Health
RFK Jr. Says Trump Just Did What No Democrat Ever Had the Guts to Do

The Vigilant Fox and Overton |
This might be the biggest shake-up in American healthcare history.
President Trump just did what every other politician only talked about—he took a sledgehammer to Big Pharma. With the stroke of a pen, he signed an executive order that could slash drug prices by as much as 90%.
And then RFK Jr. stepped up and revealed why no one else—not even Bernie Sanders—ever followed through.
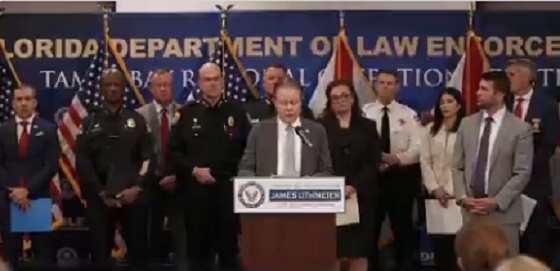
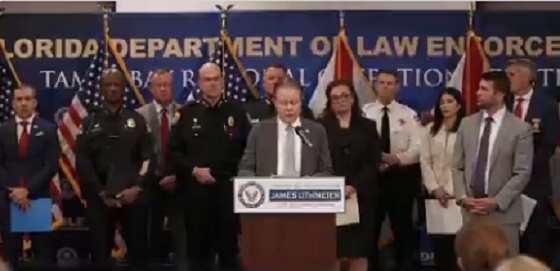
Standing before reporters and his healthcare team, President Trump announced the most aggressive move on drug pricing America has ever seen. The plan? To cut prescription drug costs by up to 90%—a direct strike against the industry that’s drained American families dry for years.
“Starting today, the United States will no longer subsidize the health care of foreign countries, which is what we were doing,” Trump said. “We were subsidizing others’ health care, countries where they paid a small fraction of what for the same drug that what we pay many, many times more for.”
This wasn’t just about reining in corporate greed. Trump laid it out clearly: this was a global scam, and America was the one footing the bill.
“And [we] will no longer tolerate profiteering and price gouging from Big Pharma,” he added. “But again, it was really the countries that forced Big Pharma to do things that frankly, I’m not sure they really felt comfortable doing, but they’ve gotten away with it, these countries, European Union has been brutal, brutal.”
Trump promised that would change. “So for the first time in many years, we’ll slash the cost of prescription drugs and we will bring fairness to America.”
How much cheaper? “If you think of a drug that is sometimes ten times more expensive, it’s much more than the 59%… but between 59 and 80, and I guess even 90%.”
For struggling families, this wasn’t just reform. It was real relief.
Then came the reveal that changed everything. HHS Secretary Robert F. Kennedy Jr. stood beside the president and exposed one of Washington’s best-kept secrets. It wasn’t just corruption—it was betrayal.
“This is an extraordinary day,” Kennedy began. “This is an issue that, you know, I grew up in the Democratic Party, and every major Democratic leader for 20 years has been making this promise to the American people.”
He pointed straight to Bernie Sanders, who made drug pricing the core of his presidential campaigns. “This was the fulcrum of Bernie Sanders runs for presidency, that he was going to eliminate this discrepancy between Europe and the United States.”
But none of them actually meant to fix it.
“As it turns out, none of them were doing it. And it’s one of these promises that politicians make to their constituents, knowing that they’ll never have to do it.”
Why not? Because the system was never meant to be fixed.
“There’s at least one pharmaceutical lobbyist for every congressman, every Senator on Capitol Hill, and every member of the Supreme Court,” Kennedy said.
“There has never been a president more willing to stand up to the oligarchs than President Donald Trump,” he added. “And I’m very, very proud of you, Mr. President, for your courage, for I’ll say it because I don’t want to be crude, your intestinal fortitude, your stiff spine and your willingness to stand up for the American people.”
With one line, RFK Jr. shattered the bipartisan charade—and gave Trump credit no Democrat had the guts to say out loud.
If you’re not following me yet, you’re missing the real story behind the headlines.
I post critical updates daily. Subscribe now and stay ahead of the curve.
Then Dr. Oz came with a line that hit hard.
“This is the most powerful executive order on pharmacy pricing and healthcare ever in the history of our nation.”
He explained how Americans were stuck paying five to ten times more than Europeans for the exact same drugs—and why that ends now.
“It’s only happening because we have a president with the fortitude, the guts to stand up to the withering criticism and lobbying that’s going to occur as soon as folks hear about the executive order,” said the head of CMS.
Dr. Oz made it personal. “On behalf of the child in Philadelphia with a $1,000-a-month drug, or the older woman in L.A. who can’t afford her blood thinner—I’m going to thank President Trump. God bless you for having the guts to take on this industry.”
He said Trump’s plan will force other countries to start paying their fair share, just like with NATO.
“When President Trump said you’ve got to pay a little more, they came up. The same thing we believe will happen here.”
Negotiations with drug companies start in 30 days. For the first time ever, prices will be tied to global benchmarks.
“We’re going to be able to get the pharmaceutical industry whole—and finally pay the appropriate amount.”
Then NIH Director Jay Bhattacharya took the mic and called it what it was: long overdue.
“What President Trump has done is a historic measure that should have been done a long time ago.”
He explained the economics behind the scam. “One thing that’s really, really simple in economics is that when you have a persistent price difference for the same product between two countries, there’s something deeply wrong.”
Bhattacharya said Americans were being used to fund global research and development, and that ends now.
“Right now, what’s happening is the American people are subsidizing, in a large fraction, the research and development efforts for drug companies around the world, by the higher prices that we pay.”
“With this new order, Europe will share the burden of that.”
This wasn’t new information. The facts have been known for decades. But no one acted—until now.
“We’re standing up for the American consumer who’s been paying far too high prices for far too long.”
“And nothing has been done about it until this moment.”
He turned to the president and said, “I’m really, really proud, President Trump, that you have done this, and I’m really proud to be included in this and looking forward to the work ahead.”
And just before signing, Trump made it clear: Democrats were now in a tough spot.
“We’re now, on top of the tax cuts and regulation cuts, all the things, now you’re going to say that the price of your medicine is going down by 60, 70, 80%. You’re going to vote against it?”
“I think a lot of Democrats will be forced to do something that their leaders are going to beg them not to do, and that’s vote for the bill.”
“I don’t see how they can vote against it.”
That’s when ABC jumped in with a question about a jet from Qatar, implying it was a personal gift to Trump.
Without skipping a beat, Trump fired back. “You’re ABC fake news, right?”
“Let me tell you, you should be embarrassed asking that question. They’re giving us a free jet. I could say no, no, no. Don’t give us. I want to pay you a billion or $400 million or whatever it is. Or I can say thank you very much.”
When she pressed again, Trump hit even harder.
“It’s not a gift to me, it’s a gift to the Department of Defense. You should know better. Because you’ve been embarrassed enough, and so has your network.”
“Your network is a disaster. ABC is a disaster,” Trump added.
Finally, Trump lifted the bill and called Kennedy up beside him. “Here is the bill, Bobby, come on over here.”
Thanks for reading! This post took time and care to put together, and we did our best to give this story the coverage it deserved.
If you like my work and want to support me and my team and help keep this page going strong, the most powerful thing you can do is sign up for the email list and become a paid subscriber.
Your monthly subscription goes further than you think. Thank you so much for your support.
Brownstone Institute
FDA Exposed: Hundreds of Drugs Approved without Proof They Work

From the Brownstone Institute
By
The US Food and Drug Administration (FDA) has approved hundreds of drugs without proof that they work—and in some cases, despite evidence that they cause harm.
That’s the finding of a blistering two-year investigation by medical journalists Jeanne Lenzer and Shannon Brownlee, published by The Lever.
Reviewing more than 400 drug approvals between 2013 and 2022, the authors found the agency repeatedly ignored its own scientific standards.
One expert put it bluntly—the FDA’s threshold for evidence “can’t go any lower because it’s already in the dirt.”
A System Built on Weak Evidence
The findings were damning—73% of drugs approved by the FDA during the study period failed to meet all four basic criteria for demonstrating “substantial evidence” of effectiveness.
Those four criteria—presence of a control group, replication in two well-conducted trials, blinding of participants and investigators, and the use of clinical endpoints like symptom relief or extended survival—are supposed to be the bedrock of drug evaluation.
Yet only 28% of drugs met all four criteria—40 drugs met none.
These aren’t obscure technicalities—they are the most basic safeguards to protect patients from ineffective or dangerous treatments.
But under political and industry pressure, the FDA has increasingly abandoned them in favour of speed and so-called “regulatory flexibility.”
Since the early 1990s, the agency has relied heavily on expedited pathways that fast-track drugs to market.
In theory, this balances urgency with scientific rigour. In practice, it has flipped the process. Companies can now get drugs approved before proving that they work, with the promise of follow-up trials later.
But, as Lenzer and Brownlee revealed, “Nearly half of the required follow-up studies are never completed—and those that are often fail to show the drugs work, even while they remain on the market.”
“This represents a seismic shift in FDA regulation that has been quietly accomplished with virtually no awareness by doctors or the public,” they added.
More than half the approvals examined relied on preliminary data—not solid evidence that patients lived longer, felt better, or functioned more effectively.
And even when follow-up studies are conducted, many rely on the same flawed surrogate measures rather than hard clinical outcomes.
The result: a regulatory system where the FDA no longer acts as a gatekeeper—but as a passive observer.
Cancer Drugs: High Stakes, Low Standards
Nowhere is this failure more visible than in oncology.
Only 3 out of 123 cancer drugs approved between 2013 and 2022 met all four of the FDA’s basic scientific standards.
Most—81%—were approved based on surrogate endpoints like tumour shrinkage, without any evidence that they improved survival or quality of life.
Take Copiktra, for example—a drug approved in 2018 for blood cancers. The FDA gave it the green light based on improved “progression-free survival,” a measure of how long a tumour stays stable.
But a review of post-marketing data showed that patients taking Copiktra died 11 months earlier than those on a comparator drug.
It took six years after those studies showed the drug reduced patients’ survival for the FDA to warn the public that Copiktra should not be used as a first- or second-line treatment for certain types of leukaemia and lymphoma, citing “an increased risk of treatment-related mortality.”
Elmiron: Ineffective, Dangerous—And Still on the Market
Another striking case is Elmiron, approved in 1996 for interstitial cystitis—a painful bladder condition.
The FDA authorized it based on “close to zero data,” on the condition that the company conduct a follow-up study to determine whether it actually worked.
That study wasn’t completed for 18 years—and when it was, it showed Elmiron was no better than placebo.
In the meantime, hundreds of patients suffered vision loss or blindness. Others were hospitalized with colitis. Some died.
Yet Elmiron is still on the market today. Doctors continue to prescribe it.
“Hundreds of thousands of patients have been exposed to the drug, and the American Urological Association lists it as the only FDA-approved medication for interstitial cystitis,” Lenzer and Brownlee reported.
“Dangling Approvals” and Regulatory Paralysis
The FDA even has a term—”dangling approvals”—for drugs that remain on the market despite failed or missing follow-up trials.
One notorious case is Avastin, approved in 2008 for metastatic breast cancer.
It was fast-tracked, again, based on ‘progression-free survival.’ But after five clinical trials showed no improvement in overall survival—and raised serious safety concerns—the FDA moved to revoke its approval for metastatic breast cancer.
The backlash was intense.
Drug companies and patient advocacy groups launched a campaign to keep Avastin on the market. FDA staff received violent threats. Police were posted outside the agency’s building.
The fallout was so severe that for more than two decades afterwards, the FDA did not initiate another involuntary drug withdrawal in the face of industry opposition.
Billions Wasted, Thousands Harmed
Between 2018 and 2021, US taxpayers—through Medicare and Medicaid—paid $18 billion for drugs approved under the condition that follow-up studies would be conducted. Many never were.
The cost in lives is even higher.
A 2015 study found that 86% of cancer drugs approved between 2008 and 2012 based on surrogate outcomes showed no evidence that they helped patients live longer.
An estimated 128,000 Americans die each year from the effects of properly prescribed medications—excluding opioid overdoses. That’s more than all deaths from illegal drugs combined.
A 2024 analysis by Danish physician Peter Gøtzsche found that adverse effects from prescription medicines now rank among the top three causes of death globally.
Doctors Misled by the Drug Labels
Despite the scale of the problem, most patients—and most doctors—have no idea.
A 2016 survey published in JAMA asked practising physicians a simple question—what does FDA approval actually mean?
Only 6% got it right.
The rest assumed that it meant the drug had shown clear, clinically meaningful benefits—such as helping patients live longer or feel better—and that the data was statistically sound.
But the FDA requires none of that.
Drugs can be approved based on a single small study, a surrogate endpoint, or marginal statistical findings. Labels are often based on limited data, yet many doctors take them at face value.
Harvard researcher Aaron Kesselheim, who led the survey, said the results were “disappointing, but not entirely surprising,” noting that few doctors are taught about how the FDA’s regulatory process actually works.
Instead, physicians often rely on labels, marketing, or assumptions—believing that if the FDA has authorized a drug, it must be both safe and effective.
But as The Lever investigation shows, that is not a safe assumption.
And without that knowledge, even well-meaning physicians may prescribe drugs that do little good—and cause real harm.
Who Is the FDA Working for?
In interviews with more than 100 experts, patients, and former regulators, Lenzer and Brownlee found widespread concern that the FDA has lost its way.
Many pointed to the agency’s dependence on industry money. A BMJ investigation in 2022 found that user fees now fund two-thirds of the FDA’s drug review budget—raising serious questions about independence.

Yale physician and regulatory expert Reshma Ramachandran said the system is in urgent need of reform.
“We need an agency that’s independent from the industry it regulates and that uses high-quality science to assess the safety and efficacy of new drugs,” she told The Lever. “Without that, we might as well go back to the days of snake oil and patent medicines.”
For now, patients remain unwitting participants in a vast, unspoken experiment—taking drugs that may never have been properly tested, trusting a regulator that too often fails to protect them.
And as Lenzer and Brownlee conclude, that trust is increasingly misplaced.
- Investigative report by Jeanne Lenzer and Shannon Brownlee at The Lever [link]
- Searchable public drug approval database [link]
- See my talk: Failure of Drug Regulation: Declining standards and institutional corruption
Republished from the author’s Substack
Health
Red Deer Hospital Lottery 2025 Winners

The Red Deer Regional Health Foundation is thrilled to announce the winners of this year’s Red Deer Hospital Lottery prizes – including the Dream Home, a $100,000.00 cash prize, and Mega Bucks 50.
James Smith of Spruce View has won the $100,000.00 cash prize.
Montey Brehaut of Red Deer has won the Mega Bucks 50 jackpot, taking home $301,702.50.
The grand prize Sorento Custom Homes Dream Home, including furnishings by Urban Barn and worth $1,074,472 – has been awarded to Oscar Gunnlaugson of Sylvan Lake.
The winner announcements took place at noon on June 26 , 2025 – and was streamed live on Facebook from Red Deer Regional Hospital Center.
“We’re excited to celebrate this year’s winners and deeply grateful to everyone who supported the lottery,” said Manon Therriault, CEO of the Red Deer Regional Health Foundation. “Funds raised will directly enhance patient care at Red Deer Regional Hospital Centre.”
This year’s lottery proceeds will fund essential new and replacement equipment, ensuring Red Deer Regional Hospital Center can continue to serve the 500,000 people who rely on it. While plans for the hospital expansion move forward, healthcare doesn’t wait. Patients in our community need access
to life-saving technology today, and supporting Red Deer Hospital Lottery has made that possible.
A full list of winners, including electronics prize recipients, will be posted on July 2 at reddeerhospitallottery.ca.
Winners will also receive instructions on how to claim their prizes by mail.
The keys to the Dream Home will be presented at a special ceremony this summer.
-

 Bruce Dowbiggin16 hours ago
Bruce Dowbiggin16 hours agoWhat Connor Should Say To Oilers: It’s Not You. It’s Me.
-

 Business17 hours ago
Business17 hours agoFederal fiscal anchor gives appearance of prudence, fails to back it up
-

 Business15 hours ago
Business15 hours agoThe Passage of Bill C-5 Leaves the Conventional Energy Sector With as Many Questions as Answers
-
 Alberta13 hours ago
Alberta13 hours agoAlberta poll shows strong resistance to pornographic material in school libraries
-

 Business11 hours ago
Business11 hours agoCanada should already be an economic superpower. Why is Canada not doing better?
-
 Crime12 hours ago
Crime12 hours agoFlorida rescues 60 missing kids in nation’s largest-ever operation
-

 Banks14 hours ago
Banks14 hours agoScrapping net-zero commitments step in right direction for Canadian Pension Plan
-

 Business2 days ago
Business2 days agoBehind the latest CPI Numbers: Inflation Slows, But Living Costs Don’t









