Addictions
Ottawa “safer supply” clinic criticized by distraught mother

An Ottawa mother, who lost her daughter to addiction, is frustrated by Recovery Care’s failure to help her opioid-addicted son
Masha Krupp has already lost one child to an overdose and fears she could lose another.
In 2020, her 47-year-old daughter Larisa died from methadone toxicity just 12 days into an opioid addiction treatment program. The program is run by Recovery Care, an Ottawa-based harm reduction clinic with five locations across the city, which aims to stabilize drug users and eventually wean them off more potent drugs.
Krupp says she is skeptical about the effectiveness of the support and counseling services that Recovery Care claims to provide and believes the clinic was negligent in her daughter’s case.
On Oct. 22, the Ottawa mother testified before the House of Commons Standing Committee on Health, which is studying Canada’s opioid epidemic.
In her testimony, Krupp said her daughter was prescribed 30mg of methadone — 50 per cent more than the recommended induction dose — and was not given an opiate tolerance test before starting the program. Larisa received treatment at the Bells Corners Recovery Care location.
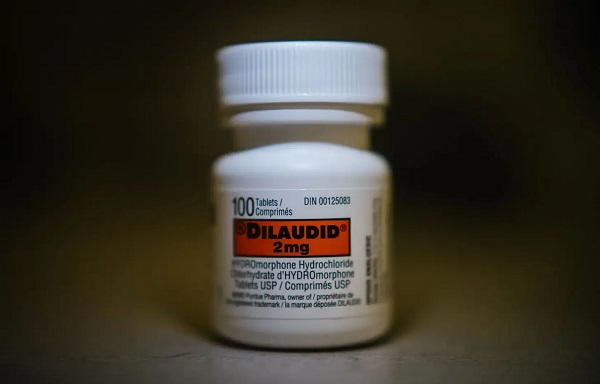
Krupp’s 30-year-old son, whom Canadian Affairs agreed not to name, has been a patient at Recovery Care’s ByWard Market location since 2021, where he receives a combination of methadone and hydromorphone, another prescription drug administered through the treatment program.
“Three years later, my son is still using fentanyl, crack cocaine and methadone, despite being with Dr. [Charles] Breau and with Recovery Care for over three years,” Krupp testified.
“About four weeks ago, I had to call 9-1-1 because he was overdosing,” Krupp told Canadian Affairs in an interview. “This is on the safer supply program … three years in, I should not be calling 9-1-1.”
Open diversion
Founded in 2018, Recovery Care is a partner in the Safer Supply Ottawa initiative. The initiative, which is led by Ottawa Public Health and managed by the nonprofit Pathways to Recovery, provides prescription pharmaceutical opioids to individuals who are at high risk of overdose.
Pathways to Recovery works with a network of service providers throughout the city — including Recovery Care — to administer safer supply.
Krupp says she supports the concept of safer supply, but believes it needs to be administered differently.
“You can’t give addicts 28 pills and say ‘Oh here you go,’” she said in her testimony. “They sell for three dollars a pop on the street,” she said, referring to the practice of some individuals selling their prescribed medications to fund purchases of more intense street drugs like heroin and fentanyl.
Krupp says she sees her son — and other patients of the program — openly divert their prescribed medications outside of the Recovery Care clinic in ByWard Market, where she parks to wait for him.
“[B]ecause there’s no treatment attached to [my son’s safer supply], it’s just the doctor gives him all these pills, he diverts them, gets the drugs he needs, and he’s still an addict,” Krupp said in her testimony.
Donna Sarrazin, chief executive of Recovery Care, told Canadian Affairs that Recovery Care has measures to address diversion, including security cameras and onsite security staff.
“Patients are educated at intake and ongoing that diversion is not permitted and that they could be removed from the program,” she said in an emailed statement.
“Recovery Care works to understand diversion and has continued to progress programs and actions to address the issues. Concerns expressed by the community and our teams are taken seriously,” she said.
Krupp says she has communicated her concerns about her son reselling his prescribed medications to his doctor, Dr. Charles Breau, both in-person and through faxed letters. “I never hear back from the doctor. Never,” she said.
Krupp also said in her testimony that police have spoken to her son about his diversion.
Breau did not respond to inquiries made to his clinical teams at Recovery Care or Montfort Hospital, a teaching hospital affiliated with the University of Ottawa.
Sarrazin said Breau is not able to comment on patient or family care.
In Krupp’s view, the safer supply program would be more successful if drug users were required to take prescribed medications under supervision.
“If he was receiving his hydromorphone under witnessed dosage and there was a treatment plan attached to it, I believe it would be successful,” she said.
Dr. Eileen de Villa, the City of Toronto’s medical officer of health, reinforced this point at the Oct. 22 Health Committee meeting. She said Toronto Public Health’s injectable opioid agonist therapy program — which combines observed administration with a treatment plan — has seen “incredible results.”
De Villa shared a case of a pregnant client who entered the program. “She went on to have a successful pregnancy, a healthy baby, has actually successfully completed the treatment, and is now housed and has even gained custody of her other children,” she said.
Subscribe for free to get BTN’s latest news and analysis, or donate to our journalism fund.
‘An affront to me’
Krupp also says Recovery Care fails to deliver on its promise of supporting patients’ mental health needs. Recovery Care’s website says its clinics offer “mental health programs which are essential to every treatment plan.”
Krupp and her son’s father have both requested a clear treatment plan and consistent counselling for their son. But he was started on safer supply after participating in only one virtual counselling session, she says.
She says Recovery Care has only one mental health counselor who services four of Recovery Care’s clinics. “If you’re getting $2-million-plus a year in funding, you should be able to staff each clinic with one on-site counselor five days a week,” she said.
Instead of personalized assistance, her son received “a sheaf of photocopies” offering generic services like Narcotics Anonymous and crisis helplines. “It’s almost an affront to me, as a taxpayer and a mother of an addict,” Krupp said.
Krupp says that, following her testimony to the parliamentary committee, Breau reached out to offer her son a mental health counseling session for the first time.
Sarrazin told Canadian Affairs that patients are encouraged to request counseling at any time. “Currently there is no wait list and appointments can be booked within 1 week,” she said in her emailed statement.
Class actions
Today, Krupp is considering launching a class-action lawsuit against Health Canada and the Government of Canada, challenging both the enactment of safer supply and the loosening of methadone dispensing requirements in 2017. She believes these changes contributed to her daughter’s death in 2020.
She is also considering joining an existing class-action lawsuit in B.C., which alleges Health Canada failed to monitor the distribution of drugs provided through safer supply programs.
The Pathways to Recovery initiative received $9.69-million in funding from Health Canada from July 2020 to March 2025. In June 2023, Health Canada allocated an additional $1.9 million to expand Ottawa’s safer supply program across five sites and improve access to practitioners, mental health support, housing and other services.
“I want to see that money being put to a recovery based treatment, not simply people going in and out and getting their medications and just creating this new sub-layer of addicts,” Krupp said.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe for free to get BTN’s latest news and analysis, or donate to our journalism fund.
Addictions
From opioids to office: An interview with Alberta’s new addiction minister

By Alexandra Keeler
Rick Wilson shares what led him into — and out of — addiction, his goals for Alberta’s recovery model and the value of an ‘Indigenous lens’
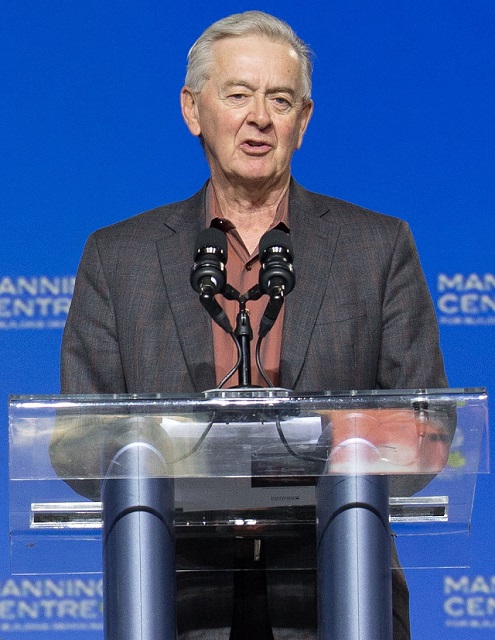
In mid-May, Alberta appointed Rick Wilson as the province’s new minister of mental health and addiction.
Wilson, who represents the Maskwacîs-Wetaskiwin riding south of Edmonton, was Alberta’s longest serving minister of Indigenous relations, serving from 2019 to this year.
Now, Wilson is tasked with accelerating the implementation of the Alberta Model, a recovery-oriented system of care that prioritizes addiction prevention, early intervention and treatment over harm reduction.
Canadian Affairs spoke with Wilson about his priorities in the new role, how his prior work with Indigenous communities shapes his perspective and what lies ahead for mental health and addiction care in Alberta.
AK: I understand you’ve been tasked with advancing the Alberta Recovery Model. What aspects of the model require the most focus in the term ahead?
RW: My goal is going to be to keep the momentum going. [We need to] get all the recovery communities opened up, keep expanding our supports, like CASA Classrooms [classroom-based mental health programs], and just keep filling the gaps for better information.
AK: Why was your predecessor, Dan Williams, shuffled out of the post?
It was a cascading event. Our speaker took a job in Washington, so we voted for a new speaker, Rick McIver. That left a hole in Municipal Affairs, [where Dan was moved]. I’d been bugging Premier Smith for more help with addictions and mental health. She said, ‘Go fix it then, I’ll put you there.’
AK: Do you have personal experience with mental health or addiction struggles?
RW: Do you want the whole sad story here?
I used to raise a lot of cattle and had one really rank bull that was terrorizing the farm. One morning I tried to get him up, and it didn’t end well — he got me down, fractured several vertebrae in my neck and back, and collapsed my lungs. I don’t know how I survived, but somehow I did.
For a year, I couldn’t walk. I was in so much pain I didn’t even know who I was. I would literally pray for one second of relief. Whatever the doctor gives you, you’ll take it — Oxytocin to Percocet; you name it, I was on it. My wife said she’d give me a pill and an hour later, I’d be begging her for more. This went on for close to a year.
I finally had what’s called laser spinal surgery. I was one of the very lucky ones. I went into it in a wheelchair, but I came out walking, and the pain was gone.
About a week later, I told my wife, ‘I think I’m full of infection — I’m burning up with fever, I’m sweating, and I think they’ve nicked a nerve. I feel like I got a giant hole in me.’ She looked at me like I was crazy.
We went to the doctor. He said I was completely healed and asked, ‘What do they have you on?’ Then he said, ‘You just quit taking everything?’ I told him, ‘Yeah, there’s no more pain, so I just quit.’
He said, ‘Well, you’re in withdrawal.’
Once I knew what it was, I was able to tough it out, but it’s not a pleasant experience. I don’t think people are really trying to get high — you just don’t want to feel that alone. I literally felt like there was a hole right through me, like I was just empty inside. So I have a lot of empathy for people that are in addiction.

Rick Wilson was sworn in as the Minister of Mental Health and Addictions on May 16. | Rick Wilson via Facebook
RW: When I was in Indigenous Relations, half my time was spent around addiction issues. It’s horrible. Out on the First Nations, there’s hardly a chief who hasn’t lost a son or somebody close to them. That’s all I did — go to funerals, one after another.
What I learned was you really just have to listen — and that’s one thing the government isn’t good at.
AK: What learnings from that role are you bringing to your new portfolio, and how do you see them benefiting your work in mental health and addiction?
RW: I want to put an Indigenous lens on the whole thing. I think that’s the piece we’re missing. What I found most successful was to use their culture. Get the elders involved. They have the sweats, smudges and language. To take somebody’s language away is devastating.
You hear a lot about reconciliation, but I took it for real. My good friend Willie Littlechild said, ‘Minister, I want to see some reconcili-action.’ He said I could use that — so I do, a lot.
AK: Can Indigenous recovery models work more broadly for non-Indigenous Albertans?
RW: I’ve really seen it work with non-Indigenous folks as well. But everybody’s going to be different. For some people, maybe Christianity is the way to go. And for some people, it’s Alcoholics Anonymous.
I think [the common thread] is that hope. [When you’re addicted] you feel hopeless.
I felt empty, and you need something to replace that emptiness. The problem is, you turn to alcohol, you turn to drugs to fill that gap, and that’s not going to do it. It’s a very temporary fix that just pushes you deeper down the rabbit hole.

Minister Rick Wilson celebrates the Pigeon Lake Regional School Class of 2025 on May 25. | Rick Wilson via Facebook
AK: Can you explain what a recovery community is, and how it fits into the province’s continuum of care?
RW: The way they used to do it, you’d throw someone in recovery for a couple of weeks [and expect] that should cure it, then out you go. Well, that doesn’t work.
[Now] it’s more of a holistic approach: you go into detox, and then from there, you go into rehab. Some people fall out of rehab, [but they go] back into detox, and eventually you start working your way around the circle.
Transitional housing is key. You can’t just send someone back into the community without support — they’ll relapse. After housing, the focus is on community reintegration, finding work, and family support. It’s like an Indigenous healing circle — a full circle to prevent falling back into addiction.
We’re working on 11 sites — one in Red Deer, Gunn, Lethbridge and Calgary opening this summer. Seven more are planned, including Edmonton, Grande Prairie and five with Indigenous communities.
AK: Some critics argue that the Alberta Model leans toward coercive care, and that the benefits of involuntary treatment may not outweigh the risks and costs. How will the Compassionate Intervention Act, which mandates addiction treatment, address those concerns?
RW: Compassionate care isn’t just for the individuals [with substance use disorders]. We have to be compassionate for them, but we also have to be compassionate for the people in their community that are impacted.
In my own riding in the Maskwacîs-Wetaskiwin — some people come in [to the hospital] three times in a day that have overdosed. To overdose several times a day — you’re doing brain damage when you’re at that point.
These people are in dire straits, and we have to intervene with them, because they’re not even capable of thinking for themselves [or] to go for voluntary treatment. We want to give the people that are addicted that opportunity to rebuild their lives. Right now, there’s just a lot of enabling going on.
This interview has been edited and condensed for clarity.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Addictions
After eight years, Canada still lacks long-term data on safer supply
By Alexandra Keeler
Canada has spent more than $100 million on safer supply programs, but has failed to research their long-term effects
Canada lacks long-term data on safer supply programs, despite funding these programs for years.
Safer supply programs dispense pharmaceutical opioids as a replacement for toxic street drugs.
There is a growing body of research on safer supply’s short-term health effects. But there are no Canadian studies that evaluate program participants’ health impacts beyond 18 months.
The absence of research into long-term data on safer supply means policymakers do not understand how safer supply affects participants’ health, substance use or social outcomes over time.
“Long-term data is important because it helps us understand not just short-term health outcomes like reduced overdoses, but also broader impacts on quality of life, stability and health care use,” said Farihah Ali, scientific lead at the Institute for Mental Health Policy Research at CAMH. The Centre for Addiction and Mental Health is one of Canada’s leading centres for addiction research and clinical care.
Pilot projects
Canada’s first safer supply programs were introduced in Ontario in 2016. Those programs were initially small in scope, intended for a small group of high-risk individuals.
In 2020, the federal government began funding safer supply pilot programs across the country. Provinces are responsible for the delivery and regulation of these programs.
B.C. introduced provincewide programs in 2021. Other provinces, such as Alberta, have restricted safer supply access to a very small number of clinics, and have generally shifted away from harm reduction models in favour of recovery-oriented approaches.
According to the Canadian Public Health Association, an advocacy organization, the original goal for safer supply was to reduce deaths and harms associated with the unregulated toxic drug supply. It was not meant to replace addiction treatment, but to rather act as a bridge to further care.
However, a 2023 report by researchers at McMaster University and Simon Fraser University noted safer supply “does not principally operate toward goals of treatment or recovery.” The report describes safer supply instead as an emergency intervention focused on stabilization and survival.
Evidence gaps
There is a small but growing body of short-term studies on the health effects of Canada’s safer supply programs. Most only track participants’ outcomes for up to 12 months.
Some of those studies suggest safer supply may reduce the immediate harms associated with drug use.
A 2024 study found a 91 per cent reduction in the risk of death among high-risk individuals receiving safer supply in B.C. Critics have raised concerns about the study’s methodology, sample size and confounding variables.
In contrast, a March study suggested B.C.’s safer supply and decriminalization policies may be associated with increased hospitalizations. These findings also sparked controversy, with experts debating how well the data isolate causal impacts.
And a comparative study released in April also showed some positive outcomes from safer supply. It too sparked significant expert debate.
‘Arms-length’
Of all the provinces, B.C. has implemented safer supply most broadly. The province’s health ministry did not directly respond when asked about the long-term goals of its safer supply program, or whether B.C. collects longitudinal data on program participants’ health outcomes.
“Evidence shows [safer supply] helps separate people from the unregulated drug supply, manage their substance use and withdrawal symptoms with regulated medications, and helps connect them to voluntary health and social supports,” a Ministry of Health spokesperson told Canadian Affairs in an email.
The ministry did not provide the evidence it referenced.
At the federal level, Health Canada confirmed that, to date, it has funded just two evaluations of safer supply programs, despite spending more than $100 million on safer supply since April 2023.
The first was a short-term study, funded by the federal government’s Substance Use and Addictions Program program. Conducted over four months, that study assessed 10 safer supply programs in Ontario, B.C., and New Brunswick. It documented initial impacts on participants’ lives and program delivery, primarily through qualitative methods such as interviews and surveys.
The second study is an ongoing, “arms-length evaluation” of 11 safer supply pilot programs funded by the Canadian Institutes of Health Research (CIHR), Canada’s federal health research agency.
When asked about long-term research on safer supply, Health Canada referred Canadian Affairs to a 2022 funding announcement about this multi-year evaluation. While the evaluation is being conducted over several years, it is unclear if it includes long-term tracking of patients’ outcomes.
Barriers and resistance
There are a number of factors that make it challenging to evaluate safer supply programs over long periods.
Ali, of CAMH, says unstable, short-term funding can disrupt long-term research.
“When programs are shut down or scaled back, we lose contact with participants and the ability to track outcomes over time,” she said.
Program participants can also be difficult to track over long periods, she says. Many struggle with housing insecurity, health instability and criminalization.
Frontline staff also face burnout and high turnover, she says, limiting support for such research activities.
Additionally, there are tradeoffs between the anonymity needed to encourage patients to access safer supply programs and the ability to collect detailed data.
“Ethical concerns — like not wanting to burden participants or risk their safety or confidentiality — require us to design studies that are trauma-informed and flexible, which adds complexity to long-term data collection,” Ali said.
Julian Somers, a clinical psychologist and professor at Simon Fraser University, says B.C.’s failure to conduct long-term evaluations of its safer supply programs is not just an oversight, but an act of negligence.
“B.C. has some of the best pharmaceutical data systems in the world,” Somers said, referring to PharmaCare and PharmaNet — databases that capture every prescription drug transaction in the province.
Somers says his team previously used PharmaNet data to examine prescribed opioids’ effects on health and social outcomes. In 2017, he proposed a long-term safer supply evaluation using these tools.
In 2017, he proposed a long-term evaluation of B.C.’s safer supply programs.
The province declined.
According to Ali, “Future research should explore how safer supply impacts people’s long-term health, stability and connection to care.”
“We also need to listen to people’s experiences, how safer supply affects their daily lives, their sense of dignity, and their relationships with care providers through qualitative mechanisms.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
-
 Education1 day ago
Education1 day agoWhy more parents are turning to Christian schools
-

 Alberta1 day ago
Alberta1 day agoOPEC+ is playing a dangerous game with oil
-

 Alberta1 day ago
Alberta1 day agoUpgrades at Port of Churchill spark ambitions for nation-building Arctic exports
-

 Business1 day ago
Business1 day agoIs dirty Chinese money undermining Canada’s Arctic?
-

 COVID-191 day ago
COVID-191 day agoJapan disposes $1.6 billion worth of COVID drugs nobody used
-

 conflict1 day ago
conflict1 day agoOne of the world’s oldest Christian Communities is dying in Syria. Will the West stay silent?
-

 COVID-191 day ago
COVID-191 day agoWATCH: Big Pharma scientist admits COVID shot not ‘safe and effective’ to O’Keefe journalist
-

 Bruce Dowbiggin1 day ago
Bruce Dowbiggin1 day agoHow Did PEI Become A Forward Branch Plant For Xi’s China?