Addictions
So What ARE We Supposed To Do With the Homeless?



David Clinton
Involuntary confinement is currently enjoying serious reconsideration
Sometimes a quick look is all it takes to convince me that a particular government initiative has gone off the rails. The federal government’s recent decision to shut down their electric vehicle subsidy program does feel like a vindication of my previous claim that subsidies don’t actually increase EV sales.
But no matter how hard I look at some other programs – and no matter how awful I think they are – coming up with better alternatives of my own isn’t at all straightforward. A case in point is contemporary strategies for managing urban homeless shelters. The problem is obvious: people suffering from mental illnesses, addictions, and poverty desperately need assistance with shelter and immediate care.
The Audit is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
Ideally, shelters should provide integration with local healthcare, social, and employment infrastructure to make it easier for clients to get back on their feet. But integration isn’t cost-free. Because many shelters serve people suffering from serious mental illnesses, neighbors have to worry about being subjected to dangerous and criminal behavior.
Apparently, City of Toronto policy now requires their staff to obscure from public view the purchase and preparation of new shelter locations. The obvious logic driving the policy is the desire to avoid push back from neighbors worried about the impact such a facility could have.
As much as we might regret the not-in-my-back-yard (NIMBY) attitude the city is trying to circumvent, the neighbors do have a point. Would I want to raise my children on a block littered with used syringes and regularly visited by high-as-a-kite – and often violent – substance abusers? Would I be excited about an overnight 25 percent drop in the value of my home? To be honest, I could easily see myself fighting fiercely to prevent such a facility opening anywhere near where I live.
On the other hand, we can’t very well abandon the homeless. They need a warm place to go along with access to resources necessary for moving ahead with their lives.
One alternative to dorm-like shelters where client concentration can amplify the negative impacts of disturbed behavior is “housing first” models. The goal is to provide clients with immediate and unconditional access to their own apartments regardless of health or behaviour warnings. The thinking is that other issues can only be properly addressed from the foundation of stable housing.
Such models have been tried in many places around the world over the years. Canada’s federal government, for example, ran their Housing First program between 2009 and 2013. That was replaced in 2014 with the Homelessness Partnering Strategy which, in 2019 was followed by Reaching Home.
There have been some successes, particularly in small communities. But one look at the disaster that is San Francisco will demonstrate that the model doesn’t scale well. The sad fact is that Canada’s emergency shelters are still as common as ever: serving as many as 11,000 people a night just in Toronto. Some individuals might have benefited from the Home First-type programs, but they haven’t had a measurable impact on the problem itself.
The Audit is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
Where does the money to cover those programs come from? According to their 2023 Financial Report, the City of Toronto spent $1.1 billion on social housing, of which $504 million came in funding transfers from other levels of government. Now we probably have to be careful to distinguish between a range of programs that could be included in those “social housing” figures. But it’s probably safe to assume that they included an awful lot of funding directed at the homeless.
So money is available, but is there another way to spend it that doesn’t involve harming residential neighborhoods?
To ask the question is to answer it. Why not create homeless shelters in non-residential areas?
Right off the top I’ll acknowledge that there’s no guarantee these ideas would work and they’re certainly not perfect. But we already know that the current system isn’t ideal and there’s no indication that it’s bringing us any closer to solving the underlying problems. So why not take a step back and at least talk about alternatives?
Good government is about finding a smart balance between bad options.
Put bluntly, by “non-residential neighborhood shelters” I mean “client warehouses”. That is, constructing or converting facilities in commercial, industrial, or rural areas for dorm-like housing. Naturally, there would be medical, social, and guidance resources available on-site, and frequent shuttle services back and forth to urban hubs.
If some of this sounds suspiciously like the forced institutionalization of people suffering from dangerous mental health conditions that existing until the 1970s, that’s not an accident. The terrible abuses that existed in some of those institutions were replaced by different kinds of suffering, not to mention growing street crime. But shutting down the institutions themselves didn’t solve anything. Involuntary confinement is currently enjoying serious reconsideration.
Clients would face some isolation and inconvenience, and the risk of institutional abuses can’t be ignored. But those could be outweighed by the positives. For one thing, a larger client population makes it possible to properly separate families and healthy individuals facing short-term poverty from the mentally ill or abusive. It would also allow for more resource concentration than community-based models. That might mean dedicated law enforcement and medical staff rather than reliance on the 9-1-1 system.
It would also be possible to build positive pathways into the system, so making good progress in the rural facility could earn clients the right to move to in-town transition locations.
This won’t be the last word spoken on this topic. But we’re living with a system that’s clearly failing to properly serve both the homeless and people living around them. It would be hard to justify ignoring alternatives.
The Audit is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
Addictions
Four new studies show link between heavy cannabis use, serious health risks

Cannabis products purchased in Ontario and B.C., including gummies, pre-rolled joints, chocolates and dried flower; April 11, 2025. [Photo credit: Alexandra Keeler]
By Alexandra Keeler
New Canadian research shows a connection between heavy cannabis use and dementia, heart attacks, schizophrenia and even death
Six months ago, doctors in Boston began noticing a concerning trend: young patients were showing up in emergency rooms with atypical symptoms and being diagnosed with heart attacks.
“The link between them was that they were heavy cannabis users,” Dr. Ahmed Mahmoud, a cardiovascular researcher and physician in Boston, told Canadian Affairs in an interview.
These frontline observations mirror emerging evidence by Canadian researchers showing heavy cannabis use is associated with significant adverse health impacts, including heart attacks, schizophrenia and dementia.
Sources warn public health measures are not keeping pace with rapid changes to cannabis products as the market is commercialized.
“The irony of this moment is that society’s risk perception of cannabis is at an all-time low, at the exact moment that the substance is probably having increasingly negative health impacts,” said Dr. Daniel Myran, a physician and Canada Research Chair at the University of Ottawa. Myran was lead researcher on three new Canadian studies on cannabis’ negative health impacts.
Legalization
Canada was the first G7 country to create a commercial cannabis market when it legalized the production and sale of cannabis in 2018.
The drug is now widely used in Canada.
In the 2024 Canadian Cannabis Survey, an annual government survey of cannabis trends, 26 per cent of respondents said they used cannabis for non-medical purposes in the past year, up from 22 per cent in 2018. Among youth, that number was 41 per cent.
Health Canada’s website warns that cannabis use can lower blood pressure and raise heart rates, which can increase the risk of a heart attack. But the warnings on cannabis product labels vary. Some mention risks of anxiety or effects on memory and concentration, but make no mention of cardiovascular risks.
The annual cannabis survey also shows a significant percentage of Canadians remain unaware of cannabis’ health risks.
In the survey, only 70 per cent of respondents said they had enough reliable information to make informed decisions about cannabis use. And 50 per cent of respondents said they had not seen any education campaigns or public health messages about cannabis.
At the same time, researchers are finding mounting evidence that cannabis use is associated with health risks.
A 2023 study by researchers at the University of Calgary, the University of Alberta and Alberta Health Services found that adults with cannabis use disorder faced a 60 per cent higher risk of experiencing adverse cardiovascular events — including heart attacks. Cannabis use disorder is marked by the inability to stop using cannabis despite negative consequences, such as work, social, legal or health issues.
Between February and April of this year, three other Canadian studies linked frequent cannabis use to elevated risks of developing schizophrenia, dementia and mortality. These studies were primarily conducted by researchers at the Ottawa Hospital Research Institute and ICES uOttawa (formerly the Institute for Clinical Evaluative Sciences).
“These results suggest that individuals who require hospital-based care for a [cannabis use disorder] may be at increased risk of premature death,” said the study linking cannabis-related hospital visits with increased mortality rates.
The three 2024 studies all examined the impacts of severe cannabis use, suggesting more moderate users may face lower risks. The researchers also cautioned that their research shows a correlation between heavy cannabis use and adverse health effects, but does not establish causality.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Budtenders
Health experts say they are troubled by the widespread perception that cannabis is entirely benign.
“It has some benefits, it has some side effects,” said Mahmoud, the Boston cardiovascular researcher. “We need to raise awareness about the side effects as well as the benefits.”
Some also expressed concern that the commercialization of cannabis products in Canada has created a race to produce products with elevated levels of THC, the main psychoactive compound that produces a “high.”
THC levels have more than doubled since legalization, yet even products with high THC levels are marketed as harmless.
“The products that are on the market are evolving in ways that are concerning,” Myran said. “Higher THC products are associated with considerably more risk.”
Myran views cannabis decriminalization as a public health success, because it keeps young people out of the criminal justice system and reduces inequities faced by Indigenous and racialized groups.
“[But] I do not think that you need to create a commercial cannabis market or industry in order to achieve those public health benefits,” he said.
Since decriminalization, the provinces have taken different approaches to regulating cannabis. But even in provinces where governments control cannabis distribution, such as New Brunswick and Nova Scotia, products with high THC levels dominate retail shelves and online storefronts.
In Myran’s view, federal and provincial governments should instead be focused on curbing harmful use patterns, rather than promoting cannabis sales.
Ian Culbert, executive director of the Canadian Public Health Association, thinks governments’ financial interest in the cannabis industry creates a conflict of interest.
“[As with] all regulated substances, governments are addicted to the revenue they create,” he said. “But they also have a responsibility to safeguard the well-being of citizens.”
Culbert believes cannabis retailers should be required to educate customers about health risks — just as bartenders are required to undergo Smart Serve training and lottery corporations are required to mitigate risks of gambling addiction.
“Give ‘budtenders’ the training around potential health risks,” he said.
“While cannabis may not be the cause of some of these negative health events … it is the intersection at which an intervention can take place through the transaction of sales. So is there something we can do there that can change the trajectory of a person’s life?”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Our content is always free – but if you want to help us commission more high-quality journalism, consider getting a voluntary paid subscription.
2025 Federal Election
Study links B.C.’s drug policies to more overdoses, but researchers urge caution
By Alexandra Keeler
A study links B.C.’s safer supply and decriminalization to more opioid hospitalizations, but experts note its limitations
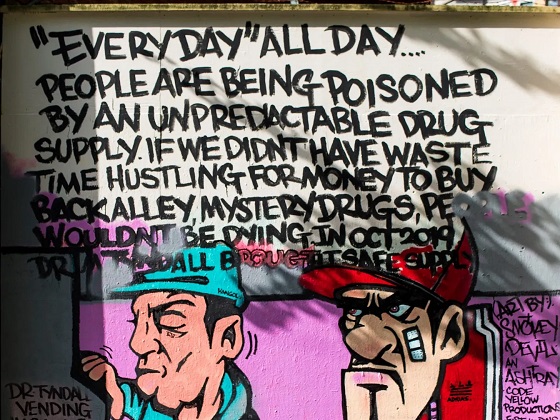
A new study says B.C.’s safer supply and decriminalization policies may have failed to reduce overdoses. Furthermore, the very policies designed to help drug users may have actually increased hospitalizations.
“Neither the safer opioid supply policy nor the decriminalization of drug possession appeared to mitigate the opioid crisis, and both were associated with an increase in opioid overdose hospitalizations,” the study says.
The study has sparked debate, with some pointing to it as proof that B.C.’s drug policies failed. Others have questioned the study’s methodology and conclusions.
“The question we want to know the answer to [but cannot] is how many opioid hospitalizations would have occurred had the policy not have been implemented,” said Michael Wallace, a biostatistician and associate professor at the University of Waterloo.
“We can never come up with truly definitive conclusions in cases such as this, no matter what data we have, short of being able to magically duplicate B.C.”
Jumping to conclusions
B.C.’s controversial safer supply policies provide drug users with prescription opioids as an alternative to toxic street drugs. Its decriminalization policy permitted drug users to possess otherwise illegal substances for personal use.
The peer-reviewed study was led by health economist Hai Nguyen and conducted by researchers from Memorial University in Newfoundland, the University of Manitoba and Weill Cornell Medicine, a medical school in New York City. It was published in the medical journal JAMA Health Forum on March 21.
The researchers used a statistical method to create a “synthetic” comparison group, since there is no ideal control group. The researchers then compared B.C. to other provinces to assess the impact of certain drug policies.
Examining data from 2016 to 2023, the study links B.C.’s safer supply policies to a 33 per cent rise in opioid hospitalizations.
The study says the province’s decriminalization policies further drove up hospitalizations by 58 per cent.
“Neither the safer supply policy nor the subsequent decriminalization of drug possession appeared to alleviate the opioid crisis,” the study concludes. “Instead, both were associated with an increase in opioid overdose hospitalizations.”
The B.C. government rolled back decriminalization in April 2024 in response to widespread concerns over public drug use. This February, the province also officially acknowledged that diversion of safer supply drugs does occur.
The study did not conclusively determine whether the increase in hospital visits was due to diverted safer supply opioids, the toxic illicit supply, or other factors.
“There was insufficient evidence to conclusively attribute an increase in opioid overdose deaths to these policy changes,” the study says.
Nguyen’s team had published an earlier, 2024 study in JAMA Internal Medicine that also linked safer supply to increased hospitalizations. However, it failed to control for key confounders such as employment rates and naloxone access. Their 2025 study better accounts for these variables using the synthetic comparison group method.
The study’s authors did not respond to Canadian Affairs’ requests for comment.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Correlation vs. causation
Chris Perlman, a health data and addiction expert at the University of Waterloo, says more studies are needed.
He believes the findings are weak, as they show correlation but not causation.
“The study provides a small signal that the rates of hospitalization have changed, but I wouldn’t conclude that it can be solely attributed to the safer supply and decrim[inalization] policy decisions,” said Perlman.
He also noted the rise in hospitalizations doesn’t necessarily mean more overdoses. Rather, more people may be reaching hospitals in time for treatment.
“Given that the [overdose] rate may have gone down, I wonder if we’re simply seeing an effect where more persons survive an overdose and actually receive treatment in hospital where they would have died in the pre-policy time period,” he said.
The Nguyen study acknowledges this possibility.
“The observed increase in opioid hospitalizations, without a corresponding increase in opioid deaths, may reflect greater willingness to seek medical assistance because decriminalization could reduce the stigma associated with drug use,” it says.
“However, it is also possible that reduced stigma and removal of criminal penalties facilitated the diversion of safer opioids, contributing to increased hospitalizations.”
Karen Urbanoski, an associate professor in the Public Health and Social Policy department at the University of Victoria, is more critical.
“The [study’s] findings do not warrant the conclusion that these policies are causally associated with increased hospitalization or overdose,” said Urbanoski, who also holds the Canada Research Chair in Substance Use, Addictions and Health Services.
Her team published a study in November 2023 that measured safer supply’s impact on mortality and acute care visits. It found safer supply opioids did reduce overdose deaths.
Critics, however, raised concerns that her study misrepresented its underlying data and showed no statistically significant reduction in deaths after accounting for confounding factors.
The Nguyen study differs from Urbanoski’s. While Urbanoski’s team focused on individual-level outcomes, the Nguyen study analyzed broader, population-level effects, including diversion.
Wallace, the biostatistician, agrees more individual-level data could strengthen analysis, but does not believe it undermines the study’s conclusions. Wallace thinks the researchers did their best with the available data they had.
“We do not have a ‘copy’ of B.C. where the policies weren’t implemented to compare with,” said Wallace.
B.C.’s overdose rate of 775 per 100,000 is well above the national average of 533.
Elenore Sturko, a Conservative MLA for Surrey-Cloverdale, has been a vocal critic of B.C.’s decriminalization and safer supply policies.
“If the government doesn’t want to believe this study, well then I invite them to do a similar study,” she told reporters on March 27.
“Show us the evidence that they have failed to show us since 2020,” she added, referring to the year B.C. implemented safer supply.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Our content is always free – but if you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
-

 Alberta15 hours ago
Alberta15 hours agoPremier Danielle Smith responds to election of Liberal government
-

 International2 days ago
International2 days agoU.S. Army names new long-range hypersonic weapon ‘Dark Eagle’
-

 Business2 days ago
Business2 days agoOttawa’s Plastics Registry A Waste Of Time And Money
-

 Business2 days ago
Business2 days agoNet Zero by 2050: There is no realistic path to affordable and reliable electricity
-

 Addictions2 days ago
Addictions2 days agoFour new studies show link between heavy cannabis use, serious health risks
-
 Business2 days ago
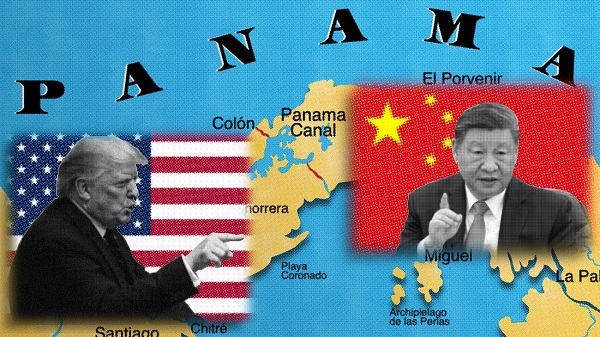
Business2 days agoTrump demands free passage for American ships through Panama, Suez
-

 COVID-192 days ago
COVID-192 days agoFormer Australian state premier accused of lying about justification for COVID lockdowns
-

 Also Interesting2 days ago
Also Interesting2 days agoTop Used Ford SUVs for Families and Adventurers