MacDonald Laurier Institute
Barriers to care persist but access to MAiD keeps expanding

From the Macdonald Laurier Institute
By Ramona Coelho
Our government has allowed the incredible power of certain lobby groups to control the public discourse and policies around MAiD and its expansion, prioritizing access to MAiD over the safety of Canadians.
My family medicine practice serves predominantly low-income and marginalized patients, including refugees, those who have been in our prison system or are facing charges, and many with disabilities and mental health issues. My patients experience high barriers to care and support and face social isolation and all kinds of discrimination. Observing the impacts of this has left me deeply concerned about our government’s priorities.
When the federal government introduced MAiD (a medical procedure that causes death) to those not at imminent risk of dying, I was appalled to learn that my patients, who are frequently blocked from care as a result of hurdles created by our government and systems, could potentially be offered an expedient death provided by the government.
In 2016, assisted suicide and euthanasia were first legalized in Canada and the term medical assistance in dying (MAiD) was created. Originally MAiD was presented as an exceptional lethal procedure for ending the lives of consenting adults who were experiencing intolerable suffering and were near death. The legislation required that patients meet certain criteria, including having a “grievous and irremediable” medical condition, such as organ failure or cancer, and a “reasonably foreseeable natural death.”
But the Canadian discourse around MAiD rapidly shifted to facilitating access and there has been a broadening of the number and criteria of those who qualify for MAiD. In 2021, Bill C-7 came into effect and removed some of the safeguards within the original pathway, now called Track 1, and created a new, second track, Track 2, for adults with physical disabilities[1] who are not dying. Furthermore, there is a planned expansion, though the timing is currently being debated in Parliament, for patients whose only medical condition is mental illness. Parliamentary recommendations in 2023 included future expansion to children and to incapable adults who signed advance directives for euthanasia.
Currently, those in Track 1 with a “reasonably foreseeable natural death” can potentially have their life ended the same day as the initial request if all the criteria are met and practitioners are available.
For those in Track 2, those not dying, death by lethal injection is set at a minimum of 90 days after the completion of the first MAiD assessment. To qualify for this track, a patient must also have a “grievous and irremediable” condition and experience intolerable psychological or physical suffering. Suffering is treated as purely subjective with no requirement for further validation. There is also no legal requirement for standard treatment options to be accessible or tried, only that a patient be informed that they exist. This means that a patient who says they are suffering intolerably could access MAiD having declined treatments that would remediate their condition. This could be because the treatment is inaccessible, or unaffordable, or if the patient declines therapy.
The Canadian Association of MAiD Assessors and Providers (CAMAP) has received 3.3 million dollars in funding from Health Canada to educate clinicians assessing and providing for those who have requested the service. So although the existing Track 1 and Track 2 pathways have different safeguards, in aiming to allow those near death to have access to MAiD quickly and with no barriers, CAMAP has created a guidance document that suggests clinicians can be flexible as to whether someone fits Track 1’s reasonably foreseeable natural death, since the law does not require that the person be terminally ill or likely to die within 6 or 12 months. It also states that a person may meet the reasonably foreseeable criterion if they’ve demonstrated a clear and serious intent to take steps to “make their natural death happen soon, or to cause their death to be predictable.” This could come about from a refusal to take antibiotics for an infection, stopping oxygen therapy, or refusing to eat and drink.
This means that people with disabilities can state their intention to or make themselves sick enough to qualify as having a reasonably foreseeable natural death, as is currently happening with adults who are not dying and yet are having their lives ended within days of their first MAiD assessment. In one case, a man had a mild stroke and received MAiD shortly after, even though he wasn’t terminally ill. The reason? He was approved for track 1 as he was temporarily eating less. This was due to following a cautious meal plan ordered by the treating team which was intended to prevent choking and aspiration risks.
Currently, some places in Canada have MAiD rates that are the highest in the world. By the end of 2022, there had been almost 45,000 MAiD deaths across Canada since legalization—more than 13,000 of which took place in 2022 with 463 of those individuals accessing MAiD through Track 2. Estimates based on provincial reporting approximate 16,000 deaths in 2023. Health Canada and MAiD expansionists have tried to reassure the public that the overwhelming number of MAiD deaths have been mostly Track 1 deaths (implying they were dying anyway) but we do not know how many of those persons were “fast-tracked” and may have had many decades of life left to live and the potential to recover with time and care.
The CAMAP guidance document that seems to circumvent Track 2 safeguards is just the beginning of many serious problems with MAiD legislation and practice in Canada.
Patient safeguards for MAiD are lacking
Other jurisdictions in the world where MAiD practices are legalized, such as New Zealand and Victoria, Australia, frown on or prohibit raising death as a treatment option. This is due to the power imbalance that exists between physician and patient, coupled with the patients’ assumption that the provider will only suggest the best options for their health. Raising MAiD unsolicited could cause undue pressure to choose death. Yet Health Canada’s 2023 Model Practice Standard for Medical Assistance in Dying recommends that MAiD should be raised to all who might qualify if the practitioner suspects it aligns with a patient’s values and preferences.
The model practice standard’s approach to “conscientious objection” is equally troubling. Health care providers who object to providing MAiD, even in specific cases, are considered conscientious objectors. A physician who is concerned that MAiD is not a patient’s best option is supposed to ignore their conscience or professional opinion and simply refer the patient on so they can seek access to a MAiD death.
This is further echoed in a CAMAP video training session where experts explain that patients might be driven to MAiD by unmet psycho-social needs. The expert leading the session responds to a trainee’s concerns: “If withdrawing is about protecting your conscience, you have [an] absolute right to do so.” But he adds: “You’ll then have to refer the person on to somebody else, who may hopefully fulfill the request in the end.” This demonstrates precisely how effective referrals can funnel patients toward death despite legitimate professional concerns and obligations that should have instead led to the process being stopped or paused.
In response to this legislation, many from the disability community have advocated for safe spaces where MAiD can’t pose a risk to their lives. The Disability Filibuster, a national grassroots disability community, stated in an open letter that its members have raised fears about seeking health care where death could be offered to them and if at their lowest, they might agree.
The disability community is not being alarmist in this concern. Health care providers often rate the quality of life of those with disabilities as poor despite those patients rating their own quality of life as the same as aged-matched healthy individuals. Put differently, many physicians might consider that patients with disabilities are better off dead, consciously or unconsciously, which might lead them to suggest MAiD.
Besides the problems of mandatory referral and raising MAiD unsolicited, there is another important factor to consider. Persons with physical disabilities systemically lack much of the essential care they need to live and consequently suffer higher rates of isolation, poverty, and marginalization, all of which can make death their most accessible option. The Canadian government commissioned a University of Guelph study, published in 2021, in which the researchers noted that some persons with disabilities were encouraged to explore the MAiD option—even though they had not been contemplating doing so—because of a lack of resources that would enable them to live. Those with disabilities can be approved for MAiD based on their disability, but it is their psycho-social suffering that can drive their requests.
The United Nations Special Rapporteur on the rights of persons with disabilities, the Independent Expert on the enjoyment of all human rights by older persons, and the Special Rapporteur on extreme poverty and human rights have all warned the Canadian government that the current MAiD framework could lead to human rights violations. Their concerns are validated by the numerous fact-checked stories about MAiD abuses that are emerging in Canada. These should give us pause. For example, Sathya Dhara Kovac, 44, ended her life through the MAiD program. She lived with a degenerative disease and her condition was worsening, but she wanted to live but lacked the home care resources to do so. “Ultimately it was not a genetic disease that took me out, it was a system,” Kovac wrote in an obituary to loved ones. All Canadians have a right to humane living conditions, to be treated with respect and dignity, and to receive appropriate timely medical care. Considering the living conditions and lack of care that as a society we allow persons with disabilities to have, choices to die might be understandable for those like Sathya. But we should ask ourselves if choices, made under inhumane conditions, are made freely if driven by structural coercion.
Disturbingly, there are MAiD assessors and providers who seem to be ok with proving MAiD under such inhumane conditions. One such provider testified at a parliamentary committee on MAiD that if someone had to wait a long time for a service that would remediate their suffering, she would still consider that waiting to be irremediable suffering and grant them MAiD in the interim. Therefore, it is not surprising that patients with unaddressed psycho-social suffering are being given MAiD by assessors like her.
When it was considering Bill C-7, the federal government asked the Parliamentary Budget Officer to estimate cost savings to our health care system of the legalization of MAiD. The office did this by looking at the comparative cost savings of MAiD versus palliative care at the end of life. Through this impoverished lens of valuation, it is clear that the cost savings will be even greater when, by many years, we prematurely end the lives of people who have higher care needs, especially when we factor in social services, disability benefits, equipment, and other costs on top of the direct savings to health care budgets. But this is not how we should create budgets or measure outcomes. Our socialized health care system is meant to serve those with disabilities, not consider them a cost to the system.
The Canadian government is currently deciding on the timing for its further roll-out of MAiD, this time for mental illness and with no legislative changes to the current safeguards. This expansion is alarming given what we know is happening already to disabled Canadians under the existing MAiD regime. The Canadian Association of Chairs of Psychiatry wrote a letter in 2022—and some testified more recently in Parliament—that we are not ready for this development. They have warned that there is no evidence to guide decisions about who with mental illness would not get better. The evidence suggests that for every 5 people whose lives would be ended based on the sole medical condition of mental illness, 2 or 3 would have recovered. We expect to have much higher numbers qualifying for MAiD on the grounds of mental illness in Canada than in other jurisdictions that allow assisted death for this reason, since barriers to care and unmitigated psycho-social suffering do not have to be rectified in this country (as they do elsewhere) before being granted MAiD.
Our government has allowed the incredible power and influence of certain lobby groups and their members to control the public discourse and policies around MAiD and its expansion, prioritizing access to MAiD over the safety of Canadians. Besides the current discussion about when to legalize MAiD for mental illness, the parliamentary committee has also recommended expansion to children and MAiD by advance directives. With eligibility for MAiD continuing to broaden, we are not giving priority to serving those most in need, but instead seem intent on rapidly expanding a path to end their lives.
[1] Disabilities is an umbrella term that includes impairment, chronic illness and/or other conditions.
Dr. Ramona Coelho is a family physician in London, Ontario. Her practice largely serves marginalized patients.
Alberta
High costs, low returns – Canada’s wildly expensive emissions cap

In this new commentary, Director of Energy, Natural Resources, and Environment Heather Exner-Pirot reveals why the Canadian government’s oil and gas emissions cap isn’t just expensive – it’s economic insanity.
Canada is the world’s third-largest exporter of oil, fourth-largest producer, and top source of imports to the United States. Much of Canada’s oil wealth is concentrated in the oil sands in northern Alberta, which hosts 99 percent of the country’s enormous oil endowment: about 160 billion barrels of proven reserves, of a total resource of approximately 1.8 trillion barrels. This is the major source of oil to the United States refinery complex, a large part of which is optimized for the oil sands’ heavy oil.
Reliability of energy supply has remerged as a major geopolitical issue. Canadian oil and gas is an essential component of North American energy security. Yet a proposed cap on emissions from the sectors promises to cut Canadian production and exports in the years ahead. It would be hard to provide less environmental benefit for a higher economic and security cost. There are far better ways to reduce emissions while maintaining North America’s security of energy supply.
The high cost of the cap
In 1994 a Liberal federal government, Alberta provincial conservative government and representatives from the oil and gas industry, working together through the national oil sands task force, developed A New Energy Vision for Canada. Their efforts turned what was then a middling resource into a trillion dollar nation-building project. Production has increased tenfold since the report came out.
The task force acknowledged the need for industry to “put its best efforts toward … reducing greenhouse gas emissions.” However, it also expected governments to “understand” that there “is no benefit to Canada or to the environment to have production and value-added processing done outside of the country in less efficient jurisdictions … policies set by regulator must not result in discouraging oil sands production.”
As part of its efforts to meet its climate goals under the Paris Accord, the Canadian government proposed a regulatory framework for an emissions cap on the oil and gas sector in December 2023. It set a legally binding limit on greenhouse gas emissions, targeting a 35 to 38 percent reduction from 2019 levels by 2030 for upstream operations, through regulations to be made under the Canadian Environmental Protection Act, 1999 (CEPA).
The federal government has not yet finalized its proposed regulations. However, industry experts and economists have criticized the current iteration as logistically unworkable, overly expensive, and likely to be challenged as unconstitutional. In effect, this policy layers a cap-and-trade system for just one sector (oil and gas) on top of a competing carbon pricing mechanism (the large-emitter trading systems, often referred to as the industrial carbon price), a discriminatory practice that also undermines the entire economic rationale of a carbon pricing system.
While the Canadian government has maintained that it is focused on reducing emissions rather than production – the latter of which would put it at odds with provincial jurisdiction over non-renewable resources – a series of third party analyses as well as the Parliamentary Budget Office’s own impact assessment find it would indeed constrain Canadian oil and gas production. The economic cost of the emissions cap far exceeds any corresponding benefit in reduced emissions.
How much will the emissions cap cost in terms of dollar per tonne of carbon in avoided emissions, both domestically and globally? Based solely on the cost to the Canadian economy, we estimate the emission cap is equivalent to a C$2,887/tonne carbon price by 2032.
Assuming no impact on global demand and full substitution by non-Canadian crudes, it finds that the cost of each tonne of carbon displaced globally is between C$96,000 to C$289,000 for oil sands bitumen production. For displaced Canadian conventional and natural gas, the cost is infinite, i.e. global emissions would actually be higher for every barrel or unit of Canadian oil and gas displaced with competitor products as a result of the emissions cap.
Canadian oil and gas emissions reduction efforts
The oil and gas sector is the highest emitting economic sector in Canada. However, it has made substantial efforts to reduce emissions over the past two decades and is succeeding. Absolute emissions in the sector peaked in 2014, despite production growing by over a million barrels of oil equivalent since (see Figure 1).
 Figure 1 Indexed greenhouse gas (GHG) emissions (and gross domestic product (GDP) at basic prices, for the oil and gas extraction industry, 2009 to 2022 (2009 = 100). Source: Statistics Canada 2024.
Figure 1 Indexed greenhouse gas (GHG) emissions (and gross domestic product (GDP) at basic prices, for the oil and gas extraction industry, 2009 to 2022 (2009 = 100). Source: Statistics Canada 2024.
Much of this success can be attributed to methane capture, particularly in the natural gas and conventional oil sectors, where absolute emissions peaked in 2007 and 2014 respectively.
Since 2014, the oil sands have dramatically increased production by over a million barrels per day, but at the same time have reduced the emissions per barrel every year, leaving the absolute emissions of the oil and gas sector relatively flat. The oil sands are performing well vis-à-vis their international peers, seeing their emissions per barrel decline by 30 percent since 2013, compared to 21 percent for global majors and 34 percent for US E&Ps (exploration and production companies) (see Figure 2).
 Figure 2 Indexed Oil Sands GHG relative intensity trend (2013=100). Source: BMO Capital Markets, “I Want What You Got: Canada’s Oil Resource Advantage,” April 2025
Figure 2 Indexed Oil Sands GHG relative intensity trend (2013=100). Source: BMO Capital Markets, “I Want What You Got: Canada’s Oil Resource Advantage,” April 2025
On an emissions intensity absolute basis, the oil sands have significantly outperformed their peers, shaving off 25kg/barrel of emissions since 2013 (see Figure 3) and more than 65kg/barrel since the oil sands task force wrote their report in 1994.
As emissions improvements from methane reductions plateau, the oil sands are likely to outperform their conventional peers in emissions per barrel reductions going forward. The sector is working on strategies such as solvent extraction and carbon capture and storage that, if implemented, would reduce the life-cycle emissions per barrel of oil sands to levels at or below the global crude average.
 Figure 3 Emissions intensity absolute change (kg CO2e/bbl) (2013–24E) Source: BMO Capital Markets, 2025
Figure 3 Emissions intensity absolute change (kg CO2e/bbl) (2013–24E) Source: BMO Capital Markets, 2025
The high cost of the cap
Several parties have analyzed the proposed emissions cap to determine its economic and production impact. The results of the assessments vary widely. For the purposes of this commentary we rely on the federal Office of the Parliamentary Budget Officer (PBO), which published its analysis of the proposed emissions cap in March 2025. Helpfully, the PBO provided a table summarizing the main findings of the various analyses (see Table 1).
The PBO found that the required reduction in upstream oil and gas sector production levels under an emissions cap would lower real gross domestic product (GDP) in Canada by 0.33 percent in 2030 and 0.39 percent in 2032, and reduce nominal GDP by C$20.5 billion by 2032. The PBO further estimated that achieving the legal upper bound would reduce economy-wide employment in Canada by 40,300 jobs and full-time equivalents by 54,400 in 2032.
 Table 2 Comparison of estimated impacts of the proposed emissions cap in 2030. Source: PBO 2025
Table 2 Comparison of estimated impacts of the proposed emissions cap in 2030. Source: PBO 2025
However, the PBO does not estimate the carbon price per tonne of emissions reduced. This is a useful metric as Canadians have become broadly familiar with the real-world impacts of a price on carbon. The federal government quashed the consumer carbon price at $80/tonne in March 2025, ahead of the federal election, due to its unpopularity and perceived impacts on affordability. The federal carbon pricing benchmark is scheduled to hit C$170 in 2030. ECCC has quantified the damages of a tonne of carbon dioxide – referred to as the “Social Cost of Carbon” – as C$294/tonne.
Based on PBO assumptions that the emissions cap will reduce emissions by 7.1MT and reduce GDP by $20.5 billion in 2032, the implied carbon price is C$2,887/tonne.
Emissions cap impact in a global context
Even this eye-popping figure does not tell the full story. The Canadian oil and gas production that must be withdrawn to meet the requirements of the emissions cap will be replaced in global markets from other producers; there is no reason to assume the emissions cap will affect global demand.
Based on life-cycle GHG emissions of the sample of crudes used in the US refinery complex, Canadian oil sands produce only 1 to 3 percent higher emissions than a global average[1] (see Figure 4), with some facilities producing lower emissions than the average barrel.
 Figure 4 Life Cycle GHG emissions of crude oils (kg CO2e/bbl). Source: BMO Capital Markets 2025
Figure 4 Life Cycle GHG emissions of crude oils (kg CO2e/bbl). Source: BMO Capital Markets 2025
As such, the emissions cap, if applied just to oil sands production, would only displace global emissions of 71,000 to 213,000 tonnes (1 to 3 percent of 7.1MT). At a cost of C$20.5 billion for those global emissions reductions, the price of carbon is equivalent to C$96,000 to C$289,000 per tonne (see Figure 5).
 Figure 5 Cost per tonne of emissions cap behind domestic carbon all (left) and post-global crude substitution (right)
Figure 5 Cost per tonne of emissions cap behind domestic carbon all (left) and post-global crude substitution (right)
For any displaced conventional Canadian crude oil or natural gas, the situation becomes absurd. Because Canadian conventional oil and natural gas have a lower emissions intensity than global averages, global product substitutions resulting from the emissions cap would actually serve to increase global emissions, resulting in an infinite price per tonne of carbon.
The C$100k/tonne carbon price estimate is probably low
We believe our assessment of the effective carbon price of the emissions cap at C$96,000+/tonne to be conservative for the following reasons.
First, it assumes Canadian heavy oil will be displaced in global markets by an average, archetypal crude. In fact, it would be displaced by other heavy crudes from places like Venezuela, Mexico, and Iraq (see Figure 4), which have higher average emissions per barrel than Canadian oil sands crudes. In such a circumstance, global emissions would actually rise and the price per carbon tonne from an emissions cap on oil sands production would also effectively be infinite.
Secondly, emissions cap impact assumptions by the PBO are likely conservative. Those by ECCC, based on a particular scenario outlook, are already outdated. ECCC assumed a production loss of only 0.7 percent by 2030, with oil sands production hitting approximately 3.7 million barrels (MMbbls) per day of bitumen production in 2030. According to S&P Global analysis, that level is likely to be hit this year.[2]
S&P further forecasts oil sands production to reach 4.0 MMbbls by 2030, or about 300,000 barrels more than it produces today. This would represent a far lower production growth rate than the oil sands have experienced in the past five years. But assuming the S&P forecast is correct, production would need to decline in the oil sands by 8 percent to meet the emissions cap requirements. PBO assumed only a 5.4 percent overall oil and gas production loss and ECCC assumed only 0.7 percent, while Conference Board of Canada assumed an 11.1 percent loss and Deloitte assumed 11.5 percent (see Table 1). Production numbers to date more closely align with Conference Board of Canada and Deloitte projections.
Let’s make the Canadian oil and gas sector better, not smaller
The Canadian oil and gas sector, and in particular the oil sands, has a responsibility to do their part to reduce emissions while maintaining competitive businesses that can support good Canadian jobs, provide government revenues and diversify exports. The oil sands sector has re-invested for decades in continuous improvements to drive down production costs while improving its emissions per barrel.
It is hard to conceive of a more expensive and divisive way to reduce emissions from the sector and from the Canadian economy than the proposed emissions cap. Other expensive programs, such as Norway’s EV subsidies, the United Kingdom’s offshore wind contracts-for-difference, Germany’s Energiewende feed-in-tariffs and surcharges, and US Inflation Reduction Act investment tax credits, don’t come close to the high costs of the emissions cap on a price-per-tonne of carbon abated basis.
The emissions cap, as currently proposed, will make Canada’s oil and gas sector significantly less competitive, harm investment, and undermine Canada’s vision to be an energy superpower. This policy will also reduce the oil and gas sector’s capacity to invest in technologies that drive additional emission reductions, such as solvents and carbon capture, especially in our current lower price environment. As such it is more likely to undermine climate action than support it.
The federal and provincial governments have come together to advance a vision for Canadian energy in the past. In this moment, they have the opportunity once again to find real solutions to the climate challenge while harnessing the energy sector to advance Canada’s economic well-being, productivity, and global energy security.
About the author
Heather Exner-Pirot is Director of Energy, Natural Resources, and Environment at the Macdonald-Laurier Institute.
Immigration
Mass immigration can cause enormous shifts in local culture, national identity, and community cohesion

By Geoff Russ for Inside Policy
It matters where immigrants come from, why they choose Canada, and how many are arriving from any single country. When it comes to countries of origin, immigration streams into Canada have become wildly unbalanced over the last decade.
Few topics have animated Canadians more than immigration in the past year.
There is broad consensus among the public that the annual intake of newcomers must fall, and polling shows both native-born and immigrant citizens agree on this. In Ottawa, the Conservative opposition has called for lower numbers, and the Liberal government ostensibly concurs.
While much of the discussion surrounding immigration has focused on economic factors like affordability and the shrinking housing supply, less attention has been paid to the cultural and political changes of welcoming more than 5 million people into the country since 2014.
Specifically, attention must be paid to the possible outcomes of importing hundreds of thousands of people from regions embroiled by war or prone to conflict. This is a necessity as digital technology proliferates and guarantees the world will be interconnected, but not united.
Mass immigration brings in far more than just people. It can cause enormous shifts in local culture, national identity, political allegiances, and community cohesion.
It matters where immigrants come from, why they choose Canada, and how many are arriving from any single country. When it comes to countries of origin, immigration streams into Canada have become wildly unbalanced over the last decade.
In 2023, almost 140,000 people immigrated to Canada from India, while the second-largest intake came from China, with 31,770 people.
This new trend is at odds with Canada’s historical immigration policies, which were more evenly weighted by country. In 2010, the top three national pools of immigration were the Philippines at 38,300 newcomers, India with 33,500, and China with 31,800.
Other countries that Canada has received increasing numbers of migrants from includes Syria, Pakistan, and Nigeria.
Past federal governments took consideration for details like economic needs and capacity for integration. Canadian immigration policy in 2025 should take into account modern communications and conflicts within certain regions as well.
21st century technology continues to advance and innovate at dizzying speeds, giving rise to immersive social platforms and instant messaging platforms like WhatsApp or Signal. This has brought the world closer together, but rather than promoting peace and understanding, it has amplified foreign conflicts and brought them to our own backyards.
Tens of thousands of migrants from the Levant have arrived since 2015, a region where anti-Zionism is deeply ingrained in the cultures, as well as full-blown antisemitism.
Since the outbreak of the Israel-Hamas War in 2023, the entire West has borne witness to antisemitic violence in Europe and North America, often perpetrated by ideologically motivated migrants.
Earlier this year, a Syrian migrant in Germany went on a stabbing spree with the intent of murdering Jews, while last September, Canadian police foiled the plot of a Pakistani man in Ontario who had planned to commit a mass killing of Jews in New York City.
Canada’s political culture has been profoundly affected by these same waves, with demographic changes forcing the federal government to alter its longstanding foreign policy positions. For example, the newly-minted Minister of Industry Mélanie Joly allegedly remarked last year that her shifting stance on the Israel-Hamas war was due to the “demographics” of her Montreal riding.
Montreal itself has become a hotbed of anti-Israeli and anti-semitic violence. Riots, property damage, and the storming of the McGill University campus have been carried out by radicals inspired by Hamas and their allies.
In 1968, the great Canadian thinker Marshall McLuhan co-authored War and Peace in the Global Village, which warned of the consequences of modern technologies erasing the boundaries of the world. McLuhan explicitly cautioned that technology would make the world smaller, and lead to conflict in his theorized global village.
Today, that village is one where Jewish students are routinely harassed on college campuses in Vancouver and Toronto, while synagogues are burnt to the ground in Melbourne. It does not matter whether the victims are Israeli or not. They are seen by their assailants as legitimate targets as part of an enemy tribe.
On May 21, two staffers at the Israeli embassy in Washington DC were shot dead by a man shouting pro-Palestinian slogans.
These sorts of imported feuds go beyond the Middle East. Global tensions in regions like the Indian subcontinent present another threat of foreign-inspired and funded violence, as well as undue political shifts.
India and Pakistan are locked in a long running standoff over the disputed territory of Kashmir.
Last month, several tourists were murdered in Kashmir by militants that India accused Pakistan of backing, leading to several low-level exchanges between the Indian and Pakistani militaries before a ceasefire was brokered. Tensions are far from dissipated, and the possibility of a full-scale confrontation between India and Pakistan remains high.
Considering those two rivals have massive diasporas in the West, a potential war on the subcontinent could radically change domestic politics in countries in Canada, Australia, and Britain.
In 2022, violent clashes broke out between Hindu and Muslim youths in the British city of Leicester following a cricket match between India and Pakistan. The street battles lasted for weeks, and threatened to restart later that year following an escalation in India and Pakistan’s clash over Kashmir. In London, demonstrators from the Pakistani and Indian communities came close to violence.
If a sporting rivalry can inspire hooliganism, a war will spark something far worse, and the globalization of the Israel-Gaza conflict is a glimpse into what that might look like.
There is historical precedent in Canada for how overseas conflicts affect domestic politics.
During the 19th century, hundreds of thousands of Irish—both Catholic and Protestant—emigrated to Canada before and after Confederation in 1867. They brought their religious feuds with them.
The militantly anti-Catholic Orange Order, run by Protestants, became one of the most powerful political forces in Ontario. They held a virtual monopoly on municipal politics in Toronto, excluded Catholics from jobs in the public service, and took part in brawls with the city’s Irish Catholic community for more than 100 years.
Thomas D’Arcy McGee, one of the Fathers of Confederation and an Irish Catholic migrant, was murdered for speaking out against the republican Fenian Brotherhood, which had infiltrated politics both in Canada and the United States.
Integration throughout successive generations mitigates and even practically eliminates the impact of imported conflicts. This was the case with the Irish sectarian divide, though it took over a century to fade away.
Worth noting is that roughly 300,000 Ukrainian refugees currently reside in Canada, having been admitted under a special visa program following the Russian invasion in 2022. It is intended to be temporary, with the expectation of repatriation once a stable peace returns to Ukraine.
Similarly to Irish-Canadians, the vast majority of the established Ukrainian-Canadian community has its roots in pre-modern Canada, and is largely well-integrated into the country’s social fabric. To date, there has been no major violence or anti-social harms inflicted upon their Russian-Canadian counterparts despite the war, or vice-versa.
Furthermore, the Canadian government has a longstanding close relationship with Kyiv, and there is far more trust and transparency regarding intent and collaboration. This is not the case with governments like China and India, the former of whom actively interferes in our elections, and the latter of which has been accused of assassinating dissidents on Canadian soil.
The existence of the iPhone, the internet, and opportunistic foreign governments makes it incredibly dangerous to not change course. That is not to imply that the average migrant is an active foreign agent. But the sheer quantity makes vetting them all a challenge.
Mitigating these threats requires strategic planning when crafting immigration policy.
Other parts of the world like Southeast Asia, Southern Europe, and Latin America are relatively stable and peaceful and are potential sources of newcomers with far lower risk of foreign interference and diasporic violence.
At-play is the stability, unity, and integrity of our political system. Canadian politics must remain fully Canadian in its focus and priorities. That cannot happen if we sleepwalk into becoming a battleground for the rest of the world.
Geoff Russ is a writer and policy analyst, and a contributor for the Macdonald-Laurier Institute.
-

 Alberta10 hours ago
Alberta10 hours agoAlberta Independence Seekers Take First Step: Citizen Initiative Application Approved, Notice of Initiative Petition Issued
-
 Crime9 hours ago
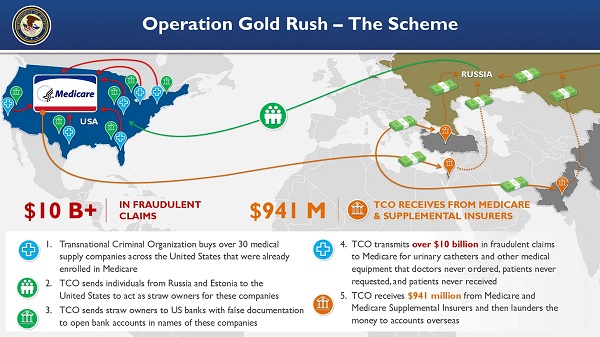
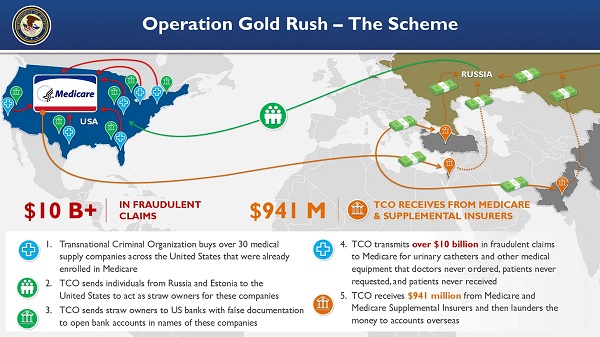
Crime9 hours agoNational Health Care Fraud Takedown Results in 324 Defendants Charged in Connection with Over $14.6 Billion in Alleged Fraud
-

 Health8 hours ago
Health8 hours agoRFK Jr. Unloads Disturbing Vaccine Secrets on Tucker—And Surprises Everyone on Trump
-

 Bruce Dowbiggin11 hours ago
Bruce Dowbiggin11 hours agoThe Game That Let Canadians Forgive The Liberals — Again
-

 Alberta1 day ago
Alberta1 day agoCOVID mandates protester in Canada released on bail after over 2 years in jail
-

 Crime2 days ago
Crime2 days agoProject Sleeping Giant: Inside the Chinese Mercantile Machine Linking Beijing’s Underground Banks and the Sinaloa Cartel
-

 Alberta2 days ago
Alberta2 days agoAlberta uncorks new rules for liquor and cannabis
-

 Business1 day ago
Business1 day agoCanada’s loyalty to globalism is bleeding our economy dry