Health
RFK Jr. purges CDC vaccine panel, citing decades of ‘skewed science’

From LifeSiteNews
By Robert Jones
RFK Jr.’s HHS has removed all Advisory Committee on Immunization Practices members in an effort to reset public confidence in vaccine oversight.
Health and Human Services Secretary Robert F. Kennedy Jr. has dismissed every member of the CDC’s top vaccine advisory panel, citing what he described as a “decades” of “conflicts of interest” and “skewed science” in the vaccine regulatory system.
RFK Jr.’s abrupt decision to “retire” all 17 members of the Advisory Committee on Immunization Practices (ACIP) was announced in a Wall Street Journal op-ed Monday and confirmed by HHS shortly thereafter.
The move marks the most sweeping reform to federal vaccine policy in years and follows months of internal reviews and mounting public skepticism.
Kennedy accused the ACIP of being “little more than a rubber stamp for any vaccine,” claiming “it has never recommended against a vaccine.”
“The public must know that unbiased science guides the recommendations from our health agencies,” Kennedy wrote. “This will ensure the American people receive the safest vaccines possible.”
ACIP holds the power to influence which vaccines are recommended by the CDC and covered by insurers. But according to Kennedy, it has failed in its duty to protect the public.
He cited multiple government investigations—dating back to 2000 and 2009—finding that ACIP members were routinely advising on products from pharmaceutical firms with which they had financial ties. Committee members were also issued conflict-of-interest waivers from the CDC.
Kennedy pointed to the 1997 vote approving the Rotashield vaccine – later withdrawn for causing severe bowel obstructions in infants – as a case study in regulatory failure. Four of the eight members who voted for it had financial stakes in rotavirus vaccines under development.
He explained “retiring” the 17 members, “some of whom were last-minute appointees of the Biden administration,” by saying that without such a move, “the Trump administration would not have been able to appoint a majority” until 2028.
CNBC warned the firings could “undermine vaccinations” and erode trust among scientists. But Kennedy, a longtime vaccine industry sceptic, maintains that trust has already “collapsed” – and that restoring it requires nothing less than a full reset.
Under Kennedy’s leadership, HHS has already halted recommendations for routine COVID-19 shots for healthy children and pregnant women and cancelled COVID-era programs to fast-track new vaccines.
It remains unclear who will replace the outgoing ACIP members, though HHS confirmed the committee will still meet later this month, now under new leadership.
“The new members won’t directly work for the vaccine industry,” he promised. “They will exercise independent judgment, refuse to serve as a rubber stamp, and foster a culture of critical inquiry—unafraid to ask hard questions.”
Business
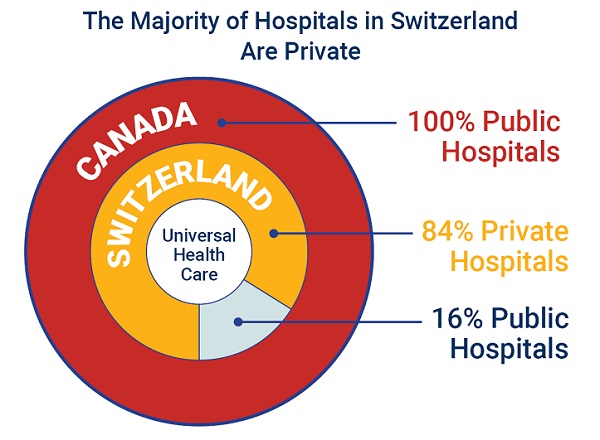
84% of Swiss hospitals and 60% of hospitalizations are in private facilities, and they face much lower wait times
From the Fraser Institute
If Canada reformed to emulate Switzerland’s approach to universal health care, including its much greater use of private sector involvement, the country would deliver far better results to patients and reduce wait times, finds a new study published today by the Fraser Institute, an independent, non-partisan Canadian policy think-tank.
“The bane of Canadian health care is lack of access to timely care, so it’s critical to look to countries like Switzerland with more successful universal health care,” said Yanick Labrie, senior fellow at the Fraser Institute and author of Integrating Private Health Care Into Canada’s Public System: What We Can Learn from Switzerland. The study highlights how Switzerland successfully integrates the private sector into their universal health-care system, which consistently outperforms Canada on most health-care metrics, including wait times.
For example, in 2022, the percentage of patients who waited less than two months for a specialist appointment was 85.3 per cent in Switzerland compared to just 48.3 per cent in Canada.
In Switzerland, 84.2 per cent of all hospitals are private (either for-profit or not-for profit) institutions, and the country’s private hospitals provide 60.2 per cent of all hospitalizations, 60.9 per cent of all births, and 67.1 per cent of all operating rooms.
Crucially, Swiss patients can obtain treatment at the hospital of their choice, whether located inside or outside their geographic location, and hospitals cannot discriminate against patients, based on the care required.
“Switzerland shows that a universal health-care system can reconcile efficiency and equity–all while being more accessible and responsive to patients’ needs and preferences,” Labrie said.
“Based on the success of the Swiss model, provinces can make these reforms now and help improve Canadian health care.”

Integrating Private Health Care into Canada’s Public System: What We Can Learn from Switzerland
- Access to timely care remains the Achilles’ heel of Canada’s health systems. To reduce wait times, some provinces have partnered with private clinics for publicly funded surgeries—a strategy that has proven effective, but continues to spark debate in Canada.
- This study explores how Switzerland successfully integrates private health care into a universal public system and considers what Canada can learn from this model.
- In Switzerland, universal coverage is delivered through a system of managed competition among 44 non-profit private insurers, while decentralized governance allows each of the 26 cantons to coordinate and oversee hospital services in ways that reflect local needs and priorities.
- Nearly two-thirds of Swiss hospitals are for-profit institutions; they provide roughly half of all hospitalizations, births, and hospital beds across the country.
- All hospitals are treated equally—regardless of legal status—and funded through the same activity-based model, implemented nationwide in 2012.
- The reform led to a significant increase in the number of cases treated without a corresponding rise in expenditures per case, suggesting improved efficiency, better use of resources, and expanded access to hospital care.
- The average length of hospital stay steadily decreased over time and now stands at 4.87 days in for-profit hospitals versus 5.53 days in public ones, indicating faster patient turnover and more streamlined care pathways.
- Hospital-acquired infection rates are significantly lower in private hospitals (2.7%) than in public hospitals (6.2%), a key indicator of care quality.
- Case-mix severity is as high or higher in private hospitals, countering the notion that they only take on simpler or less risky cases.
- Patient satisfaction is slightly higher in private hospitals (4.28/5) than in public ones (4.17/5), reflecting strong user experience across multiple dimensions.
- Canada could benefit from regulated competition between public and private providers and activity-based funding, without breaching the Canada Health Act.

Health
RFK Jr. appoints Robert Malone, Martin Kulldorff, other COVID shot critics to overhauled CDC vaccine panel
From LifeSiteNews
By Robert Jones
Health and Human Services Secretary Robert F. Kennedy Jr. has announced eight appointments for the CDC’s top vaccine advisory panel, following his dismissal of all 17 previous members, citing a need to rebuild public trust in the federal immunization process.
On Monday, I took a major step towards restoring public trust in vaccines by reconstituting the Advisory Committee for Immunization Practices (ACIP). I retired the 17 current members of the committee. I’m now repopulating ACIP with the eight new members who will attend ACIP’s…
— Secretary Kennedy (@SecKennedy) June 11, 2025
RFK Jr. said the new Advisory Committee on Immunization Practices (ACIP) will demand “definitive safety and efficacy data” before issuing any new vaccine recommendations and will re-evaluate existing guidance. The restructured panel is set to convene on June 25.
The appointees include several prominent physicians and scientists, including former Harvard epidemiologist Martin Kulldorff and mRNA researcher Robert Malone, both known for their criticism of COVID-19-era public health policy and the COVID-19 shots.
Kulldorff helped draft the Great Barrington Declaration with Jay Bhattacharya and Sunetra Gupta, which called for focused protection rather than mass lockdowns – a position widely debated among epidemiologists. He also spoke out strongly against vaccine passports and mandates, as well as mask mandates and contact tracing. He was dismissed from Harvard in 2024 because of his refusal to receive the COVID-19 injections.
Malone, who conducted early work on mRNA vaccine delivery systems, was banned from several platforms for posts deemed “misleading” during the COVID crisis. He has given related interviews on The Joe Rogan Experience and elsewhere and was reinstated on X following Elon Musk’s revision of COVID-19 policies.
Retsef Levi, a professor at MIT, has raised concerns about potential cardiovascular risks linked to COVID-19 mRNA shots and has called for stricter safety monitoring. In 2023, a petition circulated opposing his work, though it did not gain traction.
Other appointees include:
- Joseph Hibbeln, an NIH psychiatrist and nutrition researcher focused on immune and neurodevelopmental health.
- Cody Meissner, a pediatric infectious disease expert with previous experience on both FDA and CDC vaccine panels.
- James Pagano, a veteran emergency physician with decades of clinical experience.
- Vicky Pebsworth, a nurse-scientist with prior FDA vaccine advisory roles and Pacific Region Director of the National Association of Catholic Nurses. She is also a Lay Dominican.
- Michael Ross, an OB-GYN and clinical researcher with a background in immunology and women’s health policy.
Joseph R. Hibbeln, MD, is a psychiatrist and neuroscientist with a career in clinical research, public health policy, and federal service. As former Acting Chief of the Section on Nutritional Neurosciences at the National Institutes of Health, he led research on immune regulation, neurodevelopment, and mental health. His work has informed U.S. public health guidelines, particularly in maternal and child health. With more than 120 peer-reviewed publications and extensive experience in federal advisory roles, Dr. Hibbeln brings expertise in immune-related outcomes, psychiatric conditions, and evidence-based public health strategies.
Martin Kulldorff, MD, PhD, is a biostatistician and epidemiologist formerly at Harvard Medical School and a leading expert in vaccine safety and infectious disease surveillance. He has served on the Food and Drug Administration’s Drug Safety and Risk Management Advisory Committee and the CDC’s Vaccine Safety Subgroup of the Advisory Committee on Immunization Practices, where he contributed to national vaccine safety monitoring systems. Dr. Kulldorff developed widely used tools such as SaTScan and TreeScan for detecting disease outbreaks and vaccine adverse events. His expertise includes statistical methods for public health surveillance, immunization safety, and infectious disease epidemiology. He has also been an influential voice in public health policy, advocating for evidence-based approaches to pandemic response.
Retsef Levi, PhD, is the Professor of Operations Management at the MIT Sloan School of Management and a leading expert in healthcare analytics, risk management, and vaccine safety. He has served as Faculty Director of MIT Sloan’s Food Supply Chain Analytics and Sensing Initiative and co-led the Leaders for Global Operations Program. Dr. Levi has collaborated with public health agencies to evaluate vaccine safety, including co-authoring studies on mRNA COVID-19 vaccines and their association with cardiovascular risks. His research has contributed to discussions on vaccine manufacturing processes, safety surveillance, and public health policy. Dr. Levi has also served on advisory committees and engaged in policy discussions concerning vaccine safety and efficacy. His expertise spans healthcare systems optimization, epidemiologic modeling, and the application of AI and data science in public health. Dr. Levi’s work continues to inform national and international debates on immunization safety and health system resilience.
Robert W. Malone, MD, is a physician-scientist and biochemist known for his early contributions to mRNA vaccine technology. He conducted foundational research in the late 1980s on lipid-mediated mRNA delivery, which laid the groundwork for later developments in mRNA-based therapeutics. Dr. Malone has held academic positions at institutions including the University of California, Davis, and the University of Maryland, and has served in advisory roles for the U.S. Department of Health and Human Services and the Department of Defense. His expertise spans molecular biology, immunology, and vaccine development.
Cody Meissner, MD, is a Professor of Pediatrics at the Geisel School of Medicine at Dartmouth and a nationally recognized expert in pediatric infectious diseases and vaccine policy. He has served as Section Chief of Pediatric Infectious Disease at Dartmouth-Hitchcock Medical Center and has held advisory roles with both the Centers for Disease Control and Prevention (CDC) and the Food and Drug Administration (FDA). Dr. Meissner has been a voting member of the CDC’s Advisory Committee on Immunization Practices and the FDA’s Vaccines and Related Biological Products Advisory Committee, where he has contributed to national immunization guidelines and regulatory decisions. His expertise spans vaccine development, immunization safety, and pediatric infectious disease epidemiology. Dr. Meissner has also been a contributing author to American Academy of Pediatrics policy statements and immunization schedules, helping shape national standards for pediatric care.
James Pagano, MD, is a board-certified Emergency Medicine physician with over 40 years of clinical experience following his residency at UCLA. He has worked in diverse emergency settings, from Level 1 trauma centers to small community hospitals, caring for patients across all age groups, including infants, pregnant women, and the elderly. Dr. Pagono served on multiple hospital committees, including utilization review, critical care, and medical executive boards. He is strong advocate for evidence-based medicine.
Vicky Pebsworth, OP, PhD, RN, earned a doctorate in public health and nursing from the University of Michigan. She has worked in the healthcare field for more than 45 years, serving in various capacities, including critical care nurse, healthcare administrator, health policy analyst, and research scientist with a focus on public health policy, bioethics, and vaccine safety. She is the Pacific Region Director of the National Association of Catholic Nurses. She is a former member of the Food and Drug Administration’s Vaccine and Related Biological Products Advisory Committee and the National Vaccine Advisory Committee’s 2009 H1N1 Vaccine Safety Risk Assessment Working Group and Vaccine Safety Working Group (Epidemiology and Implementation Subcommittees).
Michael A. Ross, MD, is a Clinical Professor of Obstetrics and Gynecology at George Washington University and Virginia Commonwealth University, with a career spanning clinical medicine, research, and public health policy. He has served on the CDC’s Advisory Committee for the Prevention of Breast and Cervical Cancer, where he contributed to national strategies for cancer prevention and early detection, including those involving HPV immunization. With research experience in hormone therapies, antibiotic trials, and immune-related conditions such as breast cancer prevention, Dr. Ross has engaged in clinical investigations with immunologic relevance. He has advised major professional organizations, including the American College of Obstetricians and Gynecologists, and contributed to federal advocacy efforts around women’s health and preventive care. His continued service on biotech and healthcare boards reflects his commitment to advancing innovation in immunology, reproductive medicine, and public health.
Kennedy framed the move as part of a broader campaign to remove conflicts of interest and restore credibility to federal vaccine recommendations. Just a few days ago, he accused the panel of having been “little more than a rubber stamp for any vaccine” and pledged that the new members would not have direct ties with the vaccine industry.
The new ACIP, he said, will be focused on what RFK called “gold-standard science” and “common sense.” The June meeting will mark the beginning of its work.
-
 Crime2 days ago
Crime2 days agoOntario Police’s Record Fentanyl Bust Suggests Cartel–Iranian–PRC-Supplied Nexus from Ottawa to Hamilton Along Six Nations Corridor
-

 Business2 days ago
Business2 days agoTelegram founder Pavel Durov exposes crackdown on digital privacy in Tucker Carlson interview
-

 Alberta2 days ago
Alberta2 days agoAlbertans need clarity on prime minister’s incoherent energy policy
-

 Business2 days ago
Business2 days agoVanishing lines and fading logic
-

 Business1 day ago
Business1 day agoAudit report reveals Canada’s controversial COVID travel app violated multiple rules
-

 Education2 days ago
Education2 days agoOur sweetest success yet: Smile Cookie Campaign breaks record
-

 Energy1 day ago
Energy1 day agoHow to realize Canada’s ambitions as an energy superpower
-
 illegal immigration2 days ago
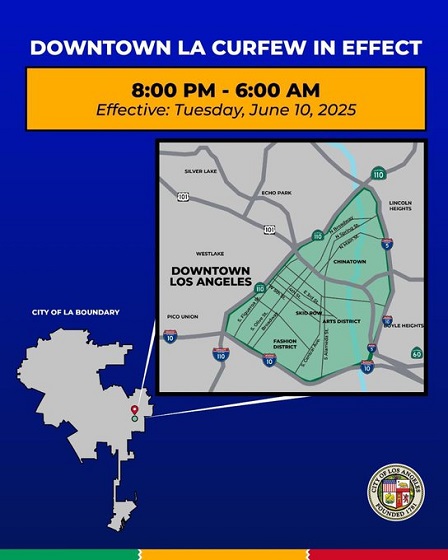
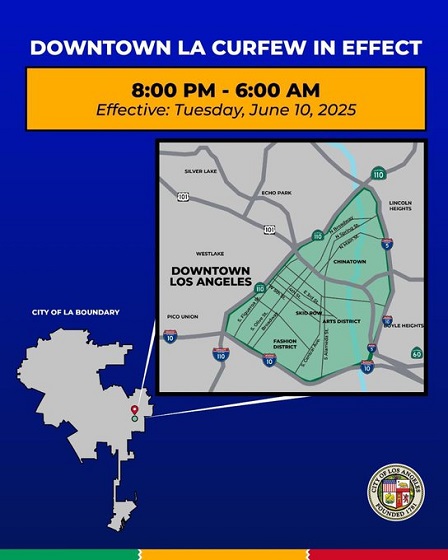
illegal immigration2 days agoLAPD arrests dozens following downtown L.A. curfew






