Addictions
Ontario to close 10 safe consumption sites and open 19 recovery hubs

A photo of the South Riverdale neighbourhood. (Photo credit: Andrea Nickel)
News release from Break The Needle

Ontario’s decision to close safe consumption sites near schools and daycares comes in the wake of a bystander’s death and class-action lawsuit
In a dramatic shift in policy, Ontario is closing 10 safe consumption sites located near schools and daycares, citing public safety concerns.
“Our first priority must always be protecting our communities, especially when it comes to our most innocent and vulnerable — our children,” said Ontario Health Minister Sylvia Jones at an Association of Municipalities of Ontario conference in Ottawa on Tuesday.
Safe consumption sites, which enable people to use illicit drugs with sterile equipment under staff supervision, will be prohibited from operating within 200 metres of schools and child-care centres after March 31, 2025.
The province also plans to introduce legislation to prevent municipalities from establishing new consumption sites, requesting the decriminalization of illegal drugs or participating in federal safe supply initiatives, a health ministry press release says.
Safe consumption sites have faced mounting scrutiny in the wake of community feedback highlighting their effect on public safety.
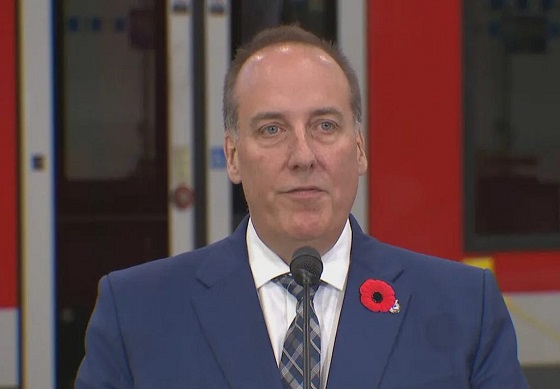
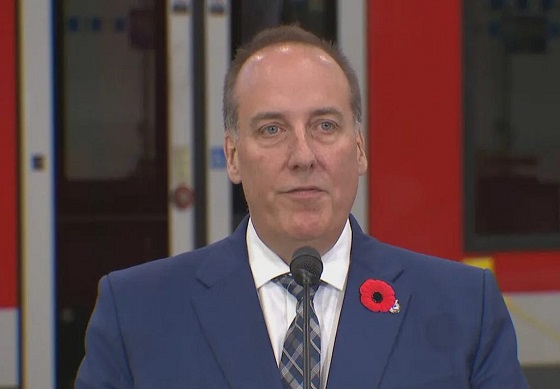
“We’ve noticed a real change from 2021 onwards,” Andrea Nickel, a parent who lives near a safe consumption site at Toronto’s South Riverdale Community Health Centre, told Canadian Affairs in May.
“At the beginning of last year it just escalated out of control.”
Unacceptable danger
Ontario opened its first safe consumption site in 2017 with the aim of reducing overdose deaths and providing users with a gateway to treatment. Today, there are 23 safe consumption sites across the province, 17 of which are provincially funded.
KeepSIX, the safe consumption site in South Riverdale, is among the sites facing closure. Last July, Karolina Huebner-Makurat, a local resident and mother of two, was fatally shot during a gunfight outside the site. Her death prompted Ontario to conduct two reviews of the centre and to also review the 16 other provincially funded sites.
A review of keepSIX conducted by the hospital network Unity Health Toronto and released in February recommended improvements in security, community relations, law enforcement communication and staff training. It did not recommend closure.
The second review, released in April and conducted by former health-care executive Jill Campbell, also opposed closure. It advocated instead for expanded harm reduction and treatment, enhanced security and increased mental health support.
In March 2024, two South Riverdale residents launched a class-action lawsuit against the operator of keepSIX and all levels of government, Canadian Affairs reported in May. The lawsuit alleges the site has exposed the community to unacceptable danger.
The site’s proximity to daycares and schools and its role in exposing children to illicit drugs and used needles are at the heart of that case.
Reacting to this week’s announcement, South Riverdale parent Andrea Nickel said she is supportive of the site’s services. “[But] it is not unreasonable to ask that they are balanced with community safety, specifically kids’ safety.”
South Riverdale’s response cited the centre’s role in reversing 74 overdoses in 2023.
“Every overdose reversed is a life saved,” Anne Marie Aikins, a public affairs consultant at AMA Communications, said on behalf of the centre.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
‘Devil’s in the details’
In Tuesday’s address, Ontario’s health minister also announced a $378-million investment to establish 19 new Homelessness and Addiction Recovery Treatment Hubs (HART hubs) across the province. These recovery-focused hubs will offer social support services and employment assistance to individuals struggling with addiction.
They will not provide supervised drug consumption, needle exchange programs or the “safe supply” of prescribed controlled substances.
“The devil’s in the details with these things,” said John-Paul Michael, an addictions case manager in Toronto who has extensive experience in harm reduction and lived experience with substance use.
“Everyone I know in the harm-reduction community is very much in favour of having better access to treatment, better access to detox, better wraparound care,” he said. “The problem becomes when it is at the expense of other evidence-based care.”
Michael says safe consumption sites are often the only form of health care available to individuals struggling with addiction. Eliminating them would leave these individuals without support, he says.
“Safe consumption sites are essential for saving lives, particularly for those who may never seek formal treatment,” he said. “Eliminating these supports disregards the value of human life.”
Michael is also concerned about the reduction of needle exchange services, which are crucial for managing HIV and Hepatitis C rates and lessening the burden on emergency rooms.
“Community-based nurses at [safe consumption sites] provide basic care that can prevent emergency department visits and potentially severe outcomes, such as [intensive care unit] stays,” Michael said.
The province will soon seek proposals to establish up to 10 HART hubs. Priority will be given to proposals that aim to transition existing safe consumption sites — especially those facing closure — into HART hubs.
“[T]he likelihood is that [these transitions] would happen very quickly,” Health Minister Jones told reporters on Tuesday. “The other applications — it will depend on what they bring forward.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Addictions
Canadian gov’t not stopping drug injection sites from being set up near schools, daycares

From LifeSiteNews
Canada’s health department told MPs there is not a minimum distance requirement between safe consumption sites and schools, daycares or playgrounds.
So-called “safe” drug injection sites do not require a minimum distance from schools, daycares, or even playgrounds, Health Canada has stated, and that has puzzled some MPs.
Canadian Health Minister Marjorie Michel recently told MPs that it was not up to the federal government to make rules around where drug use sites could be located.
“Health Canada does not set a minimum distance requirement between safe consumption sites and nearby locations such as schools, daycares or playgrounds,” the health department wrote in a submission to the House of Commons health committee.
“Nor does the department collect or maintain a comprehensive list of addresses for these facilities in Canada.”
Records show that there are 31 such “safe” injection sites allowed under the Controlled Drugs And Substances Act in six Canadian provinces. There are 13 are in Ontario, five each in Alberta, Quebec, and British Columbia, and two in Saskatchewan and one in Nova Scotia.
The department noted, as per Blacklock’s Reporter, that it considers the location of each site before approving it, including “expressions of community support or opposition.”
Michel had earlier told the committee that it was not her job to decide where such sites are located, saying, “This does not fall directly under my responsibility.”
Conservative MP Dan Mazier had asked for limits on where such “safe” injection drug sites would be placed, asking Michel in a recent committee meeting, “Do you personally review the applications before they’re approved?”
Michel said that “(a)pplications are reviewed by the department.”
Mazier stated, “Are you aware your department is approving supervised consumption sites next to daycares, schools and playgrounds?”
Michel said, “Supervised consumption sites were created to prevent overdose deaths.”
Mazier continued to press Michel, asking her how many “supervised consumption sites approved by your department are next to daycares.”
“I couldn’t tell you exactly how many,” Michel replied.
Mazier was mum on whether or not her department would commit to not approving such sites near schools, playgrounds, or daycares.
An injection site in Montreal, which opened in 2024, is located close to a kindergarten playground.
Conservative Party leader Pierre Poilievre has called such sites “drug dens” and has blasted them as not being “safe” and “disasters.”
Records show that the Liberal government has spent approximately $820 million from 2017 to 2022 on its Canadian Drugs and Substances Strategy. However, even Canada’s own Department of Health admitted in a 2023 report that the Liberals’ drug program only had “minimal” results.
Recently, LifeSiteNews reported that the British Columbia government decided to stop a so-called “safe supply” free drug program in light of a report revealing many of the hard drugs distributed via pharmacies were resold on the black market.
British Columbia Premier David Eby recently admitted that allowing the decriminalization of hard drugs in British Columbia via a federal pilot program was a mistake.
Former Prime Minister Justin Trudeau’s loose drug initiatives were deemed such a disaster in British Columbia that Eby’s government asked Trudeau to re-criminalize narcotic use in public spaces, a request that was granted.
Official figures show that overdoses went up during the decriminalization trial, with 3,313 deaths over 15 months, compared with 2,843 in the same time frame before drugs were temporarily legalized.
Addictions
Canada is divided on the drug crisis—so are its doctors

When it comes to addressing the national overdose crisis, the Canadian public seems ideologically split: some groups prioritize recovery and abstinence, while others lean heavily into “harm reduction” and destigmatization. In most cases, we would defer to the experts—but they are similarly divided here.
This factionalism was evident at the Canadian Society of Addiction Medicine’s (CSAM) annual scientific conference this year, which is the country’s largest gathering of addiction medicine practitioners (e.g., physicians, nurses, psychiatrists). Throughout the event, speakers alluded to the field’s disunity and the need to bridge political gaps through collaborative, not adversarial, dialogue.
This was a major shift from previous conferences, which largely ignored the long-brewing battles among addiction experts, and reflected a wider societal rethink of the harm reduction movement, which was politically hegemonic until very recently.
Recovery-oriented care versus harm reductionism
For decades, most Canadian addiction experts focused on shepherding patients towards recovery and encouraging drug abstinence. However, in the 2000s, this began to shift with the rise of harm reductionism, which took a more tolerant view of drug use.
On the surface, harm reductionists advocated for pragmatically minimizing the negative consequences of risky use—for example, through needle exchanges and supervised consumption sites. Additionally, though, many of them also claimed that drug consumption is not inherently wrong or shameful, and that associated harms are primarily caused not by drugs themselves but by the stigmatization and criminalization of their use. In their view, if all hard drugs were legalized and destigmatized, then they would eventually become as banal as alcohol and tobacco.
The harm reductionists gained significant traction in the 2010s thanks to the popularization of street fentanyl. The drug’s incredible potency caused an explosion of deaths and left users with formidable opioid tolerances that rendered traditional addiction medications, such as methadone, less effective. Amid this crisis, policymakers embraced harm reduction out of an immediate need to make drug use slightly less lethal. This typically meant supervising consumption, providing sterile drug paraphernalia, and offering “cleaner” substances for addicts to use.
Many abstinence-oriented addiction experts supported some aspects of harm reduction. They valued interventions that could demonstrably save lives without significant tradeoffs, and saw them as both transitional and as part of a larger public health toolkit. Distributing clean needles and Naloxone, an overdose-reversal medication, proved particularly popular. “People can’t recover if they’re dead,” went a popular mantra from the time.
Saving lives or enabling addiction?
However, many of these addiction experts were also uncomfortable with the broader political ideologies animating the movement and did not believe that drug use should be normalized. Many felt that some experimental harm reduction interventions in Canada were either conceptually flawed or that their implementation had deviated from what had originally been promised.
Some argued, not unreasonably, that the country’s supervised consumption sites are being mismanaged and failing to connect vulnerable addicts to recovery-oriented care. Most of their ire, however, was directed at “safer supply”—a novel strategy wherein addicts are given free drugs, predominantly hydromorphone (a heroin-strength opioid), without any real supervision.
While safer supply was meant to dissuade recipients from using riskier street drugs, addiction physicians widely reported that patients were selling their free hydromorphone to buy stronger illicit fentanyl, thereby flooding communities with diverted opioids and exacerbating the addiction crisis. They also noted that the “evidence base” behind safer supply was exceptionally poor and would not meet normal health-care standards.
Yet, critics of safer supply, and harm reduction radicalism more broadly, were often afraid to voice their opinions. The harm reductionists were institutionally and culturally dominant in the late 2010s and early 2020s, and opponents often faced activist harassment, aggressive gaslighting, and professional marginalization. A culture of self-censorship formed, giving both the public and influential policymakers a false impression of scientific consensus where none actually existed.
The resurgence in recovery-oriented strategies
Things changed in the mid-2020s. British Columbia’s failed drug decriminalization experiment eroded public trust in harm reductionism, and the scandalous failures of safer supply—and supervised consumption sites, too—were widely publicized in the national media.1
Whereas harm reductionism was once so powerful that opponents were dismissed as anti-scientific, there is now a resurgent interest in alternative, recovery-oriented strategies.
These cultural shifts have fuelled a more fractious, but intellectually honest, national debate about how to tackle the overdose crisis. This has ruptured the institutional dominance enjoyed by harm reductionists in the addiction medicine world and allowed their previously silenced opponents to speak up.
When I first attended CSAM’s annual scientific conference two years ago, recovery-oriented critics of radical harm reductionism were not given any platforms, with the exception of one minor presentation on safer supply diversion. Their beliefs seemed clandestine and iconoclastic, despite seemingly having wide buy-in from the addiction medicine community.
While vigorous criticism of harm reductionism was not a major feature of this year’s conference, there was open recognition that legitimate opposition to the movement existed. One major presentation, given by Dr. Didier Jutras-Aswad, explicitly cited safer supply and involuntary treatment as two foci of contention, and encouraged harm reductionists and recovery-oriented experts to grab coffee with one another so that they might foster some sense of mutual understanding.2
Is this change enough?
While CSAM should be commended for encouraging cross-ideological dialogue, its efforts, in this respect, were also superficial and vague. They chose to play it safe, and much was left unsaid and unexplored.
Two addiction medicine doctors I spoke with at the conference—both of whom were critics of safer supply and asked for anonymity—were nonplussed. “You can feel the tension in the air,” said one, who likened the conference to an awkward family dinner where everyone has tacitly agreed to ignore a recent feud. “Reconciliation requires truth,” said the other.
One could also argue that the organization has taken an inconsistent approach to encouraging respectful dialogue. When recovery-oriented experts were being bullied for their views a few years ago, they were largely left on their own. Now that their side is ascendant, and harm reductionists are politically vulnerable, mutual respect is in fashion again.
When I asked to interview the organization about navigating dissension, they sent a short, unspecific statement that emphasized “evidence-based practices” and the “benefits of exploring a variety of viewpoints, and the need to constantly challenge or re-evaluate our own positions based on the available science.”
But one cannot simply appeal to “evidence-based practices” when research is contentious and vulnerable to ideological meddling or misrepresentation.
Compared to other medical disciplines, addiction medicine is highly political. Grappling with larger, non-empirical questions about the role of drug use in society has always necessitated taking a philosophical stance on social norms, and this has been especially true since harm reductionists began emphasizing the structural forces that shape and fuel drug use.
Until Canada’s addiction medicine community facilitates a more robust and open conversation about the politicization of research, and the divided—and inescapably political—nature of their work, the national debate on the overdose crisis will be shambolic. This will have negative downstream impacts on policymaking and, ultimately, people’s lives.
Our content is always free – but if you want to help us commission more high-quality journalism,
consider getting a voluntary paid subscription.
-
 Alberta2 days ago
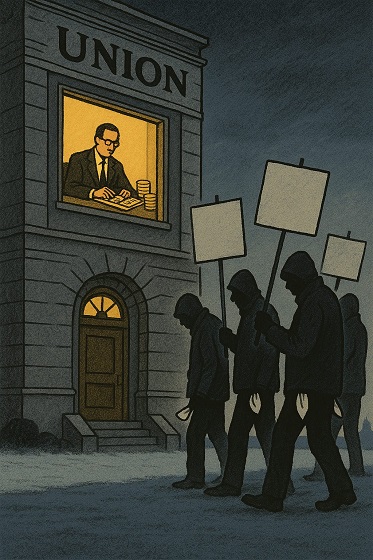
Alberta2 days agoATA Collect $72 Million in Dues But Couldn’t Pay Striking Teachers a Dime
-
 Media2 days ago
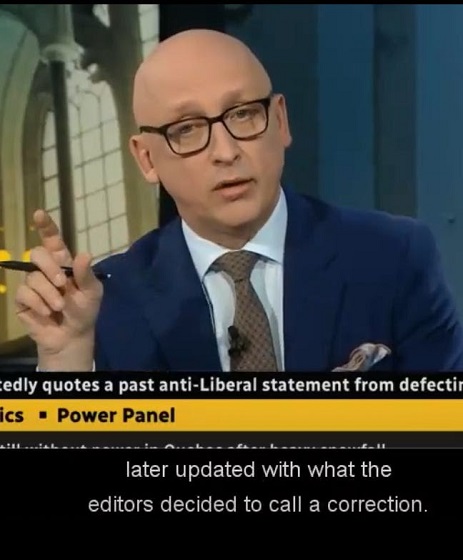
Media2 days agoBreaking News: the public actually expects journalists to determine the truth of statements they report
-

 Artificial Intelligence2 days ago
Artificial Intelligence2 days agoAI seems fairly impressed by Pierre Poilievre’s ability to communicate
-

 Business2 days ago
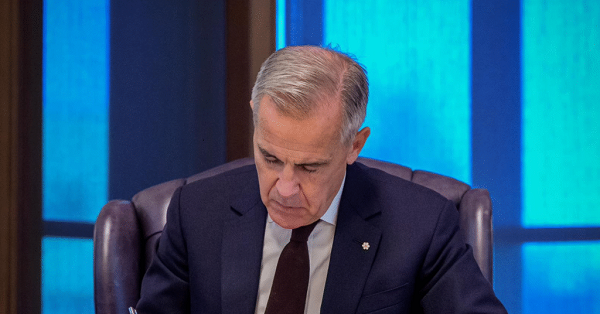
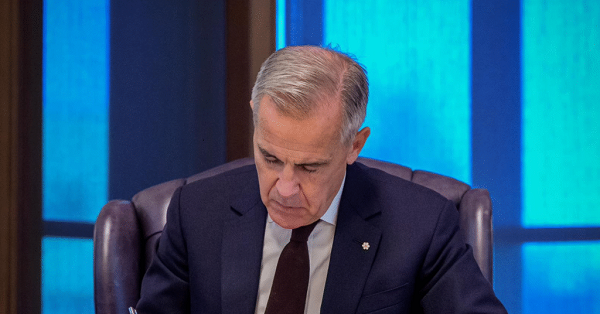
Business2 days agoCarney doubles down on NET ZERO
-
 National2 days ago
National2 days agoWatchdog Demands Answers as MP Chris d’Entremont Crosses Floor
-
 Business2 days ago
Business2 days agoLiberal’s green spending putting Canada on a road to ruin
-

 Alberta16 hours ago
Alberta16 hours agoCalgary mayor should retain ‘blanket rezoning’ for sake of Calgarian families
-

 Alberta13 hours ago
Alberta13 hours agoNational Crisis Approaching Due To The Carney Government’s Centrally Planned Green Economy









