Fraser Institute
Other countries with universal health care don’t have Canada’s long wait times

From the Fraser Institute
By Mackenzie Moir and Bacchus Barua
Unfortunately it’s now very common to see stories about how long provincial wait times for medical care are driving patients to seek care elsewhere, often at great personal cost. Take the recent case of the Milburns in Manitoba who, after waiting years for a knee surgery, are now considering selling their home and moving to Alberta just to get on a potentially shorter public wait list.
Patients in Manitoba could expect to wait a median of 29 weeks to see an orthopedic specialist after a referral from a family physician, then they still faced a median 24.4 week wait to get treatment. In other words, the total typical wait for orthopedic surgery in the province is more than one year at 53.4 weeks. Remember, that’s a median measure, which means some patients wait much longer.
Unfortunately, the Milburns are unlikely to get more timely care on the public wait list in Alberta. At 64.1 weeks, the total median wait for orthopedic care in Alberta was actually longer than in Manitoba. And this doesn’t include the time it takes for provincial coverage to activate for a new provincial resident, or the time it will take to find a new family doctor and get the necessary tests, scans and referrals.
To get more timely care, the Milburns are left with unenviable options. Because they’re insured by Manitoba’s public health-care plan, paying for covered care out of pocket is restricted. They can, however, pay for and receive care privately in other provinces as uninsured visitors (i.e. not move there permanently). Specifically, certain provinces have “exemptions” that allow physicians to charge out-of-province patients directly to provide these procedures privately.
Alternatively, the Milburns could leave Canada and travel even further from home to receive timely care abroad.
But it doesn’t have to be this way.
Long wait times are not the necessary price Canadians must pay for universal coverage. In fact, Canada is one of 30 high-income countries with universal health care. Other countries such as Switzerland, the Netherlands, Germany and Australia have much shorter wait times. For example, only 62 per cent of Canadians reported access to non-emergency surgery in less than four months in 2020 compared to 99 per cent of Germans, 94 per cent of Swiss and 72 per cent of Australians.
The difference? These countries approach health care in a fundamentally different way than us. One notable difference is their attitude towards the private sector.
In Germany, patients can seek private care while still insured by the public system or can opt out and purchase regulated private coverage. These approaches (universal, privately paid or privately insured) are able to deliver rapid access to care. The Swiss simply mandate that patients purchase private insurance in a regulated-but-competitive marketplace as part of their universal scheme. Lower-income families receive a subsidy so they can participate on a more equal footing in the competitive marketplace to obtain the insurance that best fits their needs.
Perhaps the most direct comparator to Canada is Australia—not just geographically, but because it also primarily relies on a tax-funded universal health-care system. However, unlike Canada, individuals can purchase private insurance to cover (among other things) care received as a private patient in a public or private hospital, or simply pay for their private care directly if they choose. In 2021/22 more than two-thirds (70 per cent) of non-emergency admissions to a hospital involving surgery (both publicly and privately funded) took place in a private facility.
Of course, these faster-access countries share other differences in attitudes to universal health-care policy including requirements to share the cost of care for patients and funding hospitals on the basis of activity (instead of Canada’s outdated bureaucratically-determined budgets). A crucial difference, however, is that patients are not generally prevented from paying privately for health care in their home province (or canton or state) in any of these countries.
Without fundamental reform, and as provincial systems continue to struggle to provide basic non-emergency care, we’ll continue to see more stories like the Milburn’s. Without reform, many Canadians will continue to be forced to make similarly absurd decisions to get the care they need, rather than focusing on treatment and recovery.
Authors:
Business
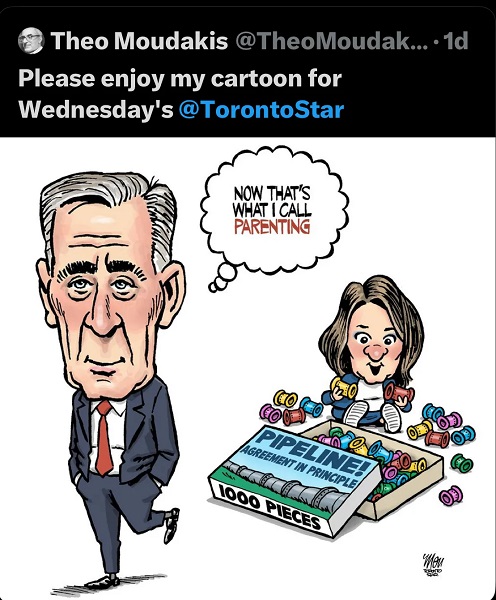
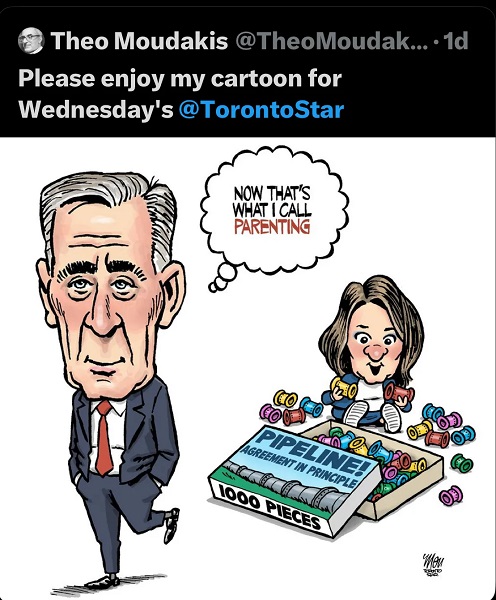
Ottawa’s gun ‘buyback’ program will cost billions—and for no good reason

From the Fraser Institute
By Gary Mauser
The government told Cape Bretoners they had two weeks to surrender their firearms to qualify for reimbursement or “buyback.” The pilot project netted a grand total of 22 firearms.
Five years after then-prime minister Justin Trudeau banned more than 100,000 types of so-called “assault-style firearms,” the federal government recently made the first attempt to force Canadians to surrender these firearms.
It didn’t go well.
The police chief in Cape Breton, Nova Scotia, volunteered to run a pilot “buyback” project, which began last month. The government told Cape Bretoners they had two weeks to surrender their firearms to qualify for reimbursement or “buyback.” The pilot project netted a grand total of 22 firearms.
This failure should surprise no one. Back in 2018, a survey of “stakeholders” warned the government that firearms owners wouldn’t support such a gun ban. According to Prime Minister Carney’s own Privy Council Office the “program faces a risk of non-compliance.” And federal Public Safety Minister Gary Anandasangaree was recently recorded admitting that the “buyback” is a partisan maneuver, and if it were up to him, he’d scrap it. What’s surprising is Ottawa’s persistence, particularly given the change in the government and the opportunity to discard ineffective policies.
So what’s really going on here?
One thing is for certain—this program is not, and never has been, about public safety. According to a report from the federal Department of Justice, almost all guns used in crimes in Canada, including in big cities such as Toronto, are possessed illegally by criminals, with many smuggled in from the United States. And according to Ontario’s solicitor general, more than 90 per cent of guns used in crimes in the province are illegally imported from the U.S. Obviously, the “buyback” program will have no effect on these guns possessed illegally by criminals.
Moreover, Canadian firearms owners are exceptionally law-abiding and less likely to commit murder than other Canadians. That also should not be surprising. To own a firearm in Canada, you must obtain a Possession and Acquisition Licence (PAL) from the RCMP after initial vetting and daily monitoring for possible criminal activity. Between 2000 and 2020, an average of 12 PAL-holders per year were accused of homicide, out of approximately two million PAL-holders. During that same 10-year period, the PAL-holder firearms homicide rate was 0.63 (per 100,000 PAL-holders) compared to 0.72 (per 100,000 adult Canadians)—that’s 14 per cent higher than the rate for PAL-holders.
In other words, neither the so-called “assault-style firearms” nor their owners pose a threat to the public.
And the government’s own actions belie its claims. If these firearms are such a threat to Canadians, why slow-roll the “buyback” program? If inaction increased the likelihood of criminality by law-abiding firearms owners, why wait five years before launching a pilot program in a small community such as Cape Breton? And why continue to extend the amnesty period for another year, which the government did last month at the same time its pilot project netted a mere 22 firearms?
To ask those questions is to answer them.
Another question—how much will the “buyback” program cost taxpayers?
The government continues to block any attempt to disclose the full financial costs (although the Canadian Taxpayers Federation has launched a lawsuit to try to force the government to honour its Access to Information Act request). But back in 2020 the Trudeau government said it would cost $200 million to compensate firearms owners (although the Parliamentary Budget Officer said compensation costs could reach $756 million). By 2024, the program had spent $67.2 million—remember, that’s before it collected a single gun. The government recently said the program’s administrative costs (safe storage, destruction of hundreds of thousands of firearms, etc.) would reach an estimated $1.8 billion. And according to Carney’s first budget released in November, his government will spend $364 million on the program this fiscal year—at a time of massive federal deficits and debt.
This is reminiscent of the Chretien government’s gun registry fiasco, which wound up costing more than $2 billion even after then-justice minister Allan Rock promised the registry program would “almost break even” after an $85 million initial cost. The Harper government finally scrapped the registry in 2012.
As the Carney government clings to the policies of its predecessor, Canadians should understand the true nature of Ottawa’s gun “buyback” program and its costs.
Business
Recent price declines don’t solve Toronto’s housing affordability crisis

From the Fraser Institute
By Jake Fuss and Austin Thompson
House prices in Toronto are declining. But the city’s affordability crisis is far from over—and government policies will likely make it worse.
While most Torontonians know there’s a crisis, the numbers make it clear. According to our new study, in 2023 (the latest year of available data), a family earning the city’s median after-tax income ($60,510) had to save $216,240 (the equivalent of 42.9 months of its after-tax income) for a 20 per cent downpayment on a typical home of any type (single-detached, semi-detached, condominium). But even if that family could somehow clear this monumental hurdle, it then had to dedicate 110.2 per cent of its after-tax income for monthly mortgage payments ($5,557)—a financial impossibility, unless the family can share housing costs (e.g. live-in tenants) or rely on financial support from elsewhere.
At this point, some long-time Toronto residents might recall their own difficult home purchase and think, “Hasn’t it always been this bad?” But just a decade ago, the hurdles weren’t nearly as high.
For example, in 2014 in Toronto, a 20 per cent downpayment cost 26.4 months of median after-tax family income—not 42.9 months. And the monthly mortgage payment on a typical home purchase required 56.0 per cent of median after-tax family income—not 110.2 per cent. So yes, typical homes have been broadly unaffordable for median-income-earning Toronto families for years, but it’s way worse now.
For Torontonians priced out of homeownership, renting has not offered much relief. In 2023, Toronto had the least affordable rents in Canada. The monthly cost of the median rental unit was $1,750, equal to 34.7 per cent of the median after-tax family income. That’s up from $1,110 (or 27.7 per cent of after-tax income) in 2014.
Fast-forward to today, and Torontonians should view reports of “crashing” home prices in the proper context. Typical home prices peaked at $1.27 million in the first quarter of 2022. By the second quarter of 2025, they had fallen to $1.00 million. That’s a marked decline, but prices remain well above pre-pandemic levels and far beyond the reach of most typical families.
And while the fall in house prices hasn’t been enough to restore affordability, it has caused a steep contraction in homebuilding as builders take a more cautious approach to development at a time when the city still needs more new homes to improve affordability.
This unhealthy dynamic, where price declines weigh heavily on housing construction, is made worse by government policy. Despite hundreds of millions of taxpayer dollars spent on housing initiatives by the federal government, the Ford government and Toronto City Hall, key provincial and municipal policies continue to impose needless costs and restrictions on new housing.
For example, Toronto homebuilders must endure costly wait times of more than two years for municipal approvals—more than three times longer than in Vancouver and seven times longer than in Edmonton. New high-rise developments in Toronto face municipal charges of $134,900 per unit compared to $38,100 in Ottawa and $6,900 in Edmonton. Meanwhile, the Ford government has backed away from several critical recommendations from its own Housing Task Force, which would make it easier to build more and denser housing, such as allowing fourplexes provincewide without special approval.
Of course, federal immigration policy, particularly over the last five years, has increased demand for new homes in Toronto and across the country. But even so, if not for lengthy approval processes, sky-high fees and restrictive land-use policies, many more new homes would be built in Toronto today despite declining prices. Homes only get built when buyers can cover the cost of construction plus a reasonable return on investment for developers. But when governments drive up costs, increase uncertainty and claim a significant share of the final sale price through fees and charges, projects that might otherwise proceed can become financially unviable. The result is less new housing, fewer options for buyers and a slower path to improved affordability.
To help improve housing affordability, Toronto needs a steady flow of new homebuilding. Torontonians should demand faster approvals, lower fees and more sensible rules on what types of homes can be built.
-
 National2 days ago
National2 days agoMedia bound to pay the price for selling their freedom to (selectively) offend
-

 Business2 days ago
Business2 days agoIs there a cure for Alzheimer’s Disease?
-

 C2C Journal2 days ago
C2C Journal2 days agoLearning the Truth about “Children’s Graves” and Residential Schools is More Important than Ever
-

 Bruce Dowbiggin2 days ago
Bruce Dowbiggin2 days agoSometimes An Ingrate Nation Pt. 2: The Great One Makes His Choice
-

 Alberta2 days ago
Alberta2 days agoNew era of police accountability
-

 Brownstone Institute2 days ago
Brownstone Institute2 days agoThe Unmasking of Vaccine Science
-

 Alberta2 days ago
Alberta2 days agoEmissions Reduction Alberta offering financial boost for the next transformative drilling idea
-

 Business20 hours ago
Business20 hours agoRecent price declines don’t solve Toronto’s housing affordability crisis