Addictions
Ontario reviewing supervised consumption sites after Toronto shooting death
A woman weeps as mourners tie yellow ribbons and flowers to a fence following public vigil for Karolina Huebner-Makurat, in Toronto, Monday, July 17, 2023. Ontario says it has launched a “critical incident review” of the province’s supervised consumption sites after a woman was killed by a stray bullet in Toronto’s east end last month. THE CANADIAN PRESS/Chris Young
Toronto
Ontario says it has launched a “critical incident review” of the province’s supervised consumption sites after a woman was killed by a stray bullet in Toronto’s east end last month.
Hannah Jensen, a spokesperson for Health Minister Sylvia Jones, says all sites are expected to comply with strict requirements and the review will start with the South Riverdale Community Health Centre near the scene of Karolina Huebner-Makurat’s death.
Police have said the 44-year-old mother of two was walking in the Leslieville neighbourhood on July 7 when she was hit by a stray bullet after a physical altercation between three men resulted in shots being fired.
Three people are facing charges in her death, including 23-year-old SRCHC community worker Khalila Zara Mohammed who is charged with being an accessory after the fact and obstructing justice.
Twenty-year-old Ahmed Mustafa Ibrahim was also arrested and charged this week with manslaughter and robbery, while 32-year-old Damian Hudson was arrested last month and charged with second-degree murder.
None of the charges have been proven in court and Toronto police say they are still looking for a third suspect involved in the shooting.
This report by The Canadian Press was first published Aug. 17, 2023.
Addictions
“Safer supply” reminiscent of the OxyContin crisis, warns addiction physician

Dr. Lori Regenstreif, MD, MSc, CCFP (AM), FCFP, MScCH (AMH), CISAM, has been working as an addiction medicine physician in inner city Hamilton, Ontario, since 2004. She co-founded the Shelter Health Network in 2005 and the Hamilton Clinic’s opioid treatment clinic in 2010, and helped found the St. Joseph’s Hospital Rapid Access Addiction Medicine (RAAM) clinic.
|
[This article is part of Break The Needle’s “Experts Speak Up” series, which documents healthcare professionals’ experiences with Canada’s “safer supply” programs] By: Liam Hunt
Dr. Lori Regenstreif, an addiction physician with decades of experience on the frontlines of Canada’s opioid crisis, is sounding the alarm about the country’s rapidly expanding “safer supply” programs.
While proponents of safe supply contend that providing drug users with free tablets of hydromorphone – a pharmaceutical opioid roughly as potent as heroin – can mitigate harms, Dr. Regenstreif expresses grave concern that these programs may inadvertently perpetuate new addictions and entrench existing opioid use.
She sees ominous similarities between safer supply and the OxyContin crisis of the late 1990s, when the widespread overprescribing of opioids flooded North American communities with narcotics, sparking an addiction crisis that continues to this day. Having witnessed the devastating consequences of OxyContin in the late 1990s, she believes that low-quality and misleading research is once again encouraging dangerous overprescribing practices.
Flashbacks to the OxyContin Crisis
Soon after Dr. Regenstreif received her medical license in Canada, harm reduction became the primary framework guiding her practice in inner-city Vancouver. This period coincided with Health Canada’s 1996 regulatory approval of oxycodone (brand name: OxyContin) based on trials, sponsored by Purdue Pharma, that failed to assess the serious risks of misuse or addiction.
Dr. Regenstreif subsequently witnessed highly addictive prescription opioids flood North American streets while Purdue and its distributors reaped record profits at the expense of vulnerable communities. “That was really peaking in the late 90s as I was coming into practice,” she recounted during an extended interview with Break The Needle. “I was being pressured to prescribe it as well.”
Oxycodone addiction led to the deaths of tens of thousands of individuals in the United States and Canada. As a result, Purdue Pharma faced criminal penalties, fines, and civil settlements amounting to 8.5 billion USD, ultimately leading to the company’s bankruptcy in 2019.
During the OxyContin crisis, patients would regularly procure large amounts of pharmaceutical opioids for resale on the black market – a process known as “diversion.” Dr. Regenstreif has seen alarming indications that safer supply hydromorphone is being diverted at similarly high levels, and estimated that, out of her patient pool, “15 to 20 out of maybe 40 people who have to go to a pharmacy frequently” have reported witnessing diversion.
Between one to two thirds of her new patients have told her that they are accessing diverted hydromorphone tablets – in many cases, the tablets almost certainly originate from safer supply.
Injecting crushed hydromorphone tablets pose severe health risks, including endocarditis and spinal abscesses. “I’ve seen people become quadriplegic and paraplegic because the infection invaded their spinal cord and damaged their nervous system,” said Dr. Regenstreif. While infections can be mitigated by reducing the number of times drug users inject drugs into their bodies, she says that safer supply programs do not discourage or reduce injections.
She further noted, “I’ve seen a teenager in [the] hospital getting their second heart valve replacement because they continue to inject after the first one.” The pill that nearly stopped the patient’s heart was one of the tens of thousands of hydromorphone tablets handed out daily via Canadian safe supply programs.
Her experiences are consistent with preliminary data from a scientific paper published by JAMA Internal Medicine in January, which found that safe supply distribution in British Columbia is associated with a “substantial” increase in opioid-related hospitalizations, rising by 63% over the first two years of program implementation — all without reducing deaths by a statistically significant margin.
While Dr. Regenstreif has worked in a variety of settings, from Ontario’s youth correctional system to Indigenous healing facilities in the Northwest Territories, her experiences in Australia, where she worked during a sabbatical year from 2013 to 2014, were particularly educational.
Australia has far fewer opioid-related deaths than Canada – in 2021, opioid mortality rates were 3.8 per 100,000 in Australia and 21 per 100,000 in Canada (a difference of over 500%). Dr. Regenstreif credited this difference to Australia’s comparatively controlled opioid landscape, where access to pharmaceutical narcotics is tightly regulated.
“Heroin had been a long-standing street opioid. It was really the only opioid you tended to see, because the only other ones people could get a prescription for were over-the-counter, low-potency codeine tablets,” she said. To this day, opioid prescriptions in Australia require special approval for repeat supplies, preventing stockpiling and street diversion.
No real evidence supports “safer supply”
Critics and whistleblowers have argued that Canadian safe supply programs, which have received over $100 million in federal funding through Health Canada’s Substance Use and Addictions Program (SUAP), were initiated without adhering to the rigorous evidentiary standards typically required to classify medication as “safe.”
Dr. Regenstreif shares these concerns and says that no credible studies show that safer supply saves lives, and that little effort is invested into exploring its possible risks and unintended consequences – such as increased addiction, hospitalization, overdose and illicit diversion to youth and vulnerable individuals.
Most studies which support the experiment simply interview recipients of safer supply and then present their answers as objective evidence of success. Dr. Regenstreif criticized these qualitative studies as methodologically flawed “customer satisfaction surveys,” as they are “very selective” and rely on small, bias-prone samples.
“If you have 400 people in a program, and you get feedback from 12, and 90% of those 12 said X, that’s not [adequate] data,” said Dr. Regenstreif, criticizing the lack of follow-up often shown safer supply researchers. “Nobody seems to track down the […] people who were not included. Did they get kicked out of the program? [Did they engage in] diversion? Did they die? We’re not hearing about that. It doesn’t make any sense in an empirical scientific universe.”
Safe supply advocates typically argue that opioids themselves are not problematic, but rather their unregulated and illicit supply, as this allows for contaminants and unpredictable dosing. However, studies have found that opioid-related deaths rise when narcotics, legal or not, are more widely available.
Dr. Regensteif is calling upon harm reduction researchers to build a more robust evidence base before calling for the expansion of safer supply. That includes more methodologically rigorous and transparent quantitative research to evaluate the full impact of Canada’s harm reduction strategies. Forgoing this evidence or adequate risk-prevention measures could lead to consequences as catastrophic as those resulting from Purdue’s deceptive marketing of OxyContin, she said.
Subscribe to our newsletter to get our latest news and analysis – or donate to our investigative journalism fund.
Critics propose solutions despite bullying
Dr. Regenstreif has faced pressure and exclusion for speaking out against safe supply. She estimates that while only a quarter of her local colleagues shared her doubts a few years ago, “now I would say more than half” harbor the same concerns. However, many are reluctant to voice their reservations publicly, fearing professional or social repercussions. “People who don’t want to speak out don’t want to be labeled as right-wing […] they don’t want to be labeled as conservative.”
While she acknowledges that safe supply may play a limited role for a small subset of patients, she believes it has been oversold as a panacea without adequate safeguards or due evaluation. “It doesn’t seem as if policymakers are listening to the people on the ground who have experience in doing this,” she said.
She contends that the solution to Canada’s addiction crisis lies in a more holistic, recovery-oriented approach that includes all four pillars of addiction: harm reduction, prevention, treatment, and enforcement. Her vision includes a national network of publicly-funded, rapid-access addiction medicine clinics with integrated counseling and wraparound services.
Additionally, Dr. Regenstreif stresses the importance of building upon established opioid agonist treatments (OAT), like methadone and buprenorphine, rather than solely relying on novel approaches whose social and medical risks are not yet fully understood.
At the core of Dr. Regenstreif’s advocacy lies a profound dedication to her patients and to the science of addiction medicine. “I like to think I kind of am fear-mongering with my patients, [by] trying to make them afraid of not getting better,” she explains. “I don’t want them to end up in the hospital and not come back out. I don’t want them to end up dead.”
[This article has been co-published with The Bureau, a Canadian media outlet that tackles corruption and foreign influence campaigns through investigative journalism. Subscribe to their work to get the latest updates on how organized crime influences the Canadian drug trade.]
Addictions
Alberta and opioids III: You can’t always just stop

Monty Ghosh at Highlevel Diner, May 30. Photo: Paul Wells
By Paul Wells

This is the concluding installment in a series on drugs in Alberta. Previously:
i. “Worse Than I’ve Ever Seen,” June 4
ii. “Alberta’s System Builder,” June 7
To support ambitious reporting on important issues, please consider a paid subscription:
A matter of expectations
Street family
My tour guide for much of my visit to Edmonton was Dr. Monty Ghosh, a clinician who’s on faculty at the University of Calgary and the University of Edmonton. He seems to talk to everybody who works with substance users in Alberta, from his own patients to front-line clinicians to the Alberta government. His relations with the latter go up and down, but he urged me to talk to Marshall Smith, the chief of staff to premier Danielle Smith.
On my first night in Edmonton Ghosh walked me around a neighbourhood that included the George Spady Society supervised-consumption site, the Hope Mission’s Herb Jamieson Centre, and the Royal Alexandra Hospital, which has a supervised-consumption service on its premises.
A lot of people use the services these places provide. Other people don’t. Shelters in particular are tricky: they’re usually for single people who arrive alone. “The Hope, the Herb, the Navigation Centre, offering the world,” one Edmonton Police Service officer told me. “But all these places have one thing in common: rules.” If you have a spouse or a pet, you want to keep your drug supply or you want to stay close to your “street family” — the community spirit in neighbourhoods like this is striking, and might be surprising to people who prefer to stay away — a shelter’s probably not for you.
Several of the places we visited weren’t ready to welcome us when we showed up unannounced. To say the least, they’re busy. That was the case at Radius Community Health and Healing, an institutional building in a more residential part of the neighbourhood. Radius is a drop-in clinic and, as we’ll see, quite a bit more.
On a sunny weekday afternoon, more than a dozen people stood, sat or lay on the building’s front steps and truncated lawn. One lay on his back, shirtless, not moving visibly. Ghosh asked the man whether he was all right, asked again, finally nudged him. The man stirred, looked around. Ghosh apologized mildly for bothering him, then checked in on two other people who also weren’t moving. They turned out to be all right too.
Francesco Mosaico, Radius’s medical director, was on his way home for the day when we arrived, but we made plans to talk the next day. When I returned, I met Mosaico and Radius’s executive director, Tricia Smith, in her office.
I think it’s important to hear them out, because when drug use becomes the object of political debate, it’s natural to talk as though policy decisions are the main thing keeping people from getting well. This can lead to a lot of blame on one hand, and to excessive optimism on the other. In fact the biggest thing that keeps people from getting well is often the entire sum of their lives until now, compounded by the influence of drugs that are more potent than anything earlier generations had to deal with.
The most complex patients
Radius offers primary care to people “experiencing multiple barriers,” Smith said. That can include homelessness, addiction, severe mental health problems, criminal records. The centre’s team includes 12 family physicians and three psychiatrists. They currently see about 3,000 patients.
Radius has Western Canada’s only non-profit dental clinic. The centre runs a respite program for people who are not sick enough to be in acute care but are too sick to be managing independently on their own. It has a program for pregnant women experiencing homelessness. It runs on a harm-reduction model, so they don’t need to be drug-free to go into the program. It has an interdisciplinary Assertive Community Treatment team to help people with mental-health and substance problems find and stay in market apartments, with frequent assistance. There’s a supervised consumption site in the basement.
“In fact,” Smith said, “we actually have an exemption from the College of Physicians and Surgeons of Alberta to filter out and keep the most complex patients. The least complex, we refer elsewhere.” I couldn’t get care in Radius if I tried; they’d politely refer me elsewhere. They’re for the people who need the most help.
After my visit, Smith wrote to me to add another program to the list: Kindred House, which for more than 25 yearss has supported women and Trans women sex workers. “The women we see are from age 18 to 50, predominantly Indigenous, have intergenerational trauma, past/current trauma, substance use issues, often houseless or couch surfing,” Smith wrote.
Smith has been at Radius for three and a half years. While I was there, I asked her how work at Radius is going. “It’s going fabulously, honestly,” she said. She arrived early in the COVID pandemic, after eight years in Alberta government departments — which in turn followed 20 years as a Canadian Forces army nurse, including in combat zones. “I’m in the right place,” she said of Radius. “It felt like coming home.”
How come? “The staff, the team, the work, the dedication. It just feels like family. I missed that. Being in the military was a big thing. This work that this group does is just really amazing. The team is amazing and it’s hard, but it’s good work.”
And how’s the workload evolving? “Unfortunately, for this population, the struggles are only increasing, and the number of individuals that are experiencing those challenges is not getting less,” she said. “The workload isn’t going anywhere. It’s getting more difficult.”
Paul Wells is a reader-supported publication. To receive new posts and support my work, consider becoming a free or paid subscriber.
“Especially in the last couple years, I don’t think things have ever been worse for the vulnerable population,” Mosaico, Radius’s medical director, added. The same housing crunch that has made homes less affordable for everyone has put thousands of the most vulnerable on the street. Results: more frequent frostbite or burns from lamps lit to keep from freezing. Body lice. Trauma from watching friends die. And to Mosaico’s astonishment, frequent shigella outbreaks.
“Shigella’s a bacteria that causes torrential bloody diarrhea. It can be treated with a single dose of antibiotics. But if you’re homeless and you don’t have a place to take care of yourself… 70 percent of the cases have had to be hospitalized in the last two years…. I mean, they’re talking about potentially calling it an endemic disease, and it’s a disease of destitution. You see it in refugee camps in developing countries, not in the capital of Alberta, you know?”
Ten thousand times deadlier
Radius also works closely with the Alberta government to integrate its services with the “recovery-oriented system of care” that I told you about last week. There are two Radius staffers working at the Integrated Care Centre the police set up to replace the old, passive holding cells for overnight detention. There are two more at the Navigation Centre, which steers people toward social and government services. If there’s an Alberta model, they’re part of it. So I was fascinated by the response when I asked my hosts the basic question that sent me to Alberta: Why are so many people dying?
“I think it’s the nature of the drugs,” Mosaico said. “You know, people used to overdose and die. But I’ve been here 17 years. I think in the first 10 or 11 years it wasn’t very common to hear about overdoses by opioids. Every once in a while you’d hear about it, but it wasn’t a daily thing. Whereas now with fentanyl and carfentanil, it’s really dangerous.”
Carfentanil is 10,000 times more potent than morphine, 100 times more than fentanyl. The Edmonton Police won’t return stolen cars they recover until they’ve scrubbed them thoroughly, because even trace amounts of these drugs are too dangerous. “We’re finding clients who use methamphetamines and swear up and down they’re not taking opioids,” Mosaico said. “And then we do urine tests and it’s there. We think their dealers are lacing methamphetamine with fentanyl because it increases the addiction.”
The other big thing on his mind, Mosaico said, is that any program to guide users into recovery will bump up against the fact that different people have often lived starkly different lives.
93% 4+
“I don’t know if you’re familiar with Adverse Childhood Experiences — the ACEs study,” Mosaico said. I was, barely, but I needed a refresher.
The original study began in 1985 in San Diego, under Vincent Felitti, who ran an obesity clinic, and Rob Anda from the Centres for Disease Control. (If you want to learn more about the study, this article and this speech on Youtube are good places to start.)
“They surveyed 17,000 people,” Mosaico said. “They found, you know, if people had developmental trauma — so, trauma between the ages of 0 and 18 — and there are 10 different forms of trauma that the study bore out as being detrimental. Things like physical, emotional, sexual abuse; physical, emotional neglect; substance use in the family; untreated mental illness in the family; separation from biological parents; maternal figure being treated violently; and a household member going to jail.
“If those things occurred, you would just tally up the number of types of trauma and you’d get a score out of 10. What they found was, if you scored four or greater, that there seem to be adverse health effects in adulthood. And it wasn’t just the presence of addictions or mental illness. It was lung disease, heart disease, liver disease, certain forms of cancer, diabetes, obesity.” This is almost folk wisdom today, but at the time, Felitti and Anda were amazed at the strength of the correlations between childhood trauma and adult physical and mental health.
The original test has been widely replicated, and it usually finds that the proportion of people in a sample who’ve had four or more adverse childhood experiences is about 12%. So something like every eighth person you meet had a really difficult childhood, and while you can’t predict for individuals from statistical trends, there’s a good chance they’re still living with the fallout.
The team at Radius surveyed a large sample of the population under their care. The prevalence of high-risk ACE scores was about 93 percent, compared to 12 in the general population,” Mosaico said.
“Harvard has a center on the developing child, which has pulled together a lot of the science that explains the neurobiological link between the adverse trauma and the adverse health effects. They talk about limitations in the development of executive function, of decision-making, emotional regulation. Impulse control is underdeveloped, neuroanatomically in the brain. And instead what over-develops is the fight-or-flight response.
“So you’re dealing with a population that, because of their experiences, isn’t the same as the general population . And then that’s compounded by the fact that a high percentage of those clients who have high ACE scores also have traumatic brain injuries from living rough on the street. They also have adult trauma that compounds the childhood trauma. They have [fetal alcohol spectrum disorder], which impairs executive function even further.
“I hear these success stories and I think they’re wonderful, when you hear about people who have a difficult life and then they straighten up. And then, you know, they go back to their jobs and their families and they become leaders in their communities. But this is a population which is over-represented in every aspect of society, negatively as it were. In the prisons and child family welfare services. In the health system, you know, prevalence of HIV, tuberculosis, Hepatitis C, STIs, all that.
“And you look at them and you think, even if they managed to wait, you know, six months to get into an addiction recovery bed, after waiting for weeks to get into detox and they go through the program, what do they go back to? Most of them had to drop out of school. They have criminal records, which makes it hard to get a job. They’re disconnected and estranged from their families. They haven’t learned social skills.
“I had a client who lived in dumpsters for two and a half years. The fact that he just stayed housed — on income support — for the rest of his life was a huge win, right? It was important for his dignity, his quality of life. It’s just a matter of adjusting your expectations of what might actually be realistic.”
Thank you for reading Paul Wells. This post is public so feel free to share it.
Dr. Larson writes
The idea for these stories goes back to February, when it first became clear to me that 2023 would be Alberta’s worst year for overdose fatalities. I asked the communications team at the University of Calgary for names of people to talk to. Many weeks went by, because sometimes it’s ridiculous how hard it is to extract myself from Ottawa routine. After I published the second article in this series, the one where Marshall Smith showed me all the stuff Alberta is building, I received an email from Dr. Bonnie R. Larson, who’s on faculty at the University of Calgary. She thought I should have talked to her, and she thought I was too credulous in reporting the Alberta government’s side. I asked if I could publish part of her email. Here it is.
What cannot be taken for granted is Mr. Smith’s view that his goals are different, somehow nobler, than those of us on the front line. Smith paints a picture that front line providers’ priorities are at odds with his own. His perspective is at once undemocratic, insulting, and arrogant, belittling those who are doing the hard work of keeping people alive every day.
I will not have Smith speak for me in his suggestion that front liners lack system knowledge and that is why we support harm reduction. This ignores the excellent evidence supporting harm reduction interventions at the population level. Smith seems to think he knows from whence I “enter this conversation”. If so, why does he not engage me and my expert colleagues? Where I “enter this conversation” is at 20 years of working with the affected community and 13 years of post-secondary education. The only reason I am what Smith likes to dismiss as a “radical harm reduction activist”, is because the UCP, immediately upon taking office, set out to destroy harm reduction in Alberta. Nobody would have ever needed to fight this soul-destroying battle in the first place if Smith hadn’t put Alberta squarely on its current path of destruction. Yes, we should hope for a better tomorrow but that doesn’t excuse ignoring the past and present.
I would ask you to think about several additional factors that your analysis appears to ignore, including who actually benefits, in power and wealth, from Smiths’ system of so-called care? DId you consider the other ways that the UCP policy direction is moving the entire publicly-funded system steadily towards profit? Gunn (McCullough Centre) was a wonderful non-profit facility that helped many of my patients find their way to recovery from substance use disorders. While I agree that people should not have to pay for treatment, the question remains: in whose pockets do those tax dollars ultimately land?
You report that Smith indicates that they are “monitoring” the entire system. Where is the data from that monitoring? They have had five years now to show some outcomes, but who am I, just a lowly street doctor, to ask for population data? What I do know is that if deaths begin to decline, it is because so many are already gone. You should ask to see the data about which Smith so proudly boasts.
Smith’s entire premise that he is fixing the ‘addiction crisis’ is a fallacy. Addictions are not increasing. Deaths by drug poisonings are, however, and Smith’s circus is only making that worse. Allow me to spell it out for you: harm reduction addresses the drug poisoning crisis that is, no question, taking a horrific toll in Alberta and nationally. Smith’s ROSC, in contrast, addresses a figmentary addictions crisis.
One last tip. Medications used for opioid agonist treatment are not harm reduction, they are treatment. Nobody here is against treatment or recovery. But Marshall Smith is against harm reduction. Why can’t we just have the full spectrum of care??? Polarization is created by politicians to benefit politicians.
I don’t endorse everything Dr. Larson writes here. The data, or a lot of it, seems to me to be publicly available on the province’s impressive dashboard website. Use the tabs at the top of the page to navigate. And indeed, the story the dashboard tells is alarming, which, as I explained in this series’ first instalment, is why I flew west. But Larson’s years of front-line work has earned her, at the very least, a right of rebuttal.
Synthesis
On my last day in Edmonton, I met Monty Ghosh at Highlevel Diner, at the outer edge of the hip Strathcona neighbourhood on the south of the North Saskatchewan River. Highlevel is famous for its cinnamon buns, which, if I’m going to be honest, are noteworthy mostly for being large.
If the Alberta government and its most vociferous critics are thesis and antithesis, Ghosh tries to provide synthesis. He helped design the National Overdose Response Service, or NORS, which provides some of the emergency-response capability supervised consumption sites offer to people who aren’t near such a site or can’t use it for other reasons. He’s been critical of the Alberta government, but both sides keep lines of communication open.
I asked him about diverted safe supply — the idea that pharmaceutical opioids used in safe-supply programs in BC, principally hydromorphone tablets, are being sold or distributed away from their intended use. “I know it happens,” Ghosh said. “We sometimes get clients from British Columbia who come to Alberta to try to escape BC, because they’re looking for a fresh start. They’re looking for support and they’ll tell me themselves that they’ve diverted their safe supply.”
But what are the quantities? Trivial so far, Ghosh maintains. “Have I seen hydromorphone come into our province? Not at all, not yet.” This is the same thing I heard from Warren Driechel, the Edmonton deputy police chief.
Why do people divert their prescribed safe supply anyway? The answer Ghosh gave me was the answer I heard from everyone I asked. “They never used it. It just was not effective. The potency of the hydromorphone that they’re getting was nowhere near touching the fentanyl that they were using. It wasn’t dealing with the cravings, it wasn’t dealing with withdrawals, they felt it was useless. So what did they do? They sold it. They’re incredibly poor, they cannot afford their substance-use concerns and so therefore they supplement with revenue from hydromorphone.”
Before I flew to Edmonton, when Ghosh and I were trying to gauge on the phone what each of us thought of this infernal crisis, he figured out that I was interested in the differences between government policy in British Columbia and Alberta. “I’m not sure you want to hear this,” he said, “but I think it’s going to be bad everywhere.” I said that’s what I think too. Perhaps I surprised him.
I don’t know what happens next. Maybe things just stop getting worse everywhere on their own, for big complex reasons that resist easy analysis. Overdose deaths were lower last year in the United States, the capital of this hellscape, than the year before.
If not… well, we shall see. I wonder what happens in year six or seven of the effort the Alberta government is building. Is there resentment among people in ordinary hospitals and correctional facilities, who don’t have access to bespoke programs and personal attention? Does the ROSC system become bureaucratized after the first generation of administrators moves on?
Or does it start to win converts? David Eby, the NDP premier of British Columbia, has started putting distance between himself and his public-health advisors on legalization and safe supply. A new appointment in BC is being closely watched in Edmonton.
Or, conversely, does the Alberta recovery effort bump up against the limits imposed by the substances involved and by human nature? Reported recovery rates from addiction vary widely, depending in part on how you measure them. This paper puts the rate at less than 30%. If you even manage to double it, that still leaves a large cohort who aren’t getting better. Would their neighbours see them as people who “failed recovery” or “blew their chance?”
I won’t claim to know. I do hope that in the year ahead, more Canadians check their assumptions and stow their cheap certainties. Especially those who aspire to positions of leadership.
For the full experience subscribe to Paul Wells.
-

 COVID-1913 hours ago
COVID-1913 hours agoFederal court rules COVID shots don’t stop transmission of virus, sides with anti-mandate lawsuit
-

 Red Deer8 hours ago
Red Deer8 hours agoRed Deer Symphony Orchestra invites you to the 2024-2025 season!
-
 Crime12 hours ago
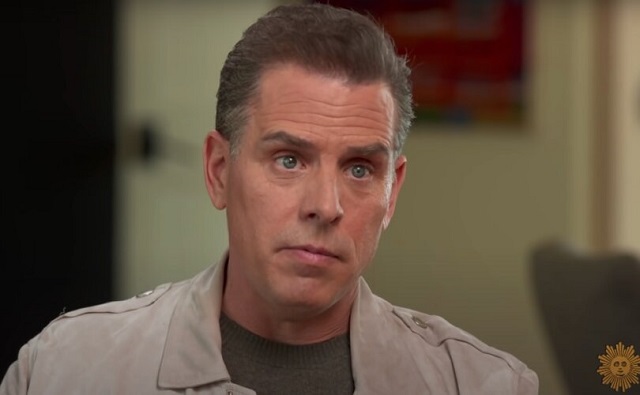
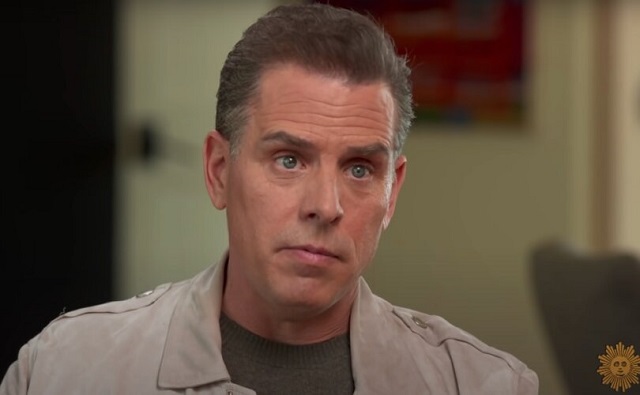
Crime12 hours agoFBI admits identity of Hunter Biden laptop in Delaware trial after intelligence officials denied story in 2020
-
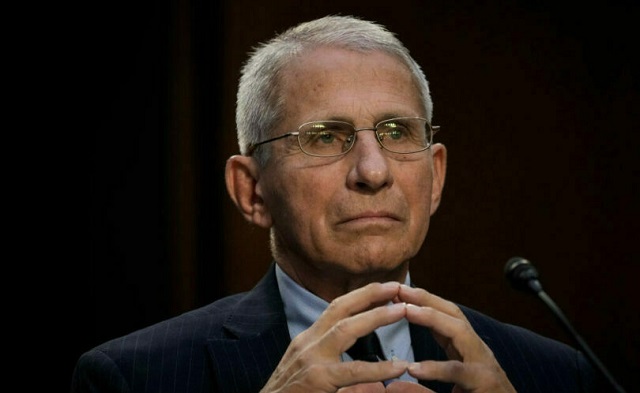
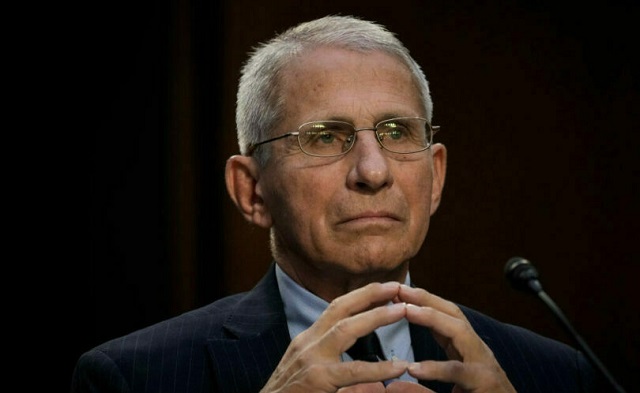 COVID-195 hours ago
COVID-195 hours agoCivil liberties group demands Fauci preserve records with Big Tech for COVID collusion lawsuit
-

 Frontier Centre for Public Policy10 hours ago
Frontier Centre for Public Policy10 hours agoTrump’s trial defines justice in disrepute – A Canadian perspective
-

 Addictions8 hours ago
Addictions8 hours ago“Safer supply” reminiscent of the OxyContin crisis, warns addiction physician
-

 International1 day ago
International1 day agoWilliam ‘Lia’ Thomas loses challenge to rule banning him from women’s Olympic contests
-

 Economy1 day ago
Economy1 day agoOttawa should abandon unfeasible and damaging ‘net-zero’ plan


