Health
RFK Jr. Drops Stunning Vaccine Announcement
 The Vigilant Fox
The Vigilant Fox
This changes everything.
HHS Secretary Robert F. Kennedy Jr. just unveiled new reforms that could transform how this country treats vaccine injuries forever.
But before sharing the details with Chris Cuomo Thursday night, he exposed just how bad things really were inside the Department of Health and Human Services before he took charge.
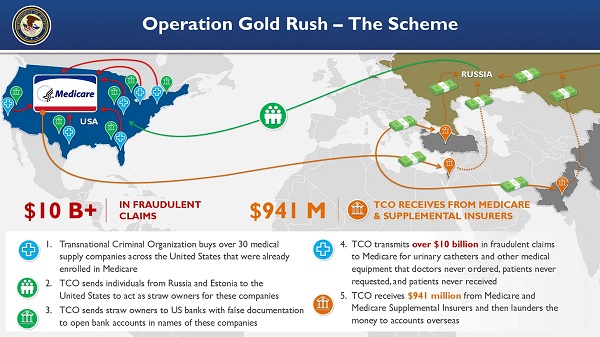
According to Kennedy, parts of HHS were “selling patient information to each other” and actively working against one another.
That means your private health data—funded by taxpayers—was being treated like a commodity inside the same agency that’s supposed to protect it.
But it gets even worse. Kennedy said when he tried to access CMS data—patient and billing records from Medicare and Medicaid—he was told HHS would have to buy it back from another branch of itself.
“So I tried to get the CMS patient information, which belongs to the American people and belongs to HHS, and the sub-agencies said we have to buy it from them, and it doesn’t make any sense. There are sub-agencies that refuse to give us patient data,” Kennedy lamented.
This kind of red tape, he argued, is exactly what’s prevented progress. But change is already in motion.
Kennedy pointed to DOGE—the Department of Government Efficiency—as one of the major drivers of reform.
“We’re going from 82,000 workers to 62,000. That’s tough on everybody. But I think in the long run we’re going to have much greater morale in a demoralized agency,” he said.
The vaccine injury news broke when Kennedy announced that the CDC is creating a new sub-agency focused entirely on vaccine injuries—a long-overdue shift for patients who’ve spent years searching for answers without any support from the government.
“We’re incorporating an agency within CDC that is going to specialize in vaccine injuries,” Kennedy announced.
“These are priorities for the American people. More and more people are suffering from these injuries, and we are committed to having gold-standard science make sure that we can figure out what the treatments are and that we can deliver the best treatments possible to the American people.”
For years, the vaccine-injured have felt ignored or dismissed, as public health agencies refused to even acknowledge the problem. Now, there’s finally an initiative underway to investigate their injuries and to provide support.
Kennedy also revealed a series of additional HHS reforms aimed at turning America’s health crisis around:
1. Operation Stork Speed
“We launched Operation Stork Speed to improve our capacity to have good, nutritious baby formula for the American public that doesn’t have heavy metals or other poisons in it,” Kennedy explained.
2. Eliminating Toxic Food Dyes
“We’ve met with the major food processors and told them we want chemical dyes out of all of our foods,” he added.
3. Cleaning up the SNAP program
Kennedy also pointed out that a huge portion of government food aid is going toward sugar-filled sodas—and it’s fueling a health crisis.
“Ten percent of SNAP is now spent on soda drinks, which are giving diabetes to children… 38% of American teens are now prediabetic or diabetic,” he lamented.
“We are reforming the SNAP program so that we’re not poisoning kids.”
The ultimate goal, Kennedy said, is to restore America’s health to what it was when he was a kid—before toxic food dyes, ultra-processed foods, and an out-of-control 72-dose vaccine schedule entered the picture.
“We’re reforming every part of the agency to make sure that our food supply is good and that we have the healthiest kids in the world, which we had when I was a kid.”
Whether you agree with him or not, Kennedy is doing more at HHS than any leader in recent memory—and for the first time in a long time, Americans injured by vaccines are finally being heard.
Thanks for reading! I hope this brought you the good news you needed to start your day.
If you like my work and want to support me, my family, and keep this page going, the most impactful thing you can do is to sign up for the newsletter and become a paid subscriber.
Your monthly subscription goes further than you think. Thank you so much for your support.
A little about me: I used to work in healthcare. But when the Biden administration pushed vaccine mandates, I couldn’t stay silent. My conscience led me to speak out—and that’s how this page was born.
Since then, I’ve shared thousands of videos featuring top doctors and scientists brave enough to challenge the official COVID narrative. Along the way, we’ve racked up billions of views and helped millions see the side of the story the government tried to keep hidden.
Now, I’m digging even deeper—breaking down expert interviews, firsthand accounts, and forgotten science to uncover what you haven’t been told about cancer, cholesterol, fasting, sunlight, and more.
If you’re tired of one-sided health messaging that always aligns with Big Pharma, follow me for easily digestible clips and insights about your health that you’re not hearing from the mainstream.
Follow on 𝕏: @VigilantFox
Telegram: t.me/VigilantFox
Email List: vigilantfox.com
Addictions
‘Over and over until they die’: Drug crisis pushes first responders to the brink

First responders say it is not overdoses that leave them feeling burned out—it is the endless cycle of calls they cannot meaningfully resolve
The soap bottle just missed his head.
Standing in the doorway of a cluttered Halifax apartment, Derek, a primary care paramedic, watched it smash against the wall.
Derek was there because the woman who threw it had called 911 again — she did so nearly every day. She said she had chest pain. But when she saw the green patch on his uniform, she erupted. Green meant he could not give her what she wanted: fentanyl.
She screamed at him to call “the red tags” — advanced care paramedics authorized to administer opioids. With none available, Derek declared the scene unsafe and left. Later that night, she called again. This time, a red-patched unit was available. She got her dose.
Derek says he was not angry at the woman, but at the system that left her trapped in addiction — and him powerless to help.
First responders across Canada say it is not overdoses that leave them feeling burned out — it is the endless cycle of calls they cannot meaningfully resolve. Understaffed, overburdened and dispatched into crises they are not equipped to fix, many feel morally and emotionally drained.
“We’re sending our first responders to try and manage what should otherwise be dealt with at structural and systemic levels,” said Nicholas Carleton, a University of Regina researcher who studies the mental health of public safety personnel.
Canadian Affairs agreed to use pseudonyms for the two frontline workers referenced in this story. Canadian Affairs also spoke with nine other first responders who agreed to speak only on background. All of these sources cited concerns about workplace retaliation for speaking out.
Moral injury
Canada’s opioid crisis is pushing frontline workers such as paramedics to the brink.
A 2024 study of 350 Quebec paramedics shows one in three have seriously considered suicide. Globally, ambulance workers have among the highest suicide rates of public service personnel.
Between 2017 and 2024, Canadian paramedics responded to nearly 240,000 suspected opioid overdoses. More than 50,000 of those were fatal.
Yet many paramedics say overdose calls are not the hardest part of the job.
“When they do come up, they’re pretty easy calls,” said Derek. Naloxone, a drug that reverses overdoses, is readily available. “I can actually fix the problem,” he said. “[It’s a] bit of instant gratification, honestly.”
What drains him are the calls they cannot fix: mental health crises, child neglect and abuse, homelessness.
“The ER has a [cardiac catheterization] lab that can do surgery in minutes to fix a heart attack. But there’s nowhere I can bring the mental health patients.
“So they call. And they call. And they call.”
Thomas, a primary care paramedic in Eastern Ontario, echoes that frustration.
“The ER isn’t a good place to treat addiction,” he said. “They need intensive, long-term psychological inpatient treatment and a healthy environment and support system — first responders cannot offer that.”
That powerlessness erodes trust. Paramedics say patients with addictions often become aggressive, or stop seeking help altogether.
“We have a terrible relationship with the people in our community struggling with addiction,” Thomas said. “They know they will sit in an ER bed for a few hours while being in withdrawals and then be discharged with a waitlist or no follow-up.”
Carleton, of the University of Regina, says that reviving people repeatedly without improvement decreases morale.
“You’re resuscitating someone time and time again,” said Carleton, who is also director of the Psychological Trauma and Stress Systems Lab, a federal unit dedicated to mental health research for public safety personnel. “That can lead to compassion fatigue … and moral injury.”
Katy Kamkar, a clinical psychologist focused on first responder mental health, says moral injury arises when workers are trapped in ethically impossible situations — saving a life while knowing that person will be back in the same state tomorrow.
“Burnout is … emotional exhaustion, depersonalization, and reduced personal accomplishment,” she said in an emailed statement. “High call volumes, lack of support or follow-up care for patients, and/or bureaucratic constraints … can increase the risk of reduced empathy, absenteeism and increased turnover.”
Kamkar says moral injury affects all branches of public safety, not just paramedics. Firefighters, who are often the first to arrive on the scene, face trauma from overdose deaths. Police report distress enforcing laws that criminalize suffering.
Understaffed and overburdened
Staffing shortages are another major stressor.
“First responders were amazing during the pandemic, but it also caused a lot of fatigue, and a lot of people left our business because of stress and violence,” said Marc-André Périard, vice president of the Paramedic Chiefs of Canada.
Nearly half of emergency medical services workers experience daily “Code Blacks,” where there are no ambulances available. Vacancy rates are climbing across emergency services. The federal government predicts paramedic shortages will persist over the coming decade, alongside moderate shortages of police and firefighters.
Unsafe work conditions are another concern. Responders enter chaotic scenes where bystanders — often fellow drug users — mistake them for police. Paramedics can face hostility from patients they just saved, says Périard.
“People are upset that they’ve been taken out of their high [when Naloxone is administered] and not realizing how close to dying they were,” he said.
Thomas says safety is undermined by vague, inconsistently enforced policies. And efforts to collect meaningful data can be hampered by a work culture that punishes reporting workplace dangers.
“If you report violence, it can come back to haunt you in performance reviews” he said.
Some hesitate to wait for police before entering volatile scenes, fearing delayed response times.
“[What] would help mitigate violence is to have management support their staff directly in … waiting for police before arriving at the scene, support paramedics in leaving an unsafe scene … and for police and the Crown to pursue cases of violence against health-care workers,” Thomas said.
“Right now, the onus is on us … [but once you enter], leaving a scene is considered patient abandonment,” he said.
Upstream solutions
Carleton says paramedics’ ability to refer patients to addiction and mental health referral networks varies widely based on their location. These networks rely on inconsistent local staffing, creating a patchwork system where people easily fall through the cracks.
“[Any] referral system butts up really quickly against the challenges our health-care system is facing,” he said. “Those infrastructures simply don’t exist at the size and scale that we need.”
Périard agrees. “There’s a lot of investment in safe injection sites, but not as much [resources] put into help[ing] these people deal with their addictions,” he said.
Until that changes, the cycle will continue.
On May 8, Alberta renewed a $1.5 million grant to support first responders’ mental health. Carleton welcomes the funding, but says it risks being futile without also addressing understaffing, excessive workloads and unsafe conditions.
“I applaud Alberta’s investment. But there need to be guardrails and protections in place, because some programs should be quickly dismissed as ineffective — but they aren’t always,” he said.
Carleton’s research found that fewer than 10 mental health programs marketed to Canadian governments — out of 300 in total — are backed up by evidence showing their effectiveness.
In his view, the answer is not complicated — but enormous.
“We’ve got to get way further upstream,” he said.
“We’re rapidly approaching more and more crisis-level challenges… with fewer and fewer [first responders], and we’re asking them to do more and more.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Business
Prime minister can make good on campaign promise by reforming Canada Health Act

From the Fraser Institute
While running for the job of leading the country, Prime Minister Carney promised to defend the Canada Health Act (CHA) and build a health-care system Canadians can be proud of. Unfortunately, to have any hope of accomplishing the latter promise, he must break the former and reform the CHA.
As long as Ottawa upholds and maintains the CHA in its current form, Canadians will not have a timely, accessible and high-quality universal health-care system they can be proud of.
Consider for a moment the remarkably poor state of health care in Canada today. According to international comparisons of universal health-care systems, Canadians endure some of the lowest access to physicians, medical technologies and hospital beds in the developed world, and wait in queues for health care that routinely rank among the longest in the developed world. This is all happening despite Canadians paying for one of the developed world’s most expensive universal-access health-care systems.
None of this is new. Canada’s poor ranking in the availability of services—despite high spending—reaches back at least two decades. And wait times for health care have nearly tripled since the early 1990s. Back then, in 1993, Canadians could expect to wait 9.3 weeks for medical treatment after GP referral compared to 30 weeks in 2024.
But fortunately, we can find the solutions to our health-care woes in other countries such as Germany, Switzerland, the Netherlands and Australia, which all provide more timely access to quality universal care. Every one of these countries requires patient cost-sharing for physician and hospital services, and allows private competition in the delivery of universally accessible services with money following patients to hospitals and surgical clinics. And all these countries allow private purchases of health care, as this reduces the burden on the publicly-funded system and creates a valuable pressure valve for it.
And this brings us back to the CHA, which contains the federal government’s requirements for provincial policymaking. To receive their full federal cash transfers for health care from Ottawa (totalling nearly $55 billion in 2025/26) provinces must abide by CHA rules and regulations.
And therein lies the rub—the CHA expressly disallows requiring patients to share the cost of treatment while the CHA’s often vaguely defined terms and conditions have been used by federal governments to discourage a larger role for the private sector in the delivery of health-care services.
Clearly, it’s time for Ottawa’s approach to reflect a more contemporary understanding of how to structure a truly world-class universal health-care system.
Prime Minister Carney can begin by learning from the federal government’s own welfare reforms in the 1990s, which reduced federal transfers and allowed provinces more flexibility with policymaking. The resulting period of provincial policy innovation reduced welfare dependency and government spending on social assistance (i.e. savings for taxpayers). When Ottawa stepped back and allowed the provinces to vary policy to their unique circumstances, Canadians got improved outcomes for fewer dollars.
We need that same approach for health care today, and it begins with the federal government reforming the CHA to expressly allow provinces the ability to explore alternate policy approaches, while maintaining the foundational principles of universality.
Next, the Carney government should either hold cash transfers for health care constant (in nominal terms), reduce them or eliminate them entirely with a concordant reduction in federal taxes. By reducing (or eliminating) the pool of cash tied to the strings of the CHA, provinces would have greater freedom to pursue reform policies they consider to be in the best interests of their residents without federal intervention.
After more than four decades of effectively mandating failing health policy, it’s high time to remove ambiguity and minimize uncertainty—and the potential for politically motivated interpretations—in the CHA. If Prime Minister Carney wants Canadians to finally have a world-class health-care system then can be proud of, he should allow the provinces to choose their own set of universal health-care policies. The first step is to fix, rather than defend, the 40-year-old legislation holding the provinces back.
-

 Crime2 days ago
Crime2 days agoEyebrows Raise as Karoline Leavitt Answers Tough Questions About Epstein
-

 Alberta2 days ago
Alberta2 days agoCOWBOY UP! Pierre Poilievre Promises to Fight for Oil and Gas, a Stronger Military and the Interests of Western Canada
-
 Alberta2 days ago
Alberta2 days agoAlberta and Ontario sign agreements to drive oil and gas pipelines, energy corridors, and repeal investment blocking federal policies
-
 Crime1 day ago
Crime1 day ago“This is a total fucking disaster”
-

 International2 days ago
International2 days agoChicago suburb purchases childhood home of Pope Leo XIV
-

 Fraser Institute1 day ago
Fraser Institute1 day agoBefore Trudeau average annual immigration was 617,800. Under Trudeau number skyrocketted to 1.4 million annually
-

 Daily Caller2 days ago
Daily Caller2 days agoBlackouts Coming If America Continues With Biden-Era Green Frenzy, Trump Admin Warns
-

 MAiD1 day ago
MAiD1 day agoCanada’s euthanasia regime is already killing the disabled. It’s about to get worse