Brownstone Institute
The Vaccine Narrative Is as Leaky as the Vaccines

BY
Let’s start with two simple questions. If regulators had the information available to them of the leakage between Covid-19 efficacy rates in controlled trials and their effectiveness in the real world, would they still grant emergency use authorization? Would their legal framework permit them to do so?
Remember, all laws serve a dual purpose. On the one hand, they are permissive and enabling, granting powers to do certain things. On the other, they are limiting and restrictive, ring-fencing what may lawfully be done even by the state.
Second, is Denmark being ruled by an anti-vaxxer government and health authority? From July 1 Denmark, which has an excellent health infrastructure including data collection, banned under-18s from being vaccinated and in mid-September the ban was extended to boosters for under-50s, other than in exceptional circumstances for immunocompromised and high-risk individuals in both cases.
The explanation offered by the health authorities is interesting both for what they said and what they did not say. They anticipate a rise in Covid-19 infections over autumn and winter and “aim to prevent serious illness, hospitalisation and death.” This risk applies to 50-year olds and above and not those younger. Because the vaccines are not meant to prevent infection, they will no longer be offered to the under-50s.
However, governments don’t ban products merely because they are not beneficial. Bans apply only to products that inflict harms. So the unstated reality is the benefit: harm ratio is no longer favorable. The really interesting question therefore is: why don’t they say so? The empirical data from around the world demonstrates negligible to negative vaccine effectiveness for healthy under-50s and greater risk of serious adverse events. Denmark’s decision marks official if implicit acknowledgment that harms are greater than benefits.
Baffling Origins of Lockdown
The lockdowns across the Western world remain, to me, inexplicable and baffling. The abandonment of a century’s worth of cumulative scientific knowledge and global and national pandemic preparedness plans were based neither on new science nor emerging data.
Rather, they were based firstly on apocalyptic modelling using flawed assumptions and secondly on dubious data from China whose authoritarian policies played to innate instincts in our own health bureaucrats and politicians, cheered on by the mainstream media. In a further nod to anti-scientific groupthink conformism, critical and contrarian voices within the health and political establishments were silenced and exorcised. Outside government, they were vilified and expelled from the public square in active collusion with the social media tech giants.
In February 2020, when the cruise ship Diamond Princess docked in Yokohama with 3,711 people on board, Kentaro Iwata, an infectious diseases expert at Kobe University, described it as a “Covid-19 mill.” Outbreaks seed easily on cruise ships because of the high numbers of susceptible elderly passengers living and socializing in confined quarters.
Even under these worst possible conditions, under one-fifth of the captive population was infected, a small number of the infected died and 98.2% recovered. Using age-adjusted data, Oxford University’s Centre for Evidence-Based Medicine estimated the infection fatality rate (IFR) of 0.5% and a case fatality rate (CFR) of 1.1% on the Diamond Princess and, as of March 26, 2020, a global IFR of approximately 0.20% (compared to the seasonal flu’s 0.1% and the Spanish flu’s >2.5% which killed mostly people in the 20–40 age bracket). Reassuringly, even for the over-70s without comorbidities, the IFR was below 1%.
All this ‘bullet proof’ data was thrown out in favor of completely unreliable data and fake videos from China that were then fed into mathematical modelling to produce apocalyptic scenarios that in turn were treated as forecasts by the media and governments. Madness.
India’s Experience: Vaccines Are Not Necessary for Beating Back Covid

India’s experience in mid-2021 proved that vaccines are not necessary for rapid mass recovery from a virulent Covid wave. Anyone who has followed the Covid narrative will remember the horrific pictures in spring-summer 2021 with bodies floating ashore on riverbanks and piling up in cremation grounds. The gradient was broadly similar during the curve’s ascent and descent, with the death rate reaching 1.06 per million people on April 20, peaking at 2.98 on May 21 and 23 and falling back to 1.00 on June 24 (Figure 1). On those three dates India’s full vaccination coverage was 1.26%, 2.96% and 3.53% of the population, respectively.
People questioned the reliability of the data, openly asserting a vast undercount in order to cushion the political embarrassment. Knowing something of India, I disagree and noted more than a hint of racism in the coverage. No matter. Even if the authorities deliberately suppressed the rising numbers of dead, it would be absurd to suggest they did the same with the downward numbers. The symmetrical rise and fall is consistent with the experience of most countries with successive waves of the virus. Whatever else might explain the fall, it certainly wasn’t high vaccination coverage. Herd immunity to the then-dominant Delta variant through a mix of uncontrolled infections and modest vaccination, possibly.
Another contender for the explanation is the widespread use of ivermectin. Mid-crisis in May last year, the state government of Uttar Pradesh (India’s most populous state with 200 million people!), boasted it had been the first to authorize large-scale prophylactic and therapeutic use of ivermectin against Covid-19 in May–June 2020. Studies were confirming that “the drug helped the state to maintain a lower fatality and positivity rate as compared to other states.”
A meta-analysis by Andrew Bryant and Tess Lawrie in the American Journal of Therapeutics of 24 randomized control trials (RCTs) in 15 countries (one of which was subsequently pulled as possibly fraudulent) concluded that ivermectin significantly helps to prevent and treat Covid-19 and, with a 62% mortality reduction, can potentially save millions of lives. They published a follow-up analysis in the same journal that removed the suspect study and the results still showed robust ivermectin efficacy.
An analysis of seven RCTs, covering 1,327 patients, by Swedish physician Sebastian Rushworth found “a 62% reduction in the relative risk of dying among Covid patients treated with ivermectin.” A recent large-scale study from Brazil published on August 31 found that, compared to regular users, non-use of ivermectin increased the risk of Covid-related mortality by 12.5 times and dying from Covid by seven times.
Yet for some strange reason, Western health bureaucracies would neither recommend ivermectin – a low cost, off patent and no profit drug for Big Pharma – nor fund a rigorous but fair (that is, not designed to fail) clinical assessment of its efficacy against Covid. It had morphed into Voldermectin: the drug that must not be named.
Global Experience: Vaccines Are Not Sufficient to Beat Back Covid
My earlier articles show why Australia’s Covid numbers this year demonstrate that vaccines are not sufficient to prevent mass infections, hospitalization and deaths either. Steve Kirsch alerted his Substack subscribers on September 17 to an internal report for the governing Liberal Party of Canada back in June. It makes for depressing reading that will come as no surprise to all of us who have grown increasingly cynical about public health authorities and governing elites. The report draws on official Ontario data, is informed by wide international scholarship and emphasizes that the empirical results are in line with trends in other Canadian provinces and countries.
The fully vaccinated show rise in hospital admissions within 5-6 months; the boosted, within two weeks and rising thereafter for several months. Immunity through natural infection can last up to 20 months. Vaccination shows considerable benefits to over-70s and some benefit to over-60s but virtually no benefit to under-60s with respect to hospitalization and mortality rates. By contrast, adverse events are concentrated in the 18–69 age groups, and especially, in order of most to least, in the 40–49, 50–59 and 30–39 age groups.
Because the “abundance of data” demonstrates that vaccines do not prevent infection, transmission, hospitalization and deaths for the under-60s, “public health policy tools such as, mass vaccination campaigns, mandates, passports and travel restrictions need to be re-evaluated for relevance.” Factoring in also “known adverse events and unknown long-term effects,” the “empirical evidence investigated in this report … does not support continuing mass vaccination programs, mandates, passports and travel bans for all age groups.” The government has sat on this report since June – what a surprise.
Meanwhile there continues to be very little evidence in the real world that countries with high rates of multiple vaccine doses suffer correspondingly lower rates of Covid-19 mortality (Figures 2 and 3). In the two charts, Chile has both the highest booster rollout and the highest Covid-related death rate per capita, while India has the lowest booster coverage yet the second lowest mortality rate.


Some experts point to a worrying trend of rising excess mortality among under-14s in 28 European countries. An article in Vaccine – downloaded more than 110,000 times in preprint – seems to suggest, albeit tentatively, that added risks of serious adverse events are 2.4 and 4.4 times higher than the reduced risk of hospitalization for Moderna and Pfizer vaccines, respectively. Cautioning that the harm-benefit ratio will vary with populations at different Covid risk profiles and in different time periods from the Moderna and Pfizer studies they analyzed, the authors conclude with the need for large, randomized trials to come to robust conclusions. It would help if Moderna and Pfizer would release the granular, individual level data in their possession.
In a follow-up note on Substack, two of the study’s authors note that the normal rate of adverse events for other vaccines is 1-2 per million. The swine flu vaccine (1976) was pulled after it was associated with Guillain-Barre Syndrome at a 1 in 100,000 rate. By comparison, the Pfizer and Moderna clinical trials show 125 adverse events per 100,000 vaccinated people, while preventing between 22-63 hospitalizations.
Another new study of almost 900,000 5-11-year-old children in North Carolina, published in the New England Journal of Medicine, adds to concerns that vaccines don’t just lose their effectiveness in just a few months; they also destroy natural immunity against reinfection severe enough to put them in hospital.
Panels C and D (the study’s authors use “Panel” rather than “Chart”) clearly show that among people infected by the Delta variant, protection against reinfection of the unvaccinated lasts longer than of the vaccinated. The former’s effectiveness was still above 50% eight months later in May 2022 while the latter’s had fallen to zero (Figure 4). But with the Omicron variant, the previously infected are slightly better off vaccinated than unvaccinated after two months (94.3:90.7%) and much better off after four months (73.8:62.9%). The likely, albeit not definitive, explanation is that the vaccines themselves are destroying the protection provided by natural immunity.


Three comments about Panels E and F (Figure 5). First, while the x axis for Panel E is in weeks, Panel F’s is in months. So the first visual impression is misleading. Second, the maximum effectiveness of a vaccine against a reinfection severe enough to require hospital admission is around 88%, reached approximately four weeks after the first dose is administered. By contrast, the initial effectiveness of a previous infection is 100% and remains above 95% (remember the vaccine’s much-touted 95% efficacy rate?) until seven months later.
Third, the effectiveness of a previous infection against reinfection requiring hospitalisation does not decline to the same level as the vaccine’s peak effectiveness until nine months after infection. This is the reality that the CDC denied until recently and used as the justification for discriminating between the vaccinated and unvaccinated for access to public spaces.
Three conclusions follow:
- The risk of severe outcomes for children from infection by current Covid variants is low;
- The risk of severe adverse reactions from vaccines is higher, meaning vaccination is a net harm for young children – exactly why Denmark has banned them for children;
- Exposing healthy children to the risk of infection may be better for both individual and herd immunity than mass vaccinating them.
The FDA is not likely to restore its credibility as the US regulator with the widely ridiculed revelation that the new bivalent boosters were authorized on the basis of trial results from eight mice. Professor Marty Makary from the Johns Hopkins School of Public Health tweeted his concerns about this and also about the announcement of an annual Covid vaccine that is not data-driven and ignores natural immunity as well as the risks of immune imprinting (where the immune system remembers its initial response to infection or vaccination in a way that usually, but not always, weakens the response to future variants of the same pathogen) from a multi-dose vaccination strategy.
From mRNA Vaccine Hesitant to Anti Vaxxer
The Financial Times – as mainstream establishment as they come – recently warned that the US decision to roll out new booster shots without clinical testing on humans – already dubbed the mouse vaccine by some – risks undermining public trust and deepening vaccine hesitancy. “We already have a trust problem in this country and we don’t need to make it worse,” Eric Topol, founder and director of the Scripps Research Translational Institute, said. Yet, even while bemoaning the loss of public trust in health experts and institutions, Topol just couldn’t help himself and smeared the Covid vaccine hesitants and sceptics as “anti-vaxxers, anti-science” people.
He thereby demonstrates precisely the pathology so beautifully described by Julie Sladden in an article in Spectator Australia on September 8. The Tasmanian doctor, “Having probably received more vaccines than most, given I am both a doctor and fairly well travelled,” used to begin her apology for refusing the Covid jab with “‘I’m no anti-vaxxer!’” However, after two years of “government-endorsed segregation and dehumanisation of those who exercised their right to refuse the jab,” she has changed her mind.
If an “anti-vaxxer” is someone who cannot give informed consent to a “vaccine” that fails to prevent infection or transmission, has alarming safety signals, must be taken to earn back the right to live and work in society, for a disease that has a greater-than 99 per cent survivability rate, then “yes,” I’m an anti-vaxxer… My government made it so.
To this we should add the very high likelihood of crossover vaccine hesitancy to other vaccines. In my own case before the pandemic I have dutifully gone in for the annual flu shot strongly recommended for my age demographic. Not any more. The Covid experience killed my trust in the medical and public health establishment and, having done my own research, I now politely decline the annual pre-winter flu shot.
Brownstone Institute
Bizarre Decisions about Nicotine Pouches Lead to the Wrong Products on Shelves

From the Brownstone Institute
A walk through a dozen convenience stores in Montgomery County, Pennsylvania, says a lot about how US nicotine policy actually works. Only about one in eight nicotine-pouch products for sale is legal. The rest are unauthorized—but they’re not all the same. Some are brightly branded, with uncertain ingredients, not approved by any Western regulator, and clearly aimed at impulse buyers. Others—like Sweden’s NOAT—are the opposite: muted, well-made, adult-oriented, and already approved for sale in Europe.
Yet in the United States, NOAT has been told to stop selling. In September 2025, the Food and Drug Administration (FDA) issued the company a warning letter for offering nicotine pouches without marketing authorization. That might make sense if the products were dangerous, but they appear to be among the safest on the market: mild flavors, low nicotine levels, and recyclable paper packaging. In Europe, regulators consider them acceptable. In America, they’re banned. The decision looks, at best, strange—and possibly arbitrary.
What the Market Shows
My October 2025 audit was straightforward. I visited twelve stores and recorded every distinct pouch product visible for sale at the counter. If the item matched one of the twenty ZYN products that the FDA authorized in January, it was counted as legal. Everything else was counted as illegal.
Two of the stores told me they had recently received FDA letters and had already removed most illegal stock. The other ten stores were still dominated by unauthorized products—more than 93 percent of what was on display. Across all twelve locations, about 12 percent of products were legal ZYN, and about 88 percent were not.
The illegal share wasn’t uniform. Many of the unauthorized products were clearly high-nicotine imports with flashy names like Loop, Velo, and Zimo. These products may be fine, but some are probably high in contaminants, and a few often with very high nicotine levels. Others were subdued, plainly meant for adult users. NOAT was a good example of that second group: simple packaging, oat-based filler, restrained flavoring, and branding that makes no effort to look “cool.” It’s the kind of product any regulator serious about harm reduction would welcome.
Enforcement Works
To the FDA’s credit, enforcement does make a difference. The two stores that received official letters quickly pulled their illegal stock. That mirrors the agency’s broader efforts this year: new import alerts to detain unauthorized tobacco products at the border (see also Import Alert 98-06), and hundreds of warning letters to retailers, importers, and distributors.
But effective enforcement can’t solve a supply problem. The list of legal nicotine-pouch products is still extremely short—only a narrow range of ZYN items. Adults who want more variety, or stores that want to meet that demand, inevitably turn to gray-market suppliers. The more limited the legal catalog, the more the illegal market thrives.
Why the NOAT Decision Appears Bizarre
The FDA’s own actions make the situation hard to explain. In January 2025, it authorized twenty ZYN products after finding that they contained far fewer harmful chemicals than cigarettes and could help adult smokers switch. That was progress. But nine months later, the FDA has approved nothing else—while sending a warning letter to NOAT, arguably the least youth-oriented pouch line in the world.
The outcome is bad for legal sellers and public health. ZYN is legal; a handful of clearly risky, high-nicotine imports continue to circulate; and a mild, adult-market brand that meets European safety and labeling rules is banned. Officially, NOAT’s problem is procedural—it lacks a marketing order. But in practical terms, the FDA is punishing the very design choices it claims to value: simplicity, low appeal to minors, and clean ingredients.
This approach also ignores the differences in actual risk. Studies consistently show that nicotine pouches have far fewer toxins than cigarettes and far less variability than many vapes. The biggest pouch concerns are uneven nicotine levels and occasional traces of tobacco-specific nitrosamines, depending on manufacturing quality. The serious contamination issues—heavy metals and inconsistent dosage—belong mostly to disposable vapes, particularly the flood of unregulated imports from China. Treating all “unauthorized” products as equally bad blurs those distinctions and undermines proportional enforcement.
A Better Balance: Enforce Upstream, Widen the Legal Path
My small Montgomery County survey suggests a simple formula for improvement.
First, keep enforcement targeted and focused on suppliers, not just clerks. Warning letters clearly change behavior at the store level, but the biggest impact will come from auditing distributors and importers, and stopping bad shipments before they reach retail shelves.
Second, make compliance easy. A single-page list of authorized nicotine-pouch products—currently the twenty approved ZYN items—should be posted in every store and attached to distributor invoices. Point-of-sale systems can block barcodes for anything not on the list, and retailers could affirm, once a year, that they stock only approved items.
Third, widen the legal lane. The FDA launched a pilot program in September 2025 to speed review of new pouch applications. That program should spell out exactly what evidence is needed—chemical data, toxicology, nicotine release rates, and behavioral studies—and make timely decisions. If products like NOAT meet those standards, they should be authorized quickly. Legal competition among adult-oriented brands will crowd out the sketchy imports far faster than enforcement alone.
The Bottom Line
Enforcement matters, and the data show it works—where it happens. But the legal market is too narrow to protect consumers or encourage innovation. The current regime leaves a few ZYN products as lonely legal islands in a sea of gray-market pouches that range from sensible to reckless.
The FDA’s treatment of NOAT stands out as a case study in inconsistency: a quiet, adult-focused brand approved in Europe yet effectively banned in the US, while flashier and riskier options continue to slip through. That’s not a public-health victory; it’s a missed opportunity.
If the goal is to help adult smokers move to lower-risk products while keeping youth use low, the path forward is clear: enforce smartly, make compliance easy, and give good products a fair shot. Right now, we’re doing the first part well—but failing at the second and third. It’s time to fix that.
Addictions
The War on Commonsense Nicotine Regulation

From the Brownstone Institute
Cigarettes kill nearly half a million Americans each year. Everyone knows it, including the Food and Drug Administration. Yet while the most lethal nicotine product remains on sale in every gas station, the FDA continues to block or delay far safer alternatives.
Nicotine pouches—small, smokeless packets tucked under the lip—deliver nicotine without burning tobacco. They eliminate the tar, carbon monoxide, and carcinogens that make cigarettes so deadly. The logic of harm reduction couldn’t be clearer: if smokers can get nicotine without smoke, millions of lives could be saved.
Sweden has already proven the point. Through widespread use of snus and nicotine pouches, the country has cut daily smoking to about 5 percent, the lowest rate in Europe. Lung-cancer deaths are less than half the continental average. This “Swedish Experience” shows that when adults are given safer options, they switch voluntarily—no prohibition required.
In the United States, however, the FDA’s tobacco division has turned this logic on its head. Since Congress gave it sweeping authority in 2009, the agency has demanded that every new product undergo a Premarket Tobacco Product Application, or PMTA, proving it is “appropriate for the protection of public health.” That sounds reasonable until you see how the process works.
Manufacturers must spend millions on speculative modeling about how their products might affect every segment of society—smokers, nonsmokers, youth, and future generations—before they can even reach the market. Unsurprisingly, almost all PMTAs have been denied or shelved. Reduced-risk products sit in limbo while Marlboros and Newports remain untouched.
Only this January did the agency relent slightly, authorizing 20 ZYN nicotine-pouch products made by Swedish Match, now owned by Philip Morris. The FDA admitted the obvious: “The data show that these specific products are appropriate for the protection of public health.” The toxic-chemical levels were far lower than in cigarettes, and adult smokers were more likely to switch than teens were to start.
The decision should have been a turning point. Instead, it exposed the double standard. Other pouch makers—especially smaller firms from Sweden and the US, such as NOAT—remain locked out of the legal market even when their products meet the same technical standards.
The FDA’s inaction has created a black market dominated by unregulated imports, many from China. According to my own research, roughly 85 percent of pouches now sold in convenience stores are technically illegal.
The agency claims that this heavy-handed approach protects kids. But youth pouch use in the US remains very low—about 1.5 percent of high-school students according to the latest National Youth Tobacco Survey—while nearly 30 million American adults still smoke. Denying safer products to millions of addicted adults because a tiny fraction of teens might experiment is the opposite of public-health logic.
There’s a better path. The FDA should base its decisions on science, not fear. If a product dramatically reduces exposure to harmful chemicals, meets strict packaging and marketing standards, and enforces Tobacco 21 age verification, it should be allowed on the market. Population-level effects can be monitored afterward through real-world data on switching and youth use. That’s how drug and vaccine regulation already works.
Sweden’s evidence shows the results of a pragmatic approach: a near-smoke-free society achieved through consumer choice, not coercion. The FDA’s own approval of ZYN proves that such products can meet its legal standard for protecting public health. The next step is consistency—apply the same rules to everyone.
Combustion, not nicotine, is the killer. Until the FDA acts on that simple truth, it will keep protecting the cigarette industry it was supposed to regulate.
-
 Business2 days ago
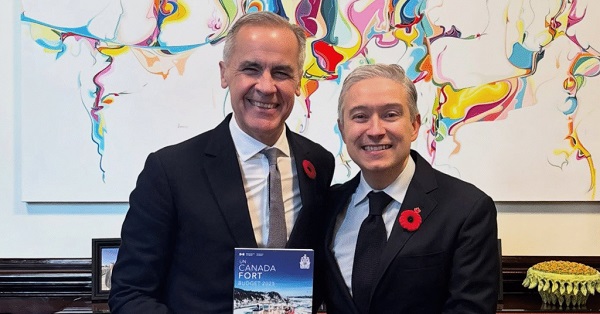
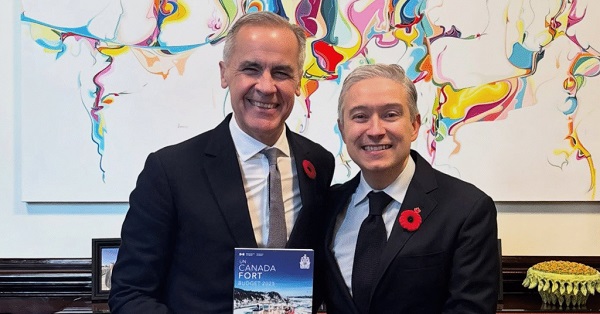
Business2 days agoCarney shrugs off debt problem with more borrowing
-
 Alberta2 days ago
Alberta2 days agoWhen Teachers Say Your Child Has Nowhere Else to Go
-

 Automotive2 days ago
Automotive2 days agoThe high price of green virtue
-

 Addictions2 days ago
Addictions2 days agoCanada is divided on the drug crisis—so are its doctors
-

 Bruce Dowbiggin2 days ago
Bruce Dowbiggin2 days agoMaintenance Mania: Since When Did Pro Athletes Get So Fragile?
-

 MAiD2 days ago
MAiD2 days agoQuebec has the highest euthanasia rate in the world at 7.4% of total deaths
-

 Daily Caller2 days ago
Daily Caller2 days agoProtesters Storm Elite Climate Summit In Chaotic Scene
-

 National1 day ago
National1 day agoConservative bill would increase penalties for attacks on places of worship in Canada












