Business
Pharma, WHO team up to create permanent ‘pandemic’ market for mandated, experimental vaccines

From LifeSiteNews
By Brenda Baletti, Ph.D., The Defender
Unlimited Hangout journalist Max Jones details how Big Pharma is using the WHO to restructure the drug market, so inadequately tested vaccines and other drugs will face minimal regulation and entire populations can be compelled to take them each time the WHO declares another global pandemic.
Big Pharma and its key investors are rolling out a new strategy — “the full takeover of the public sector, specifically the World Health Organization (WHO), and the regulatory system that now holds the entire market hostage” — according to a new investigative report by Unlimited Hangout’s Max Jones.
What’s behind the new strategy? The pharmaceutical industry is facing a “patent cliff” by 2030, as many of its blockbuster drugs are set to lose their patent protection, placing $180 billion in sales at risk and threatening to topple the industry.
According to Jones, for years, when patents expired on profitable drugs, pharmaceutical giants deployed a “mergers and acquisitions” strategy, buying up smaller drug companies to add to their product portfolios.
As a result, the industry is now dominated by a handful of companies, conventional chemical drugs exist for most health issues, and the regulatory process for new ones has become onerous.
Big Pharma has now pivoted to acquiring biotech and biologic companies, whose products are “more complex, unpredictable and difficult and expensive to make,” than chemical-based medicine, Jones wrote.
Conventional drugs are chemically synthesized and have a known structure according to the U.S. Food and Drug Administration (FDA). Biologics come from living humans, animal or microorganism cells, and are technologically altered to target particular proteins or cells in the immune system. The FDA calls biologics “complex mixtures that are not easily identified or characterized.”
As a drug class, biologics offer an appealing solution to the patent cliff problem, because they can’t be easily replicated like generic versions of conventional drugs.
Instead, producers make “biosimilars,” which unlike genetics can’t simply be interchanged with the original drug during a course of treatment without serious safety risks, according to Jones. And while generics are cheap, biosimilars are still expensive to produce. There also are regulatory hurdles to getting biosimilars to market.
However, Jones wrote, the serious safety issues associated with biologics — the high risk of serious adverse events associated with the COVID-19 vaccine, for example — make it difficult for drugmakers to find commercial success in a conventional regulatory environment.
“Luckily for Big Pharma,” Jones wrote, the WHO and its private backers “are pursuing an unprecedented legal process that would cement loopholes that could solve these significant market challenges of at least some biotechnologies.”
Such loopholes made Pfizer and Moderna’s COVID-19 mRNA vaccines — the paradigmatic example of this new strategy — Big Pharma’s highest-selling annual market success ever.
Distribution of the COVID-19 vaccines to approximately 70% of people globally was possible only because of the “fast-tracked, deregulated development and mandated consumption of the experimental drugs,” Jones wrote.
The industry hopes to replicate that model with other drugs. And it has already begun — last month the Biomedical Advanced Research and Development Authority, or BARDA, gave Moderna $176 million to develop an mRNA bird flu vaccine.
Stakeholders behind the WHO have turned it into an arm of Big Pharma
According to Jones, the process of rapidly developed and mandated experimental drugs was first adopted by the U.S. military for bioweapons threats. Now, it is being internationally legitimized by the WHO through the agency’s revisions to the International Health Regulations (IHR) and its continued attempt to push its pandemic treaty.
The amendments were watered down and the treaty was partially thwarted at the last meeting of the World Health Assembly, which ended on June 1. However, the powers added to the amendments and the language in the treaty WHO and its backers are still hoping to advance next year show the type of biotech pandemic market Big Pharma has in the works.
According to Jones, this market:
Will not be one that depends on the free will of consumers to opt in and out of products — but instead relies on tactics of forced consumption and manipulation of regulatory paradigms.
At the forefront of this push are the WHO’s public-private-partners/private stakeholders, who directly shape and benefit from this policy. Their influence has, in effect, turned the WHO into an arm of Big Pharma, one so powerful that it already demonstrated its ability to morph the entire international regulatory process for the benefit of the pharmaceutical industry during the COVID-19 pandemic.
These stakeholders can wield this power in part because the WHO receives 80% of its funding from private stakeholders.
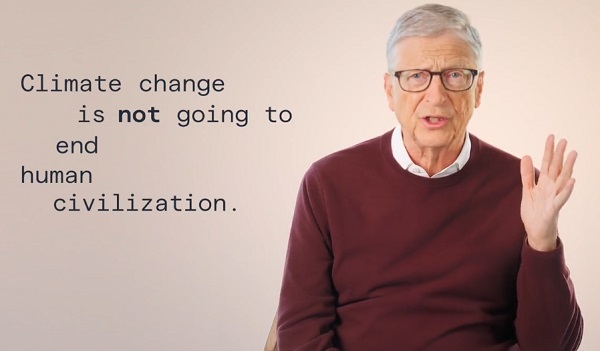
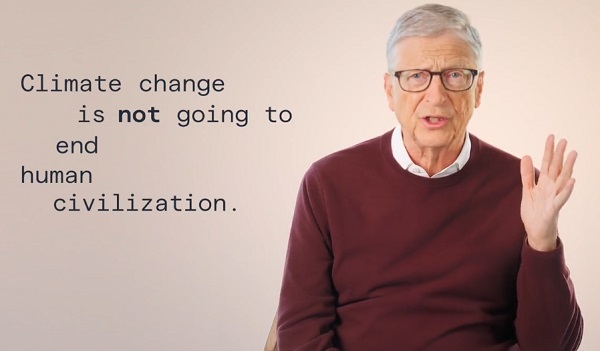
Those stakeholders include private-sector giants like Bill Gates, his public-private partnership organizations like the Coalition for Epidemic Preparedness Innovations (CEPI) and public-sector bureaucrats, such as Dr. Anthony Fauci and Rick Bright, Ph.D., of BARDA and the Rockefeller Foundation, who have been working for years to create a new system that would speed up vaccine production.
During the COVID-19 pandemic period, even states that lacked legal structures to provide emergency authorization for new drugs created them, using the WHO’s Emergency Use Listing Procedure (EUL) as justification, and aided by the WHO’s COVAX vaccine distribution system. COVAX was co-led by the WHO, Gavi, CEPI and Unicef, which are all backed by Gates.
The goal now, Jones wrote, is to institutionalize the procedures that were put in place globally for COVID-19 to pave the way for a new pandemic market.
The One Health agenda, which requires “full-scale surveillance of the human-animal environment,” both before and during pandemics, is central to this plan, he wrote.
The four pillars of the emerging pandemic market
There are four pillars to the plan for securing this market. The pillars are embodied in the WHO’s recently passed IHR amendments and the proposed pandemic treaty.
1. Biosurveillance of “pathogens with pandemic potential”: The WHO is calling on member states to create infrastructure to conduct biosurveillance on entire populations.
WHO private stakeholders, like the Wellcome Trust and the Bill & Melinda Gates Foundation, have been funding such initiatives for years and continue to be at the forefront of similar initiatives today, Jones wrote.
2. Rapid sharing of data and research: Under the IHR amendments, the WHO’s director-general must provide support for member states’ research and development. In the pending treaty, that would include helping them rapidly share data during a pandemic.
Such sharing should help coordinate global pandemic responses and also “pandemic prevention.” That means building a globally coordinated effort to research and share data on diseases that don’t currently pose a public health threat but are allegedly “likely to cause epidemics in the future.”
The WHO’s announcement last week that it is facilitating data-sharing for a new mRNA bird flu vaccine from Argentina is one example.
Experts have raised concerns that incentivizing such “preventive R&D” could incentivize risky gain-of-function research, Jones wrote.
Jones also noted that it is “highly likely” that the same global organizations that partner with the WHO and are funded by its largest private donors will be the ones doing this research and development on vaccines for “future pathogens with pandemic potential” — and also the ones profiting from it.
3. New regulatory pathways: The WHO is developing new regulatory pathways for unapproved medical products to get to market during pandemic emergencies. The IHR amendments are vague on this, Jones wrote, but the proposed language of the treaty aims to speed up emergency authorizations of WHO-recommended investigational “relevant health products.”
The proposed treaty also seeks to compel member countries to take steps to ensure they have the “legal, administrative and financial frameworks in place to support emergency regulatory authorizations for the effective and timely approval of pandemic-related health products during a pandemic.”
4. Global mandates of unapproved products: The final key element in the Big Pharma-WHO plan to pave the way for a new pandemic market is shoring up the global capacity to mandate unapproved medical products.
According to Jones, in July 2023, the WHO adopted the European Union’s (EU) digital COVID-19 passport system, or the “immunity pass” which recorded people’s vaccination records, negative test results or records of previous infections.
“While a digital vaccine passport does not function as a hard mandate in which every citizen of a given population is forced to take a vaccine, it acts as a conditional mandate — one which offers the illusion of choice, but — in reality — restricts the civil liberties of those who do not comply,” Jones wrote.
The 2005 version of the IHR allowed for travel-based mandates that required proof of vaccination to enter countries when there was a public health risk. The new IHR, Jones wrote, expands on this by detailing the kinds of technology that can be used to check such information during future pandemics.
The WHO also is developing its Global Digital Health Certification Network, which expands the EU digital passport system to a global scale. It will digitize vaccination records and health records and will be “interoperable” with existing networks.
While interoperability makes it possible for decentralized data to be shared globally, Jones wrote, “The UN is seeking to impose digital identification as a ‘human right,’ or rather as a condition for accessing other human rights, for the entire global citizenry by 2030, as established in its Sustainable Development Goal 16.9.”
The initiative seeks to provide people with a “trusted, verifiable way” to prove who they are in the physical world and online.
Verification systems of this size will place the right of citizens to do basic activities — like traveling, eating at a restaurant or working their job — in the hands of governments and potentially employers.
The rights of civilians will be conditional, dictated by data stored in a massive digital hub that is global in its sharing abilities. Not only will domestic governments have access to the health information of their own citizens under this system, but an entire global bureaucracy will as well.
This article was originally published by The Defender — Children’s Health Defense’s News & Views Website under Creative Commons license CC BY-NC-ND 4.0. Please consider subscribing to The Defender or donating to Children’s Health Defense.
Business
No Jobs Clause: Liberals Under Fire Over Stellantis Deal in Fiery Committee Showdown

It was less of an industrial strategy and more of a cultural manifesto wrapped in a subsidy package… clause after clause mandates social goals: The “50-30 Challenge” pushes for 50% women and 30% underrepresented groups on boards, with detailed reporting on diversity metrics… But job protections? Squishy at best.
Folks, here’s why every Canadian should be boiling mad: Just two years ago, on May 2, 2023, Justin Trudeau’s Liberals were all grins and photo ops, announcing a whopping $15 billion deal with Stellantis to build the NextStar EV battery plant in Windsor, Ontario. Trudeau himself called it a “historic agreement” that would “create thousands of well-paying jobs” and position Canada as a leader in electric vehicles. But fast-forward to October 14, 2025, and Stellantis pulls the plug on Brampton: They’re shifting production of the Jeep Compass from the Ontario plant to Belvidere, Illinois, citing “market conditions” exacerbated by Donald Trump’s reinstated 25% tariffs on Canadian-made vehicles. As Reuters reported on November 3, 2025, those tariffs—slapped on earlier this year—made it untenable to keep building in Canada for the U.S. market. Result? 3,000 workers laid off indefinitely, a facility idled since February 2024, and billions in taxpayer subsidies looking like a sucker punch. Stellantis isn’t even hiding it; their press release that day admitted the move was to “optimize operations” amid tariff pressures, investing $600 million in Illinois instead.
It’s a question that should make every Canadian furious, particularly anyone who still believes that the government’s role is to defend the nation’s workers rather than sell them out to foreign multinationals under the guise of “green investment.” The Trudeau government—with a lot of ribbon-cutting, back-patting, and press conference confetti—told us this was a generational opportunity. Up to $15 billion of taxpayer money was pledged through a combination of federal and Ontario subsidies, a massive, glittering pile of cash dumped at the feet of a foreign company to secure so-called “green jobs” in the electric vehicle sector. Split two-thirds federal and one-third provincial, it’s tied to production incentives—paid per kilowatt-hour as batteries roll out, not upfront, per the redacted contract leaked by CBC on October 29, 2025. But that didn’t stop the Liberals from hyping it as a slam-dunk for Canada’s economy.
At the time, Liberal ministers paraded through Windsor and Brampton with photographers in tow, declaring that the NextStar EV battery plant and a retooled Brampton assembly line would solidify Canada’s future in the EV revolution. The Strategic Innovation Fund was rolled out like a magic wand—promising prosperity, sustainability, and, of course, “equity.” Not just for jobs, but for gender representation, for racial diversity on corporate boards, for net-zero targets. It was less of an industrial strategy and more of a cultural manifesto wrapped in a subsidy package. As revealed in the CBC-leaked documents, clause after clause mandates social goals: The “50-30 Challenge” pushes for 50% women and 30% underrepresented groups on boards, with detailed reporting on diversity metrics. Climate commitments? Baked in, with net-zero benchmarks. But job protections? Squishy at best.
But now, Stellantis is pulling up stakes in Brampton. They’re shipping production of the Jeep Compass south—to Illinois. The line is shutting down. Three thousand jobs are gone, and Ottawa’s response? A letter. A procedural dispute-resolution letter sent to Stellantis lawyers on November 3, 2025, with the government now claiming the company broke a “binding agreement.” As Industry Minister Mélanie Joly told the parliamentary committee that day, “We will start the 30-day period of the formal dispute resolution process in order to bring back production at the Stellantis Brampton facility.” She added, “These actions are not symbolic. They’re the direct consequence of the violation of clear commitments.” The same government that only weeks ago was hailing this deal as a model for the future now admits it may not even contain an enforceable jobs guarantee. The language is vague. The numbers are redacted. The accountability? Nonexistent.
The Industry Minister, Mélanie Joly, faced her grilling on Parliament Hill during a meeting of the House of Commons Standing Committee on Industry and Technology (INDU)—that exposed just how hollow this whole deal really was. Conservative MPs, including Raquel Dancho and Michael Guglielmo, demanded to see the clause. Which clause did Stellantis allegedly violate? What exactly was the commitment to Brampton? How many jobs were actually guaranteed? Was there a number? Was it enforceable? The Minister couldn’t—or wouldn’t—say. She deflected, pointed to redacted documents, and, when pressed about why the contract was packed with detailed social engineering mandates on board diversity but lacked hard job protections, accused her critics of being “against women.”
You can’t make this up.
Raquel Dancho, hammering in the core question that everyone watching already knew the answer to, asked,
“Was it 3,000 jobs that that SIF agreement with Brampton guaranteed?”
The minister responded like a bureaucratic ghost, floating just above the substance of the question.
“There are job guarantees in all the different contracts,” she said, “but you absolutely need to make sure that you see not only the contract… but also its amendment.”
Translation: Trust us. It’s in there somewhere. You just can’t see it.
Dancho pushed again: Where’s the number? Where’s the clause? The minister replied, “Clearly it is about protecting jobs. It is also about the production at the Brampton facility.” Not a single figure. Not a single line reference. Just the usual empty affirmation: “We care.”
Dancho didn’t let up. She cut through the fluff with brutal clarity:
“Surely there should be an explicit Canada-wide jobs guarantee. But we’re splitting hairs here. You’ve been evasive about the numbers… I’m not sure if you understand the magnitude of the money that you’ve committed.”
Then came the math:
“Over 647,000 full-time, two-parent Canadian families had to work an entire year to provide the $11 billion your government handed over to Stellantis. And still, there’s no explicit jobs guarantee.”
And when Michael Guglielmo followed up with the most damning observation of all—why are the clearest commitments in this contract about gender and racial equity quotas, not Canadian jobs?—the minister didn’t even deny it. She shot back with the cheap and predictable counterpunch:
“Are you against women being on boards?”
This is what it’s come to.
Instead of defending Canadian workers, the minister defends ideological clauses. Instead of admitting they cut a $15 billion cheque without a locked-down jobs guarantee, they imply that questioning the deal is somehow anti-diversity. These people don’t just miss the point—they refuse to even stand in the same room as the point.
Because the priority wasn’t jobs. It was ideology. The contract’s most detailed provisions weren’t about keeping Canadians employed—they were about the “50-30 challenge,” ensuring that Stellantis boards hit quotas: 50% women or non-binary individuals, 30% racialized, LGBTQ+, Indigenous, or disabled. These were enforceable clauses. Meanwhile, the 3,000 Brampton workers whose plant just shut down got… vibes.
That’s not economic strategy. That’s social engineering masquerading as industrial policy.
And now, when the jobs are gone, when Brampton is shuttered, when the workers are packing up their toolboxes and wondering how they’re going to pay their mortgage, the Liberals say they’re “launching a dispute-resolution process.” They sent a letter. They held a press conference. The Prime Minister, not present. The Minister, ducking behind amendments and redactions. And Canadians are left asking the only question that matters: Did we just get played?
Yes. We did.
The Liberals want you to believe this is just the price of doing business in a green economy. That global supply chains shift. That the transition to EVs is complicated. That we must continue to “work together.” But that’s not leadership. That’s surrender. The truth is, this wasn’t an industrial strategy—it was a $15 billion act of political performance art. A press release dressed up as policy. A parade of woke checkboxes signed into law while real, blue-collar livelihoods were used as bait.
And now we’re paying for it—not just in tax dollars, but in lost paychecks, empty factories, and shattered trust.
This is what happens when your government governs with hashtags instead of handshakes. When they negotiate with ideology, not leverage. When they cut billion-dollar deals and forget to actually protect the people they claim to represent.
Stellantis didn’t betray Brampton. The Liberal government did.
If there was a real deal—an actual, enforceable agreement that tied billions in taxpayer money to thousands of Canadian jobs—we’d be hearing about it nonstop. The Liberals wouldn’t be hiding behind redactions, amendments, and vague references to “linked contracts.” They’d be shouting from every podium: Here’s the clause. Here’s the violation. Here’s the money we’re clawing back. But instead, what do we get?
We get, “You’ll find it.”
We get, “It’s in the amendment.”
We get, “It’s commercially sensitive.”
It’s a shell game. A bureaucratic sleight of hand. Because the truth is, if this government had locked in a rock-solid guarantee, they’d be waving it in your face. They’d be naming names and quoting line numbers. But they can’t. Because it doesn’t exist. Or worse, because they were too arrogant or incompetent to include it in the first place.
And frankly, I’m not surprised. We’ve come to expect this from a Liberal government that governs by photo op and backpedals by committee. But what this is really about—what this entire spectacle reveals—is not just incompetence. It’s the desperate attempt to hide that incompetence from their own base. To maintain the illusion that they’re builders of the future while the factories go dark behind them.
They knew what they were doing. They just didn’t care who paid for it.
Business
Carney government’s first budget should signal end to crippling ‘climate’ policies

From the Fraser Institute
The Carney government will table its long-awaited first budget tooday. The vote on the budget is expected to be a confidence vote, so the stakes are high. Everyone is speculating about what’s to be in it. CBC, the Toronto Sun and Global News are all reading the tea leaves. And I hate to miss a tea party.
The budget is, naturally, going to have major implications for Canada’s economic indicators of debt, deficit, spending, governmental expansion/contraction, and so on. I’ll leave all that macroeconomics to my colleagues at Fraser Institute. But Prime Minister Carney has made some specific claims in my areas of specialty (environment, natural resources and regulation), and has made noises about Canada becoming an “energy superpower” and “building things” again. He’s also, in speeches leading up to the budget, re-affirmed that the Trudeau-era climate-change-centric, carbon-emission-control mindset is unchanged. The wording has changed, but the focus and predicates remain. Now though, rather than pounding on terms such as carbon, greenhouse and climate change, it’s all about Canadian policy being “responsible,” “sustainable,” “moral” and “equitable.”
Here’s what I’ll look for in the budget.
First, will the government dismantle or reform bills C-48, C-69 and the oil and gas emission cap—the three-pronged trident of death for major oil and gas development in Canada? Without this, it will be difficult to take any of his talk of energy superpower or natural resource trade renaissance seriously.
Second, will the government renounce or seriously reform the economically irrational, unattainable and crippling “net-zero 2050” anti-carbon agenda and shift Canada’s climate policy from emissions abatement to something potentially more attainable, such as adaptation and resilience building? Will it free Canada’s carbon natural resource economy to be the engine of Canadian prosperity and international competitiveness once again? Or keep Canada’s carbon (oil and gas) economy (and manufacturing economy) on a path toward extinction?
Third, will the government reset the tone of Canadian culture and defuse some of the adversarial relations with resource-rich provinces by acknowledging that Canada’s natural-resource economy has been, is now and must continue to be a cornerstone in Canada’s total economy? Or will it stick to the “net-zero” extinction process for carbon emissions, which will also be an extinction process for anything that requires substantial energy generation, and for the development of natural resources as the primary wealth engine of Canada? Will the government end the disdain for the role of Canada (and notably some of Canada’s western provinces) as a natural-resources export economy?
The budget will offer a window into the mind of Prime Minister Carney on the matter of natural resources in Canada’s economy and society. With global changes undermining the international carbon control regime and idee fixe, and with an understanding that Canada is on an economic precipice, there’s an opportunity here. Let’s hope Carney works to unshackle one of Canada’s greatest engines of economic progress—its energy and natural resource production, transformation, transportation, consumption and exportation.
Canadians could use the boost in quality of life that Canada’s natural resources could bring to current and future generations.
-

 Crime2 days ago
Crime2 days agoPublic Execution of Anti-Cartel Mayor in Michoacán Prompts U.S. Offer to Intervene Against Cartels
-
 Environment2 days ago
Environment2 days agoThe era of Climate Change Alarmism is over
-

 Aristotle Foundation2 days ago
Aristotle Foundation2 days agoB.C. government laid groundwork for turning private property into Aboriginal land
-

 Justice2 days ago
Justice2 days agoA Justice System That Hates Punishment Can’t Protect the Innocent
-

 Alberta1 day ago
Alberta1 day agoCanada’s heavy oil finds new fans as global demand rises
-

 Business1 day ago
Business1 day agoCarney government should retire misleading ‘G7’ talking point on economic growth
-

 Censorship Industrial Complex1 day ago
Censorship Industrial Complex1 day agoPro-freedom group warns Liberal bill could secretly cut off Canadians’ internet access
-

 Daily Caller1 day ago
Daily Caller1 day agoNigeria Would Welcome US Intervention In Massacre Of Christians By Islamic Terror Groups








