Health
Pierre Poilievre praises MP for speaking out against euthanasia for mentally ill

From LifeSiteNews
MP Andrew Lawton, who almost died by suicide 15 years ago, launched an initiative to help those with mental illness choose life and to stop the expansion of euthanasia to the mentally ill.
Pierre Poilievre, leader of Canada’s Conservative Party praised one of his newest pro-life MPs, Andrew Lawton, for telling his story about almost dying by suicide, and for raising awareness of a bill that seeks to stop euthanasia from being expanded to those with mental illness.
“I want to thank Andrew for bravely coming forward to tell his story to try and help others suffering with their mental health,” wrote Poilievre on X last week.
Poilievre then thanked another one of his MPs, Tamara Jansen, for “leading the effort with Bill C-218 to protect these people and get them proper health care and treatment, not assisted suicide.”
As reported by LifeSiteNews, Conservative MP Lawton, who almost died in a suicide attempt 15 years ago, recently launched an initiative to help those struggling with mental illness choose life and to help stop a plan by the Canadian government to expand euthanasia to those with mental illness.
The Private Members Bill, C-218, or “An Act to amend the Criminal Code (medical assistance in dying [i.e., euthanasia]),” was introduced by Jansen and passed its first reading on June 20, 2025.
LifeSiteNews reported on Bill C-218, noting that Jansen said allowing “medical assistance in dying” (MAID) – a euphemism for assisted suicide – for those with mental illness is “not healthcare, that’s not compassion, it’s abandonment.”
“Mental illness is treatable. Recovery is possible, but only if we show up and help,” she told fellow MPs.
Jansen’s Bill C-218 reads, “This enactment amends the Criminal Code to provide that a mental disorder is not a grievous and irremediable medical condition for which a person could receive medical assistance in dying.”
The Conservative Party has attempted to oppose the expansion of euthanasia for some time, but recent legislative attempts to stop the expansion outright, instead of just delaying it, such as through Bill C-314, have failed.
Assisted suicide was legalized by the Liberal government of former Prime Minister Justin Trudeau in 2016.
Under the current law, assisted suicide is prohibited for minors and the mentally ill. Activists, however, have been pushing for these expansions with varying degrees of success.
In 2021, the Trudeau government expanded euthanasia from killing only “terminally ill” patients to allowing the chronically ill to qualify after the passage of Bill C-7. Since then, the government has sought to include those suffering solely from mental illness.
In February 2024, after pushback from pro-life, medical, and mental health groups as well as most of Canada’s provinces, the federal government delayed the mental illness expansion until 2027.
The expansion of euthanasia for the mentally ill is slated to become law in 2027 due to the passage of Bill C-7.
Health
New report warns WHO health rules erode Canada’s democracy and Charter rights
The Justice Centre for Constitutional Freedoms has released a new report titled Canada’s Surrender of Sovereignty: New WHO health regulations undermine Canadian democracy and Charter freedoms. Authored by Nigel Hannaford, a veteran journalist and researcher, the report warns that Canada’s acceptance of the World Health Organization’s (WHO) revised International Health Regulations (IHR) represents a serious erosion of national independence and democratic accountability.
The IHR amendments, which took effect on September 19, 2025, authorize the WHO Director-General to declare global “health emergencies” that could require Canada to follow directives from bureaucrats in Geneva, bypassing the House of Commons and the will of Canadian voters.
The WHO regards these regulations as “binding,” despite having no ability or legal authority to impose such regulations. Even so, Canada is opting to accept the regulations as binding.
By accepting the WHO’s revised IHR, the report explains, Canada has relinquished its own control over future health crises and instead has agreed to let the WHO determine when a “pandemic emergency” exists and what Canada must do to respond to it, after which Canada must report back to the WHO.
In fact, under these International Health Regulations, the WHO could demand countries like Canada impose stringent freedom-violating health policies, such as lockdowns, vaccine mandates, or travel restrictions without debate, evidence review, or public accountability, the report explains.
Once the WHO declares a “Pandemic Emergency,” member states are obligated to implement such emergency measures “without delay” for a minimum of three months.
Importantly, following these WHO directives would undermine government accountability as politicians may hide behind international “commitments” to justify their actions as “simply following international rules,” the report warns.
Canada should instead withdraw from the revised IHR, following the example of countries like Germany, Austria, Italy, Czech Republic, and the United States. The report recommends continued international cooperation without surrendering control over domestic health policies.
Constitutional lawyer Allison Pejovic said, “[b]y treating WHO edicts as binding, the federal government has effectively placed Canadian sovereignty on loan to an unelected international body.”
“Such directives, if enforced, would likely violate Canadians’ Charter rights and freedoms,” she added.
Mr. Hannaford agreed, saying, “Canada’s health policies must be made in Canada. No free and democratic nation should outsource its emergency powers to unelected bureaucrats in Geneva.”
The Justice Centre urges Canadians to contact their Members of Parliament and demand they support withdrawing from the revised IHR to restore Canadian sovereignty and reject blind compliance with WHO directives.
Business
Cutting Red Tape Could Help Solve Canada’s Doctor Crisis

From the Frontier Centre for Public Policy
By Ian Madsen
Doctors waste millions of hours on useless admin. It’s enough to end Canada’s doctor shortage. Ian Madsen says slashing red tape, not just recruiting, is the fastest fix for the clogged system.
Doctors spend more time on paperwork than on patients and that’s fueling Canada’s health care wait lists
Canada doesn’t just lack doctors—it squanders the ones it has. Mountains of paperwork and pointless admin chew up tens of millions of physician hours every year, time that could erase the so-called shortage and slash wait lists if freed for patient care.
Recruiting more doctors helps, but the fastest cure for our sick system is cutting the bureaucracy that strangles the ones already here.
The Canadian Medical Association found that unnecessary non-patient work consumes millions of hours annually. That’s the equivalent of 50.5 million patient visits, enough to give every Canadian at least one appointment and likely erase the physician shortage. Meanwhile, the Canadian Institute for Health Information estimates more than six million Canadians don’t even have a family doctor. That’s roughly one in six of us.
And it’s not just patients who feel the shortage—doctors themselves are paying the price. Endless forms don’t just waste time; they drive doctors out of the profession. Burned out and frustrated, many cut their hours or leave entirely. And the foreign doctors that health authorities are trying to recruit? They might think twice once they discover how much time Canadian physicians spend on paperwork that adds nothing to patient care.
But freeing doctors from forms isn’t as simple as shredding them. Someone has to build systems that reduce, rather than add to, the workload. And that’s where things get tricky. Trimming red tape usually means more Information Technology (IT), and big software projects have a well-earned reputation for spiralling in cost.
Bent Flyvbjerg, the global guru of project disasters, and his colleagues examined more than 5,000 IT projects in a 2022 study. They found outcomes didn’t follow a neat bell curve but a “power-law” distribution, meaning costs don’t just rise steadily, they explode in a fat tail of nasty surprises as variables multiply.
Oxford University and McKinsey offered equally bleak news. Their joint study concluded: “On average, large IT projects run 45 per cent over budget and seven per cent over time while delivering 56 per cent less value than predicted.” If that sounds familiar, it should. Canada’s Phoenix federal payroll fiasco—the payroll software introduced by Ottawa that left tens of thousands of federal workers underpaid or unpaid—is a cautionary tale etched into the national memory.
The lesson isn’t to avoid technology, but to get it right. Canada can’t sidestep the digital route. The question is whether we adapt what others have built or design our own. One option is borrowing from the U.S. or U.K., where electronic health record (EHR) systems (the digital patient files used by doctors and hospitals) are already in place. Both countries have had headaches with their systems, thanks to legal and regulatory differences. But there are signs of progress.
The U.K. is experimenting with artificial intelligence to lighten the administrative load, and a joint U.K.-U.S. study gives a glimpse of what’s possible:
“… AI technologies such as Robotic Process Automation (RPA), predictive analytics, and Natural Language Processing (NLP) are transforming health care administration. RPA and AI-driven software applications are revolutionizing health care administration by automating routine tasks such as appointment scheduling, billing, and documentation. By handling repetitive, rule-based tasks with speed and accuracy, these technologies minimize errors, reduce administrative burden, and enhance overall operational efficiency.”
For patients, that could mean fewer missed referrals, faster follow-up calls and less time waiting for paperwork to clear before treatment. Still, even the best tools come with limits. Systems differ, and customization will drive up costs. But medicine is medicine, and AI tools can bridge more gaps than you might think.
Run the math. If each “freed” patient visit is worth just $20—a conservative figure for the value of a basic appointment—the payoff could hit $1 billion in a single year.
Updating costs would continue, but that’s still cheap compared to the human and financial toll of endless wait lists. Cost-sharing between provinces, Ottawa, municipalities and even doctors themselves could spread the risk. Competitive bidding, with honest budgets and realistic timelines, is non-negotiable if we want to dodge another Phoenix-sized fiasco.
The alternative—clinging to our current dysfunctional patchwork of physician information systems—isn’t really an option. It means more frustrated doctors walking away, fewer new ones coming in, and Canadians left to languish on wait lists that grow ever longer.
And that’s not health care—it’s managed decline.
Ian Madsen is a senior policy analyst at the Frontier Centre for Public Policy.
-
 Alberta2 days ago
Alberta2 days agoClick here to help choose Alberta’s new licence plate design
-

 National2 days ago
National2 days agoDemocracy Watch Renews Push for Independent Prosecutor in SNC-Lavalin Case
-

 Business2 days ago
Business2 days agoOver two thirds of Canadians say Ottawa should reduce size of federal bureaucracy
-
 Media2 days ago
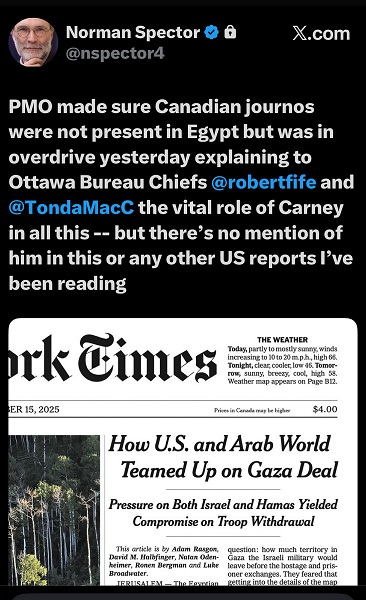
Media2 days agoCanada’s top Parliamentary reporters easily manipulated by the PMO’s “anonymous sources”
-

 Agriculture2 days ago
Agriculture2 days agoIs the CFIA a Rogue Agency or Just Taking Orders from a Rogue Federal Government?
-
 espionage2 days ago
espionage2 days ago“Suitcase of Cash” and Secret Meeting Deepen Britain’s Beijing Espionage Crisis
-
 Frontier Centre for Public Policy1 day ago
Frontier Centre for Public Policy1 day agoOttawa Should Think Twice Before Taxing Churches
-

 Alberta1 day ago
Alberta1 day agoBusting five myths about the Alberta oil sands




