Health
Robert F. Kennedy, Jr. Urges ‘Make America Healthy Again’

From Heartland Daily News
Despite dropping out of the race for president in August, Robert F. Kennedy, Jr. is turning up the volume on reforming national health care and drug policy and attracting attention to what role he might play in an administration depending on the outcome of the November election.
Kennedy has endorsed former president Donald Trump, and Trump has hinted that there could be a role in his second Trump administration.
Kennedy, who founded the safety advocacy group Children’s Health Defense, recently revealed the scope of his health care recommendations through his “Make America Healthy Again” agenda. Trump named Kennedy to his transition team and pledged to establish a panel of experts to work with Kennedy to investigate the increase of chronic health problems and childhood diseases in the United States (see related articles, pages 8,9).
In a September 5 op-ed in The Wall Street Journal, Kennedy laid out his 12-point Make America Healthy Again plan. Some of the ideas include reducing conflicts of interest at federal health agencies, implementing drug price caps, setting chemical and pesticide standards, requiring nutrition classes in medical school, redirecting money toward preventative care, rereleasing a presidential fitness standard, and expanding health savings accounts.
Boundary Crossing
Over the years, Kennedy has not hesitated to express his opinions, many of which have challenged long-held positions of the public health establishment on issues from vaccines and childhood obesity to the role of big pharmaceutical companies.
Kennedy’s stances cross ideological boundaries. His support of a single-payer national health care system conflicts with free-market opinions on the right, and his criticism of big-government bullying alienates the left. The nation’s painful experience with the measures taken to stem the spread of COVID-19 has attracted attention to Kennedy’s health care opinions in the wake of his forceful criticisms of those policies.
In a wide-ranging interview with Preferred Health magazine in June, Kennedy lambasted the lockdowns and the people he says profited from them.
“The people who came into the pandemic with a billion dollars, the Bill Gates, the Mark Zuckerbergs, the Bloombergs, the Jeffery Bezos, increased their wealth on average by 30 percent,” Kennedy told the publication.
“The lockdowns were a gift to them, the super-rich,” said Kennedy. “Jeffery Bezos, the richest or second-richest man in the world, was able to close down all of his competitors, 3.3 million businesses, and then give us a two-year training course about how to never use a retail outlet again in our lives. Forty-one percent of the black-owned businesses will never reopen. And he was instrumental because he was censoring the books that were critical of the lockdowns, including one that I wrote.”
Insider Advantage
Kennedy’s criticisms appeal to Craig Rucker, president of the Committee for a Constructive Tomorrow (CFACT).
“Kennedy, by virtue of his family name, is an insider, but his unorthodox views make him a provocative outsider,” said Rucker. “The public-health establishment, against which he has railed for years, failed miserably during the coronavirus pandemic. The ties between HHS and Big Pharma are far too cozy, and we have good reason to believe public health suffers as a consequence. A free spirit like his could be just what the doctor ordered.”
NIH Reform Call
Echoing his criticisms of the pandemic response, Kennedy says he wants to overhaul federal health care agencies, beginning with the National Institutes of Health (NIH).
The NIH suppressed the use of ivermectin and hydroxychloroquine during the early stages of the pandemic, in favor of, first, remdesivir and later the COVID vaccines through emergency use authorization, Kennedy argues. Saying the NIH “has been transformed into an incubator for the pharmaceutical industry,” Kennedy recommends removing much of the NIH’s funding for virology.
“It has stepped away from rigorous, evidence-based science, evidence-based medicine, into kind of a magical world,” Kennedy told Preferred Health. “It needs to have scientific discipline reimposed on the entire field of virology. We ought to be funding the study of the etiology of chronic diseases in our universities.”
Focus Shift
Kennedy has also spoken widely on chronic childhood diseases, some of which he has attributed to vaccines. Kennedy has called for public health authorities to shift their focus from infectious diseases such as COVID and influenza to devote more attention to diabetes, obesity, environmental toxins, and other longer-term concerns.
Kennedy has also cited large-scale factory farming and processed food as contributing to the nation’s health problems.
Peter Pitts, president and co-founder of the Center for Medicine in the Public Interest, says Kennedy brings a fresh perspective to public health debates.
“RFK Jr.’s penchant for not taking things at face value could go a long way toward forcing government public-health agencies to argue on behalf of their beliefs rather than simply relying on a ‘because I said so’ defense,” said Pitts.
Surprising Endorsements
Texas Agriculture Commissioner Sid Miller, a Republican, praised Kennedy’s efforts in a September 26 op-ed for Fox News.
“The role of Big Food, much like Big Pharma, is to prioritize their profits over our health,” wrote Miller. “I enthusiastically support RFK Jr.’s campaign to hold these industries accountable by reforming our food and medicine approval and patenting systems. In this he is uniquely qualified: the $1.7 trillion pharmaceutical industry has unfairly maligned him for decades, and he’s still standing strong.”
In a move that raised eyebrows, Robert Redfield, who headed the Centers for Disease Control and Prevention (CDC) under Trump from 2018 to 2021, endorsed Kennedy’s reform efforts in a Newsweek op-ed in September.
“If the next president prioritizes the National Institutes of Health (NIH) to identify which exposures are contributing to the spike in chronic disease in children, we will finally find out and end what is slowly destroying our children,” wrote Redfield.
Bonner Russell Cohen, Ph.D., ([email protected]) is a senior fellow at the National Center for Public Policy Research.
Health
Lack of adequate health care pushing Canadians toward assisted suicide

From LifeSiteNews
The family of an elderly man is speaking out about the terrible hospital conditions that led their father to request euthanasia before he died of natural causes.
The family of Cleo Gratton, an 84-year-old retired diamond driller who died earlier this month in Chelmsford, Ontario, of natural causes after being approved for assisted suicide, is speaking publicly about their appalling experience in the Canadian healthcare system.
According to the CBC, the elderly man “told his family he would rather die than go back to Health Sciences North in Sudbury,” and that a recent stay there found Gratton, who was suffering from heart disease and kidney failure, spending one night in the emergency room and then being transferred to a bed sitting in the hallway on the seventh floor.
“There were no lights, all the bulbs in that hallway had been completely removed,” his daughter, Lynn, told the CBC. “The only light we had was almost like a desk lamp that had been bolted to the wall. Patients are passing by, nurses are going by, no privacy, no compassion, no dignity.” The visit took place in mid-October, after which Gratton decided to apply for “medical aid in dying,” or assisted suicide.
Lynn said that nurses had to use headlamps to inspect her father’s feet, and that the experience was “just one thing after another and it really opened our eyes to what’s going on in our hospitals. My dad said, ‘Push, push, push for change. Make people aware of what’s gong on. Open the discussion, bring it to your MP, your MPP, keep going straight up.”
His family is now honoring his wishes to speak out about his experience. The doctors and nurses, Lynn emphasized, were “amazing,” but she noted that they seem overworked. “Why are they still taking in patients if we have an overcrowding issue and they have no place to put these people?” she said.
Cleo Gratton, who died of natural causes surrounded by his family before he could go through with assisted suicide, is just the most recent of many examples of Canadians opting for assisted suicide because they could not access the care that they actually desired.
In Quebec last year, Norman Meunier, a quadriplegic man, developed bedsores after four days left on an ER stretcher without a good mattress. That experience combined with lack of available homecare pushed him to request, and receive, assisted suicide.
An unnamed woman in her 80s, referred to in a MAID report as “Mrs. B,” received MAID earlier this year after requesting but being denied palliative or hospice care. Instead, with her spouse burning out as the result of her care, a rushed MAID assessment was completed, and she died by lethal injection.
In 2022, 44-year-old Winnipeg woman Sathya Dhara Khovac died by euthanasia after failing to receive the homecare resources she had desperately sought. In her posthumous obituary, she said she could have had more time if she’d had more help.
In 2019, 41-year-old Sean Tagert was euthanized after spending years attempting to find and fund the homecare and resources he needed to stay in the community where his son lived. He did not want to die but felt that he had no other choice.
And, among other stories, at least four Canadian veterans were offered assisted suicide in lieu of the unavailable mental health supports they were requesting.
Stories of Canadians seeking palliative care, mental health resources, homecare, and other medical support finding that the only option available to them is assisted suicide have become routine over the past several years. Euthanasia has become a pressure valve for an overworked and under-funded healthcare system serving an aging population increasingly need of complex care — and if assisted suicide for mental illness is legalize, things will get much, much worse.
Dr John Campbell
Cures for Cancer? A new study shows incredible results from cheap generic drug Fenbendazole

From Dr. John Campbell
You won’t hear much about Fenbendazole from the regular pipeline of medical information. There could be many reasons for that. For one, it’s primarily known for it’s use in veterinary medicine. Somehow during COVID the medical information pipeline convinced millions that if a drug is used on horses or other animals it couldn’t work for humans. Not sure how they got away with that one considering the use of animal trials for much of modern medical history.
Another possible reason, one that makes at least as much sense, is that there’s no business case for Fenbendazole. It’s been around for decades and its patent expired in the early 1990’s. That means it’s considered a generic drug that a pharmaceutical company from India could (and does) produce in mass quantities for very little profit (compared to non-generics).
So Fenbendazole is an inexpensive, widely accessible antiparasitic drug used in veterinary medicine. During the COVID pandemic a number of doctors, desperate for a suitable treatment, tried it with reportedly great levels of success. Over some time they discovered it might be useful elsewhere. Some doctors are using Fenbendazole to help treat late stage cancer. Often this is prescribed when the regular treatments clearly aren’t working and cancer is approaching or has already been declared stage 4.
What they’ve found at least in some cases is astounding results. This has resulted in a new study which medical researcher Dr. John Campbell shares in this video.
-

 Crime1 day ago
Crime1 day agoCBSA Bust Uncovers Mexican Cartel Network in Montreal High-Rise, Moving Hundreds Across Canada-U.S. Border
-

 Environment1 day ago
Environment1 day agoThe Myths We’re Told About Climate Change | Michael Shellenberger
-

 Dr John Campbell2 days ago
Dr John Campbell2 days agoCures for Cancer? A new study shows incredible results from cheap generic drug Fenbendazole
-

 Artificial Intelligence1 day ago
Artificial Intelligence1 day agoAI Faces Energy Problem With Only One Solution, Oil and Gas
-

 Health1 day ago
Health1 day agoLack of adequate health care pushing Canadians toward assisted suicide
-
 Alberta1 day ago
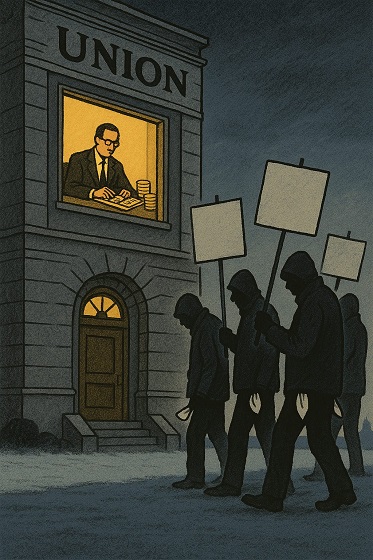
Alberta1 day agoATA Collect $72 Million in Dues But Couldn’t Pay Striking Teachers a Dime
-
 Media1 day ago
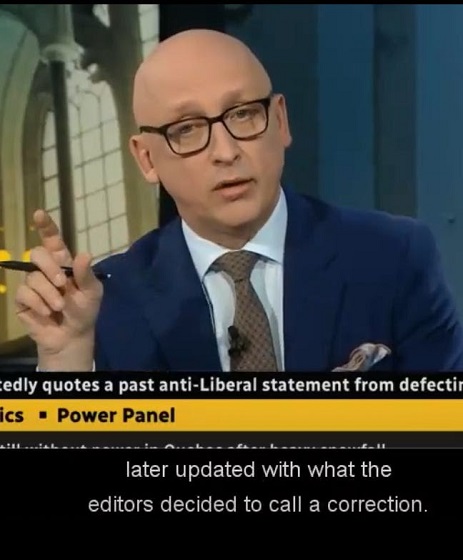
Media1 day agoBreaking News: the public actually expects journalists to determine the truth of statements they report
-

 Artificial Intelligence1 day ago
Artificial Intelligence1 day agoAI seems fairly impressed by Pierre Poilievre’s ability to communicate








