dr. Peter McCullough Part 1: Thousands of doctors are treating covid. What you need to know to help you stay out of hospital.
In countries around the world, doctors have found that treating COVID patients at home quickly when symptoms develop leads to better outcomes, dramatically lower death rates than if doctors send people home to wait until they are so sick they need hospitalizations, ICU admissions, mechanical ventilators and even dialysis when kidneys fail.
If you’ve been unaware of the extent to which many doctors already know about early treatment the following videos will be incredibly informative. These videos are exerts from a longer interview by Dr. Alfred Johnson from a medical group in the United States which was published August 20
There’s another way to end the pandemic. Doctors can knock covid out with treatment
Why aren’t more doctors treating covid? Doctor testifies early treatment saves lives
Business
Conservatives demand probe into Liberal vaccine injury program’s $50m mismanagement

From LifeSiteNews
The Liberals’ Vaccine Injury Support Program is accused of mismanaging a $50-million contract with Oxaro Inc. and failing to resolve claims for thousands of vaccine-injured Canadians.
Conservatives are calling for an official investigation into the Liberal-run vaccine injury program, which has cost Canadians millions but has little to show for it.
On July 14th, four Conservative Members of Parliament (MPs) signed a letter demanding answers after an explosive Global News report found the Liberals’ Vaccine Injury Support Program (VISP) misallocated taxpayer funds and disregarded many vaccine-injured Canadians.
“The federal government awarded a $50 million taxpayer-funded contract to Oxaro Inc. (formerly Raymond Chabot Grant Thornton Consulting Inc.). The purpose of this contract was to administer the VISP,” the letter wrote.
“However, there was no clear indication that Oxaro had credible experience in healthcare or in the administration of health-related claims raising valid questions about how and why this firm was selected,” it continued.
Canada’s VISP was launched in December 2020 after the Canadian government gave vaccine makers a shield from liability regarding COVID-19 jab-related injuries.
However, mismanagement within the program has led to many injured Canadians still waiting to receive compensation, while government contractors grow richer.
“Despite the $50 million contract, over 1,700 of the 3,100 claims remain unresolved,” the Conservatives continued. “Families dealing with life-altering injuries have been left waiting years for answers and support they were promised.”
Furthermore, the claims do not represent the total number of Canadians injured by the allegedly “safe and effective” COVID shots, as inside memos have revealed that the Public Health Agency of Canada (PHAC) officials neglected to report all adverse effects from COVID shots and even went as far as telling staff not to report all events.
The PHAC’s downplaying of vaccine injuries is of little surprise to Canadians, as a 2023 secret memo revealed that the federal government purposefully hid adverse effect so as not to alarm Canadians.
Of the $50.6 million that Oxaro Inc., has received, $33.7 million has been spent on administrative costs, compared to only $16.9 million going to vaccine-injured Canadians.
The letter further revealed that former VISP employees have revealed that the program lacked professionalism, describing what Conservatives described as “a fraternity house rather than a professional organization responsible for administering health-related claims.”
“Reports of constant workplace drinking, ping pong, and Netflix are a slap in the face to taxpayers and the thousands of Canadians waiting for support for life altering injuries,” the letter continued.
Regardless of this, the Liberal government, under Prime Minister Mark Carney, is considering renewing its contract with Oxaro Inc.
Indeed, this would hardly be the first time that Liberals throw taxpayer dollars at a COVID program that is later exposed as ineffective and mismanaged.
Canada’s infamous ArriveCan app, which was mandated for all travelers in and out of Canada in 2020, has cost Canadians $54 million, despite the Public Health Agency of Canada admitting that they have no evidence that the program saved lives.
Details regarding the app and the government contracts surrounding it have been hidden from Canadians, as Liberals were exposed in 2023 for hiding a RCMP investigation into the app from auditors.
An investigation of the ArriveCan app began in 2022 after the House of Commons voted 173-149 for a full audit of the controversial app.
COVID-19
Trump DOJ dismisses charges against doctor who issued fake COVID passports

From LifeSiteNews
Attorney General Pam Bondi has ended the federal prosecution of Dr. Michael Kirk Moore for giving ‘patients a choice when the federal government refused to do so.’
The Utah plastic surgeon who issued fake COVID-19 vaccine passports to help patients get around COVID vaccine mandates will no longer be prosecuted, U.S. Attorney General Pam Bondi announced Saturday.
During the COVID pandemic, Dr. Michael Kirk Moore Jr. and employees at his Salt Lake private practice developed a plan to provide patients who objected to being forced to take the vaccine with ineffectual, harmless saline injections instead and give them COVID vaccination cards that would satisfy (since rescinded) mandates to take the shot as a condition of employment, public facilities, mass gatherings, and more.
For his efforts, he was indicted for allegedly “endanger[ing] the health and well-being of a vulnerable population” and “undermin[ing] public trust and the integrity of federal health care programs.” The government also accused him of doing so for profit, but several sources attested off the record that Moore not only issued the cards for free but actually refused offers of compensation.
“They broke no laws and harmed no person,” the defendants’ legal team said in 2023. “Dr. Moore, specifically, abided by his long held Hippocratic oath to First Do No Harm. We believe he and his co-defendants will be found innocent of all charges.”
Last month, LifeSiteNews reported that Moore’s trial was set to begin on July 7, which could have potentially ended with him facing 35 years in jail and a $125,000 penalty. Supporters of the doctor had expressed worry that the change in presidential administration had not yet halted the prosecution.
Over the weekend, however, Bondi announced that at her direction it has now done exactly that.
“Dr. Moore gave his patients a choice when the federal government refused to do so,” she said. “He did not deserve the years in prison he was facing. It ends today.”
There is a large body of warning signs against the shots, which were developed in record time by the first Trump administration’s Operation Warp Speed initiative.
The federal Vaccine Adverse Event Reporting System (VAERS) reports 38,709 deaths, 221,030 hospitalizations, 22,331 heart attacks, and 28,966 myocarditis and pericarditis cases as of June 27, among other ailments. U.S. Centers for Disease Control & Prevention (CDC) researchers have recognized a “high verification rate of reports of myocarditis to VAERS after mRNA-based COVID-19 vaccination,” leading to the conclusion that “under-reporting is more likely” than over-reporting.
An analysis of 99 million people across eight countries published in the journal Vaccine “observed significantly higher risks of myocarditis following the first, second and third doses” of mRNA-based COVID vaccines, as well as signs of increased risk of “pericarditis, Guillain-Barré syndrome, and cerebral venous sinus thrombosis,” and other “potential safety signals that require further investigation.”
In April 2024, the U.S. Centers for Disease Control & Prevention (CDC) was forced to release by court order 780,000 previously undisclosed reports of serious adverse reactions, and a study out of Japan found “statistically significant increases” in cancer deaths after third doses of mRNA-based COVID-19 vaccines, and offered several theories for a causal link.
In January, a long-awaited Florida grand jury report on the COVID vaccine manufacturers found that while only a miniscule percentage of the millions of vaccinations resulted in serious harm based on the data it had access to, such events do occur, and there are “profound and serious issues” in pharmaceutical companies’ review process, including reluctance to share what evidence of adverse events they did find.
In May, Trump administration U.S. Food & Drug Administration (FDA) Commissioner Dr. Marty Makary and vaccine chief Dr. Vinay Prasad announced that there would no longer be blanket recommendations for all Americans to receive the shot, but the “risk factors” it would still be recommended for include asthma, cancer, cerebrovascular disease, chronic kidney diseases, a handful of chronic liver and lung diseases, diabetes, disabilities such as Down’s syndrome, heart conditions, HIV, dementia, Parkinson’s, obesity, smoking, tuberculosis, and more. Health & Human Services (HHS) Secretary Robert F. Kennedy Jr. subsequently announced COVID vaccines will not be recommended to healthy children or pregnant women.
The Trump administration has approved a new mRNA-based COVID-19 vaccine from Moderna, suggesting the federal government’s overall view of the shots will remain favorable, albeit without mandates of any kind. At the same time, it does require mRNA COVID shots to carry a new warning about the danger of heart damage in young men.
-

 Addictions1 day ago
Addictions1 day agoWhy B.C.’s new witnessed dosing guidelines are built to fail
-

 Frontier Centre for Public Policy2 days ago
Frontier Centre for Public Policy2 days agoCanada’s New Border Bill Spies On You, Not The Bad Guys
-
 Business1 day ago
Business1 day agoCarney Liberals quietly award Pfizer, Moderna nearly $400 million for new COVID shot contracts
-

 Energy2 days ago
Energy2 days agoCNN’s Shock Climate Polling Data Reinforces Trump’s Energy Agenda
-
 Opinion1 day ago
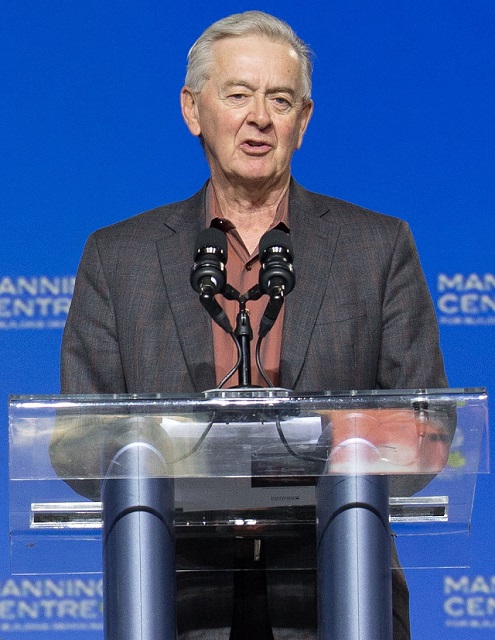
Opinion1 day agoPreston Manning: Three Wise Men from the East, Again
-

 Opinion1 day ago
Opinion1 day agoCharity Campaigns vs. Charity Donations
-

 Business1 day ago
Business1 day agoMark Carney’s Fiscal Fantasy Will Bankrupt Canada
-

 Red Deer1 day ago
Red Deer1 day agoWesterner Days Attraction pass and New Experiences!





