Addictions
Province provides 3.4 million to transition Red Deer away from drug consumption site

In Red Deer, Alberta’s government is increasing access to recovery-oriented care by launching several new initiatives within the community.
Alberta’s government has built a system of care based on the belief that recovery is possible for those suffering from the disease of addiction. The focus has been on reducing barriers to recovery by increasing capacity and ensuring that no one is forced to pay for life-saving addiction treatment. Since 2019, the province has added more than 10,000 new addiction treatment spaces. It has also removed financial barriers and pioneered a program for immediate, same-day access to life-saving evidence-based treatment medication.
Red Deer is home to Alberta’s first of 11 recovery communities being built by the province. This facility opened its doors in May 2023 and has become a beacon of hope for those suffering from addiction, along with their families. Red Deer was also the first in Alberta to open a Therapeutic Living Unit within its correctional center. This means the recovery community model of treatment has been adopted in corrections, lowering the chances of reoffending and breaking the cycle of addiction and crime in individuals’ lives. Access to opioid agonist therapy has been expanded to police cells through the Virtual Opioid Dependency Program and can also be administered by specialized paramedics with support from the province.
Earlier this year, Red Deer city council put forward and passed a motion requesting a transition of the drug consumption site to instead implement options focused on health, wellness and recovery.
In response to this request, Alberta’s government has committed $3.4 million to provide the following:
- A Mobile Rapid Access Addiction Medicine clinic operated by Recovery Alberta, located in the homeless shelter parking lot. This will offer screening, diagnosis and referral to services; access to the Virtual Opioid Dependency Program; and education, naloxone kits and needle exchange.
- A Dynamic Overdose Response Team of paramedics and licensed practical nurses to monitor a designated area of the Safe Harbour shelter facility, as well as the surrounding block.
- Recovery coaches in and around the homeless shelter to provide outreach services and help guide individuals along the path of recovery.
- Enhancements to medically supported detox capacity in partnership with Safe Harbour that will help more people safely withdraw from substances so they can continue their pursuit of recovery.
In addition, Alberta’s government recently provided more than $1.2 million over the next two years to the Red Deer Dream Centre to support 20 additional publicly funded addiction treatment beds.
“Our government will always listen to and take seriously the feedback we receive from elected local leaders. This is a well-thought-out plan that aligns with Red Deer’s needs and requests, which is why the province is making these changes and increasing support for the community. We remain committed to protecting the health and well-being of Albertans while actively supporting connections to treatment and recovery.”
“Our council is pleased to see this new path forward for recovery-oriented services in Red Deer. At the heart of our council’s and community’s efforts is the belief that recovery is possible for everyone, especially the most vulnerable. This is a complex challenge and only by working with all our partners at the province, agencies, businesses, faith communities and all Red Deerians will we create a safe, healthy and prosperous community. We look forward to close collaboration with the province as these changes are made.”
Alberta’s government is working closely with the City of Red Deer, Safe Harbour Society, Recovery Alberta and others to implement these supports starting this fall.
Since October 2018, the Red Deer drug consumption site has been operating at a temporary site within an ATCO trailer in the parking lot next to Safe Harbour Society’s detox building. As requested by the city council, the drug consumption site will be transitioned out of Red Deer once all other services are operational, which is anticipated to be in spring 2025. The program expansion for recovery services represents a net increase in programming and staffing.
“We look forward to bringing a new service to Red Deer with the opening of a Mobile Rapid Access Addiction Medicine clinic. With this and the new outreach services being put in place, Recovery Alberta will provide opportunities for those facing addiction and mental health issues to access support on an ongoing basis.”
“I am pleased to see that Alberta’s government is working collaboratively with our local government and service providers. This plan ensures we prioritize Red Deer’s needs while also supporting individuals in their pursuit of recovery.”
“Red Deer is a beautiful community with wonderful families and individuals. Transitioning the drug site out of Red Deer and focusing on recovery is the right thing to do. Thank you to the Government of Alberta and Red Deer City Council for leading, listening and doing what is right.”
“We are pleased to partner with Alberta’s government, Recovery Alberta and the City of Red Deer to increase access to addiction and detox services for those accessing supports at Safe Harbour. This partnership profoundly enhances our capacity to meet the needs of community members challenged by addiction and to support them in their recovery journey.”
Alberta is making record investments and removing barriers to recovery-oriented supports for all Albertans, regardless of where they live or their financial situation. This includes the addition of more than 10,000 new publicly funded addiction treatment spaces, expanded access to the Virtual Opioid Dependency Program—which provides same-day access to life-saving treatment medication—the removal of daily user fees for publicly funded live-in treatment, and the construction of 11 world-class recovery communities.
Quick facts
- Albertans struggling with opioid addiction can contact the Virtual Opioid Dependency Program (VODP) by calling 1-844-383-7688, seven days a week, from 6 a.m. to midnight. VODP provides same-day access to addiction medicine specialists. There is no wait list.
Related information
Related news
Addictions
Manitoba Is Doubling Down On A Failed Drug Policy

From the Frontier Centre for Public Policy
Manitoba is choosing to expand the same drug policy model that other provinces are abandoning, policies that normalize addiction while sidelining treatment, recovery, and public safety.
The New Democrat premier of British Columbia, David Eby, stood before reporters last spring and called his government’s decision to permit public drug use in certain spaces a failure.
The policy was part of the broader “harm reduction” strategy meant to address overdose deaths. Instead, it had stirred public anger, increased street disorder and had helped neither users nor the communities that host them. “We do not accept street disorder that makes communities feel unsafe,” Eby said. The province scrapped the plan.
In Alberta, the Conservative government began shutting down safer-supply prescribing due to concerns about drug diversion and misuse. The belief that more opioids can resolve the opioid crisis is losing credibility.
Ontario Progressive Conservatives are moving away from harm reduction by shutting down supervised consumption sites near schools and limiting safer-supply prescribing. Federal funding for programs is decreasing, and the province is shifting its focus to treatment models, even though not all sites are yet closed.
Yet amid these non-partisan reversals, Manitoba’s government has announced its intention to open a supervised drug-use site in Winnipeg. Premier Wab Kinew said, “We have too many Manitobans dying from overdose.” True. But it does not follow that repeating failed approaches will yield different results.
Reversing these failed policies is not a rejection of compassion. It is a recognition that good intentions do not produce good outcomes. Vancouver and Toronto have hosted supervised drug-use sites for years. The death toll keeps rising. Drug deaths in British Columbia topped 2,500 in 2023, even with the most expansive harm reduction infrastructure in the country. A peer-reviewed study published this year found that hospitalizations from opioid poisoning rose after B.C.’s safer-supply policy was implemented. Emergency department visits increased by more than three cases per 100,000 population, with no corresponding drop in fatal overdoses.
And the problem persists day to day. Paramedics in B.C. responded to nearly 4,000 overdose calls in July 2024 alone. The monthly call volume has exceeded 3,000 almost every month this year. These are signs of crisis management without a path to recovery.
There are consequences beyond public health. These policies change the character of neighbourhoods. Businesses suffer. Residents feel unsafe. And most tragically, the person using drugs is offered little more than a cot, a nurse and a quiet signal to continue. Real help, like treatment, housing and purpose, remains out of reach.
Somewhere along the way, bureaucracies stopped asking what recovery looks like. They have settled for managing human decline. They call it compassion. But it is really surrender, wrapped in medical language.
Harm reduction had its time. It made sense when it first emerged, during the AIDS crisis, when dirty needles spread HIV. Back then, the goal was to stop a deadly virus. Today, that purpose has been lost.
When policy drifts into ideology, reality becomes an afterthought. Underneath today’s approach is the belief that drug use is inevitable, that people cannot change, that liberty means letting others fade away quietly. These ideas do not reflect science. They do not reflect hope. They reflect despair. They reflect a politics that prioritizes the appearance of compassion over effectiveness.
What Manitoba needs is treatment access that meets the scale of the problem. That means detox beds, recovery homes and long-term care focused on restoring lives. These may not generate the desired headlines, but they work. They are demanding. They are slow. And they offer respect to the person behind the addiction.
There are no shortcuts. No policy will undo decades of pain overnight. But a policy that keeps people stuck using is not mercy. It is maintenance with no way out.
A government that believes in its people should not copy failure.
Marco Navarro-Genie is vice-president of research at the Frontier Centre for Public Policy and co-author, with Barry Cooper, of Canada’s COVID: The Story of a Pandemic Moral Panic (2023).
Addictions
The Death We Manage, the Life We Forget

 Marco Navarro-Génie
Marco Navarro-Génie
Our culture has lost the plot about what it means to live.
Reading that Manitoba is bringing supervised consumption to Winnipeg got me thinking.
Walk through just about any major Canadian city, and you will see them. Figures bent forward at seemingly impossible angles, swaying in the characteristic “fentanyl fold,” suspended between consciousness and oblivion. They resemble the zombies of fiction: bodies that move through space without agency, awareness, or connection to the world around them. We think of zombies as the walking dead. Health workers and bureaucrats reverse their overdoses, send them back to the street, and call it saving lives.
At the same time, Canada offers medical assistance in dying to a woman who cited chemical sensitivities and the inability to find housing. It has been offered to veterans who asked for support and were met instead with an option for death. We fight to prevent one form of death while facilitating another. The contradiction is not accidental. It reveals something about the people involved and the funding behind it. That’s our culture. Us. It appears to me that our culture no longer knows what life is.
Ask any politician or program bureaucrat, and you will hear them explain, in the dry language of bureaucracy, that the twin approach to what they call harm reduction and medical assistance in dying (MAiD) rests on the shared premise of what they believe to be compassion. They think they respect autonomy, prevent suffering, and keep people alive when possible. It sounds humane. It is, in practice, incoherent. Bear with me for a moment.
The medical establishment administers naloxone to reverse overdoses in people who spend as many as twenty hours a day unconscious. They live without meaningful relationships or memories, with little capacity for choice. The technocrats and politicians call that saving lives. They also provide assisted death to people whose suffering comes primarily from poverty, isolation, or lack of housing. There was a time when these factors could, at least in theory, be addressed so that the terminal decision did not need to be made. Now they are accepted as grounds for ending life.
But why is one preference final and the other treated as an error to correct? That question reflects the deeper disorientation.
We saw the same thing during COVID. Elderly people in care homes were left without touch, family, or comfort for days. They often died in solitude, their dementia accelerated by isolation. And those conditions were inflicted upon them in the name of saving their lives. The “system” measured success in preventing infections, not in preserving connections. Je me souviens. Or we should.
There is a pattern here. We have reduced the idea of saving lives to keeping bodies breathing, while ignoring what makes a life human: agency, meaning, development, and relationship. And in doing so, we begin to define life as mere biological persistence. But to define life by the capacity to breathe and perform basic functions is to place ourselves on the same footing as the non-human animals. It is to say, tacitly, that there is no fundamental distinction between a person and a creature. That, too, is a form of forgetting.
To be clear, the argument here is not that hopeless drug users should be administered MAiD. Instead, it is essential to recognize that the intellectual framework behind harm reduction and MAiD must be taken seriously, as it rests on some rationally defensible claims. In an age where most arguments are emotive and unexamined, the mildly logical has become strangely compelling.
It begins with the idea of autonomy. We cannot force others to live by our values. Every person must decide what makes life worth living. To insist otherwise is paternalism.
Then comes pragmatic compassion. People will use drugs whether we approve or not. People will find their lives unbearable, whether we acknowledge it or not. We can support them or moralize while they die.
There is also an emphasis on subjective experience. No one knows another’s pain. If someone says their suffering is intolerable, we are in no position to deny it, they say. If a user would rather face opioids than withdrawal and despair, are we entitled to interfere?
Finally, the comparison to medical ethics: we do not withhold insulin from diabetics who continue to eat poorly. We do not deny cancer treatment to smokers. Medicine responds to suffering, even when the patient has contributed to their condition. Harm reduction, they argue, simply applies that principle to addiction.
These arguments produced tangible benefits, they argue. Needle exchanges reduced HIV transmission. Naloxone kits prevented deaths. Safe injection sites meant fewer people dying alone. MAiD brought relief to those in agony. These were not trivial outcomes. I am aware.
Yet when we look more closely, the very logic that underlies these policies also exposes their fatal limitations.
Addiction undermines choice. It hijacks the brain’s ability to reason, compare, and choose. A person deep in addiction is not selecting between alternatives like someone choosing coffee or tea. The structure of choice, the human will, itself is broken. The addiction decides before the person does. St Augustine knew this. Dostoyevsky knew it too.
And for the empirically minded, the research supports this. In British Columbia, where the “safe supply” model was pioneered, some addiction physicians now say the policy is failing. Worse, it may be creating new opioid dependencies in people who were not previously addicted. A study earlier this year found that opioid‑related hospitalizations increased by about 33 percent, compared with pre‑policy rates. With the later addition of a drug-possession decriminalization policy, hospitalizations rose even more (overall, a 58 percent increase compared to before SOS’s implementation). The study concluded that neither safer supply nor decriminalization was associated with a statistically significant reduction in overdose deaths. This is not freedom. It is a new form of bondage, meticulously paved by official compassion.
Despair disguises itself as autonomy, especially in a spiritually unmoored culture that no longer knows how to cope with suffering. A person requesting assisted death because of chronic, untreatable pain may appear lucid and composed, but lucidity is not the same as wisdom. One can reason clearly from false premises. If life is reduced to the absence of pain and the preservation of comfort, then the presence of suffering will seem like failure, and death will appear rational. But that is not a genuine choice because it is based on a misapprehension of what life is. All life entails pain. Some of it is redemptive. Some of it is endured. But it does not follow that the presence of suffering justifies the conclusion of life.
Someone turning to drugs because of homelessness, abandonment, or despair is often in an even deeper eclipse of the will. Here, there is not even the appearance of deliberation, only the reach for numbness in the absence of meaning. What looks like a decision is the residue of collapse. We are not witnessing two forms of autonomy, one clearer than the other. We are witnessing the breakdown of autonomy in various forms, and pretending that it is freedom.
Biological survival is not life. When we maintain someone in a state of near-constant unconsciousness, with no relationships, no capacity for flourishing, we are not preserving life. We are preserving a body. The person may already be gone. To define life as nothing more than breathing and performing bodily functions is to deny what makes us human. It reduces us to the level of non-human creatures, sentient, perhaps, but without reason, memory, moral reflection, or the possibility of transcendence. It tacitly advances the view that there is no essential difference between a person and a critter, so long as both breathe and respond to some stimuli.
Governments do these things to keep ballooning overdosing deaths down, preferring to maintain drugs users among the undead instead. That reminds me of how the Mexican government hardly moves a finger to find the disappeared, 100,000 strong of lately. For as long ss they’re disappeared, they choose not to count them as homicides, and they feel justified in ignoring the causes of all the killing around them.
Some choices are nefarious. Some choices deserve challenge. Not all autonomous acts are equal. The decision to continue living with pain, or to fight addiction, requires agency. The decision to surrender to despair may signal the absence of it. To say all choices are equal is to empty the word autonomy of meaning.
This reflects a dangerously thin view of the human person that permeates our present. What we now call “harm” is only death or physical pain. What we call good is whatever someone prefers. But people are more than collections of wants.
We should have learned this by now. In Alberta, safer supply prescribing was effectively banned in 2022. Officials cited diversion and lack of measurable improvement. We are forcing some people into treatment because we recognize the impairment of judgement in addiction.
In British Columbia, public drug use was quietly re-criminalized after communities rebelled. This was an admission of policy failure. “Keeping people safe is our highest priority,” Premier David Eby said. Yet safe supply remains. In 2023, the province recorded more than 2,500 overdose deaths. Paramedics continue to respond to thousands of overdose calls each month. This is not success. It is a managed collapse.
Meanwhile, Manitoba is preparing to open its own supervised drug-use site. Premier Wab Kinew said, “We have too many Manitobans dying from overdose… so this is one tool we can use.” That may be so. However, it is a tool that others are beginning to set aside. It is a largely discredited tool. Sadly, in the self-professed age of “Reconciliation” with Aboriginal Canadians, Aboricompassionadians are disproportionately affected by these discredited policies.
The Manitoba example illustrates the broader problem, despite damning evidence. Instead of asking what helps people live, we ask whether they gave consent. We do not ask whether they were capable of it. We ask whether they avoided death. We do not ask whether they found purpose.
We are not asking what might lead someone out of addiction. We are not asking what they need to flourish. We ask only what we can do to prevent them from dying in the short term. And when that becomes impossible, technocracy offers them death in a more organized form, cleanly approved by government. That’s compasson.
The deeper problem is not policy incoherence. It is the cultural despair that skates on the thin ice of meaninglessness. These policies make sense only in a culture that has already decided life is not worth too much. What matters is state endorsement and how it’s done .
It is more cost-effective to distribute naloxone than to construct long-term recovery homes. It is easier to train nurses to supervise injection than to provide months of residential treatment. It is far simpler to legalize euthanasia for the poor and the suffering than to work on solutions that lift them out of both. But is it right?
This is not compassion. It is surrender.
A humane policy would aim to restore agency, not validate its absence. It would seek out what helps people grow in wisdom and self-command, not what leaves them comfortably sedated. It would measure success not in lives prolonged into darker dependency but in persons recovered. In lives better lived.
This vision is harder. It costs time. It requires greater effort. It requires care and what some Christians call love of neighbour. It may require saying no when someone asks for help that could lead to ruin. But anything less is not mercy. It is a slow walk toward death while we leave the “system” to pretend there is no choice.
We did have a choice. We chose shallow comfort over deep obligation. We chose to manage symptoms rather than confront the deeper conditions of our age: loneliness, meaninglessness, despair. And now we live among the results: more, not fewer, people swaying in silence, already gone walking dead.
We might ask what we’ve forgotten about suffering, about responsibility, about what life is. Lives are at stake. True. But when our understanding of life is misdirected, so will be the policies the state gives us.
We are grateful that you’re reading Haultain Research.
For the full experience, and to help us bring you more quality research and commentary,
-

 Automotive13 hours ago
Automotive13 hours agoPoliticians should be honest about environmental pros and cons of electric vehicles
-

 Agriculture2 days ago
Agriculture2 days agoWhy is Canada paying for dairy ‘losses’ during a boom?
-

 Business2 days ago
Business2 days agoCanada Hits the Brakes on Population
-

 Daily Caller2 days ago
Daily Caller2 days ago‘Almost Sounds Made Up’: Jeffrey Epstein Was Bill Clinton Plus-One At Moroccan King’s Wedding, Per Report
-
 Crime2 days ago
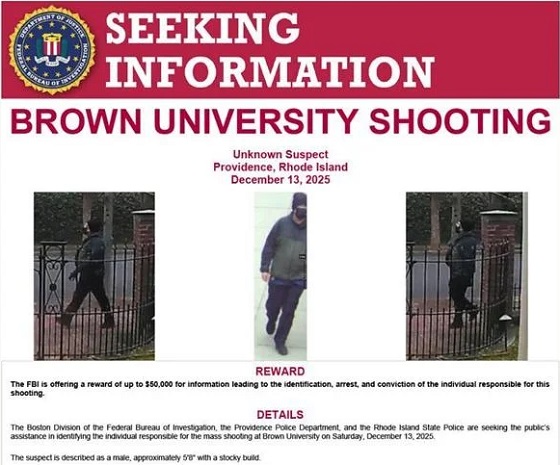
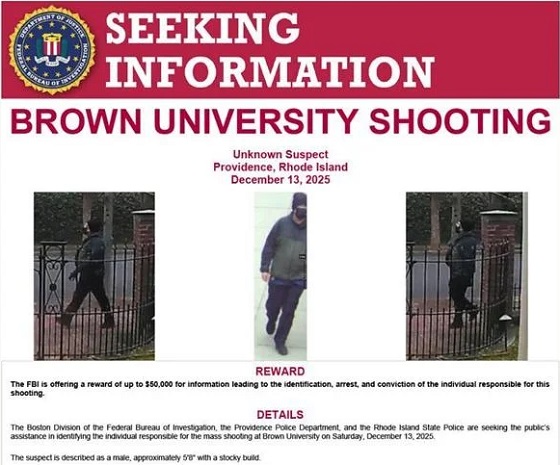
Crime2 days agoBrown University shooter dead of apparent self-inflicted gunshot wound
-

 Business2 days ago
Business2 days agoTrump signs order reclassifying marijuana as Schedule III drug
-

 Bruce Dowbiggin24 hours ago
Bruce Dowbiggin24 hours agoHunting Poilievre Covers For Upcoming Demographic Collapse After Boomers
-

 Alberta1 day ago
Alberta1 day agoAlberta’s new diagnostic policy appears to meet standard for Canada Health Act compliance






