Alberta
Province says improving primary health care system will take pressure off emergency care
Strengthening health care: Improving access for all
Alberta’s government is stabilizing and strengthening primary health care across the province so that everyone can access care when and where they need it.
Primary health care is the first point of contact Albertans have with the health care system, and includes health professionals such as family doctors, nurse practitioners and pharmacists.
Last fall, health care leaders, Indigenous partners and experts from across Canada and around the world came together to form advisory panels as part of the Modernizing Alberta’s Primary Health Care System (MAPS) initiative. The panels identified immediate, medium- and long-term improvements to strengthen Alberta’s primary health care system.
Alberta’s government will begin moving forward on the recommendations in the final report to improve access to primary health care for all Albertans. The recommendations will be implemented through a phased approach, with several moving forward immediately, followed by medium- and longer-term improvements that will enhance community-based primary health care across Alberta.
“Today marks an important step in the work I am undertaking to enhance primary care as the foundation of our health care system. The Modernizing Alberta’s Primary Health Care System (MAPS) reports clearly identify the challenges our system is facing, and their release signals this government’s commitment to take immediate and ongoing action to support and stabilize primary health care in our province. I look forward to the ongoing work of implementing needed changes with our health care partners and providers.”
Several immediate actions are being taken, all of which are consistent with recommendations from the panels. These actions are critical to ensuring Albertans have better access to health care when and where they need it. Alberta Health continues to work toward implementing recommendations over the medium and long term.
“The MAPS recommendations represent a huge leap forward for our primary health system – strengthening and clarifying governance, community involvement, and recognizing the importance of integrated team-based care that allows Albertans to access primary care from the most appropriate team member at the right time, in the right place. This is how we can ensure equitable access to care across our province.”
Strengthening primary health care
Alberta’s government is acting immediately on recommendations to improve primary health care and increase Albertans’ access to the medical care they need, including:
- Creating a primary health care division within Alberta Health.
- Allocating $57 million over three years to provide family doctors and nurse practitioners with support to help manage their increasing number of patients. Each provider has the potential to receive up to $10,000 annually.
- Working with the Alberta Medical Association to create a task force to recommend a new payment model for family physicians that encourages comprehensive primary care – where a patient has a regular family doctor who they develop a long-term relationship with and who works with them to ensure all their health care needs are met.
- Developing a memorandum of understanding with the Alberta Medical Association to collaborate on a transition to a new physician compensation model, modernize primary care governance and enable family doctors to spend more time with patients and less time on paperwork and immediately stabilize primary care.
- Expanding online mental health services, allowing doctors to bill for virtual mental health checks and therapy, and compensating them for extra time spent with patients virtually.
- Ensuring doctors get paid if patients can’t prove insurance coverage, reducing administrative burden. This is known as “good faith” claims.
- Introducing a payment system that will support nurse practitioners to open their own clinics, take on patients and offer services based on their scope of practice, training and expertise. Nurse practitioners have completed graduate studies ensuring that they are properly trained to examine patients, provide diagnoses and prescribe medication.
“We know that a strong primary health care system is foundational for better health care for Albertans, and that starts with access to a family physician and a team of dedicated providers. Primary care requires dedicated planning, resourcing and coordination. We are pleased to join the task force and believe continued collaboration and immediate action will bring us closer to our collective vision.”
“The Nurse Practitioner Association of Alberta is elated to see the newly released MAPs report, which provides direction for primary care reform and includes the full integration of nurse practitioners. The Government of Alberta is taking a significant and essential step in improving access to primary care for Albertans. This announcement is a win-win for Albertans and nurse practitioners, as it recognizes the valuable contributions of NPs delivering high-quality care for Albertans and their ability to decrease the stress on the health care system. We are excited about the future of primary care in Alberta.”
“These actions are welcome news for rural Alberta. Ensuring Albertans have access to health care professionals when and where they need it is essential. This work will help to solve some of the unique challenges for rural Albertans by encouraging health professions to practise in rural parts of the province.”
Strengthening Indigenous health care
Indigenous Peoples face many barriers to access appropriate health care. To support better health outcomes, the government will build more meaningful connections with Indigenous leaders and communities to identify improvements that reflect the unique nature of their communities. Immediate actions include:
- Creating an Indigenous health division within Alberta Health.
- Creating a $20-million fund for Indigenous communities to design and deliver innovative primary health care services and projects.
- Creating an Indigenous patient complaints investigator and Elders roster to investigate incidences of racism during the delivery of health care and provide culturally safe support to Indigenous patients throughout the patient complaint process.
- Investing in a community-based Indigenous patient navigator program to support Indigenous peoples throughout their health care journey.
“It is unacceptable that Indigenous Peoples continue to face so many barriers when accessing primary health care. It is crucial that all First Nations, Métis and Inuit peoples have equitable access to community-based primary health care that is culturally safe, respects their unique needs and is free of racism. These immediate actions will help us achieve that goal.”
“The panel’s recommendations provide a clear and stable pathway to create a safe, culturally appropriate primary health care system that includes Indigenous people as partners and leaders at every stage of the development, governance and delivery of health care services. The best solutions exist within our respective communities, tailored for our unique needs and priorities. The commitments made today are an important first step toward improving health equity for Indigenous Peoples, regardless of where they live in Alberta.”
Quick facts
- Advisory panels were established through MAPS in fall 2022 to identify primary health care improvements in the short term and over the next 10 years.
- Final reports from the panels were submitted in spring 2023.
- The strategic advisory panel final report contains 11 recommendations to refocus the system around primary health care with an emphasis on:
- access to team-based care
- integration between primary health care and community care
- a foundation of a coordinated and accountable primary health care system
- The Indigenous advisory panel final report contains 22 recommendations under five themes:
- improve health equity for Indigenous Peoples
- address Indigenous racism in health care
- build culturally safer primary health care and an Indigenous workforce
- create system innovation and support community capacity
- Indigenous ownership, stewardship, design and delivery of health care services
- Budget 2023 allocated $125 million over three years to implement recommendations from MAPS.
- The next step will be to further engage with health care partners, including Indigenous communities, to implement these immediate priorities and the broader MAPS recommendations.
Related information
Alberta
Alberta’s grand bargain with Canada includes a new pipeline to Prince Rupert

From Resource Now
Alberta renews call for West Coast oil pipeline amid shifting federal, geopolitical dynamics.
Just six months ago, talk of resurrecting some version of the Northern Gateway pipeline would have been unthinkable. But with the election of Donald Trump in the U.S. and Mark Carney in Canada, it’s now thinkable.
In fact, Alberta Premier Danielle Smith seems to be making Northern Gateway 2.0 a top priority and a condition for Alberta staying within the Canadian confederation and supporting Mark Carney’s vision of making Canada an Energy superpower. Thanks to Donald Trump threatening Canadian sovereignty and its economy, there has been a noticeable zeitgeist shift in Canada. There is growing support for the idea of leveraging Canada’s natural resources and diversifying export markets to make it less vulnerable to an unpredictable southern neighbour.
“I think the world has changed dramatically since Donald Trump got elected in November,” Smith said at a keynote address Wednesday at the Global Energy Show Canada in Calgary. “I think that’s changed the national conversation.” Smith said she has been encouraged by the tack Carney has taken since being elected Prime Minister, and hopes to see real action from Ottawa in the coming months to address what Smith said is serious encumbrances to Alberta’s oil sector, including Bill C-69, an oil and gas emissions cap and a West Coast tanker oil ban. “I’m going to give him some time to work with us and I’m going to be optimistic,” Smith said. Removing the West Coast moratorium on oil tankers would be the first step needed to building a new oil pipeline line from Alberta to Prince Rupert. “We cannot build a pipeline to the west coast if there is a tanker ban,” Smith said. The next step would be getting First Nations on board. “Indigenous peoples have been shut out of the energy economy for generations, and we are now putting them at the heart of it,” Smith said.
Alberta currently produces about 4.3 million barrels of oil per day. Had the Northern Gateway, Keystone XL and Energy East pipelines been built, Alberta could now be producing and exporting an additional 2.5 million barrels of oil per day. The original Northern Gateway Pipeline — killed outright by the Justin Trudeau government — would have terminated in Kitimat. Smith is now talking about a pipeline that would terminate in Prince Rupert. This may obviate some of the concerns that Kitimat posed with oil tankers negotiating Douglas Channel, and their potential impacts on the marine environment.
One of the biggest hurdles to a pipeline to Prince Rupert may be B.C. Premier David Eby. The B.C. NDP government has a history of opposing oil pipelines with tooth and nail. Asked in a fireside chat by Peter Mansbridge how she would get around the B.C. problem, Smith confidently said: “I’ll convince David Eby.”
“I’m sensitive to the issues that were raised before,” she added. One of those concerns was emissions. But the Alberta government and oil industry has struck a grand bargain with Ottawa: pipelines for emissions abatement through carbon capture and storage.
The industry and government propose multi-billion investments in CCUS. The Pathways Alliance project alone represents an investment of $10 to $20 billion. Smith noted that there is no economic value in pumping CO2 underground. It only becomes economically viable if the tradeoff is greater production and export capacity for Alberta oil. “If you couple it with a million-barrel-per-day pipeline, well that allows you $20 billion worth of revenue year after year,” she said. “All of a sudden a $20 billion cost to have to decarbonize, it looks a lot more attractive when you have a new source of revenue.” When asked about the Prince Rupert pipeline proposal, Eby has responded that there is currently no proponent, and that it is therefore a bridge to cross when there is actually a proposal. “I think what I’ve heard Premier Eby say is that there is no project and no proponent,” Smith said. “Well, that’s my job. There will be soon. “We’re working very hard on being able to get industry players to realize this time may be different.” “We’re working on getting a proponent and route.”
At a number of sessions during the conference, Mansbridge has repeatedly asked speakers about the Alberta secession movement, and whether it might scare off investment capital. Alberta has been using the threat of secession as a threat if Ottawa does not address some of the province’s long-standing grievances. Smith said she hopes Carney takes it seriously. “I hope the prime minister doesn’t want to test it,” Smith said during a scrum with reporters. “I take it seriously. I have never seen separatist sentiment be as high as it is now. “I’ve also seen it dissipate when Ottawa addresses the concerns Alberta has.” She added that, if Carney wants a true nation-building project to fast-track, she can’t think of a better one than a new West Coast pipeline. “I can’t imagine that there will be another project on the national list that will generate as much revenue, as much GDP, as many high paying jobs as a bitumen pipeline to the coast.”
Alberta
Albertans need clarity on prime minister’s incoherent energy policy

From the Fraser Institute
By Tegan Hill
The new government under Prime Minister Mark Carney recently delivered its throne speech, which set out the government’s priorities for the coming term. Unfortunately, on energy policy, Albertans are still waiting for clarity.
Prime Minister Carney’s position on energy policy has been confusing, to say the least. On the campaign trail, he promised to keep Trudeau’s arbitrary emissions cap for the oil and gas sector, and Bill C-69 (which opponents call the “no more pipelines act”). Then, two weeks ago, he said his government will “change things at the federal level that need to be changed in order for projects to move forward,” adding he may eventually scrap both the emissions cap and Bill C-69.
His recent cabinet appointments further muddied his government’s position. On one hand, he appointed Tim Hodgson as the new minister of Energy and Natural Resources. Hodgson has called energy “Canada’s superpower” and promised to support oil and pipelines, and fix the mistrust that’s been built up over the past decade between Alberta and Ottawa. His appointment gave hope to some that Carney may have a new approach to revitalize Canada’s oil and gas sector.
On the other hand, he appointed Julie Dabrusin as the new minister of Environment and Climate Change. Dabrusin was the parliamentary secretary to the two previous environment ministers (Jonathan Wilkinson and Steven Guilbeault) who opposed several pipeline developments and were instrumental in introducing the oil and gas emissions cap, among other measures designed to restrict traditional energy development.
To confuse matters further, Guilbeault, who remains in Carney’s cabinet albeit in a diminished role, dismissed the need for additional pipeline infrastructure less than 48 hours after Carney expressed conditional support for new pipelines.
The throne speech was an opportunity to finally provide clarity to Canadians—and specifically Albertans—about the future of Canada’s energy industry. During her first meeting with Prime Minister Carney, Premier Danielle Smith outlined Alberta’s demands, which include scrapping the emissions cap, Bill C-69 and Bill C-48, which bans most oil tankers loading or unloading anywhere on British Columbia’s north coast (Smith also wants Ottawa to support an oil pipeline to B.C.’s coast). But again, the throne speech provided no clarity on any of these items. Instead, it contained vague platitudes including promises to “identify and catalyse projects of national significance” and “enable Canada to become the world’s leading energy superpower in both clean and conventional energy.”
Until the Carney government provides a clear plan to address the roadblocks facing Canada’s energy industry, private investment will remain on the sidelines, or worse, flow to other countries. Put simply, time is up. Albertans—and Canadians—need clarity. No more flip flopping and no more platitudes.
-
 Crime2 days ago
Crime2 days agoHow Chinese State-Linked Networks Replaced the Medellín Model with Global Logistics and Political Protection
-

 Addictions2 days ago
Addictions2 days agoNew RCMP program steering opioid addicted towards treatment and recovery
-

 Aristotle Foundation2 days ago
Aristotle Foundation2 days agoWe need an immigration policy that will serve all Canadians
-

 Business2 days ago
Business2 days agoNatural gas pipeline ownership spreads across 36 First Nations in B.C.
-

 Business17 hours ago
Business17 hours agoEU investigates major pornographic site over failure to protect children
-
 Courageous Discourse1 day ago
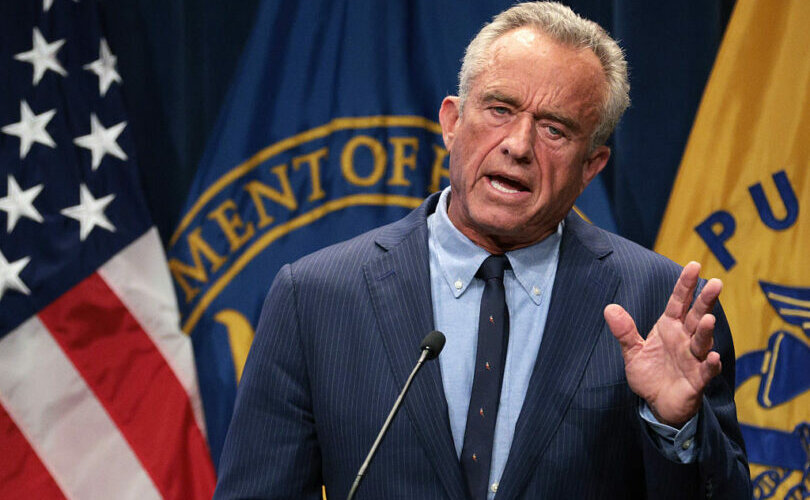
Courageous Discourse1 day agoHealthcare Blockbuster – RFK Jr removes all 17 members of CDC Vaccine Advisory Panel!
-

 Health1 day ago
Health1 day agoRFK Jr. purges CDC vaccine panel, citing decades of ‘skewed science’
-

 Censorship Industrial Complex1 day ago
Censorship Industrial Complex1 day agoConservatives slam Liberal bill to allow police to search through Canadians’ mail


