Fraser Institute
Ignore climate-obsessed propagandists and enjoy your summer

From the Fraser Institute
Ah summer, a season we used to meet with joy. Outdoor parties, leisurely road trips, weekends at the beach, blazing barbecues by day, blazing bonfires by night. We used to sing paeans to the season—“Summertime, and the living is easy, fish are jumping and the cotton is high.”
But a strange thing has happened—the climate-obsessed folks have seized upon summer as a primary propaganda source and use it to demonize activities that might produce greenhouse gases. They don’t want your living to be easy. They want your coal or gas barbecues gone, your road trips gone, your air conditioning coolant weakened or gone, and so on. And every heatwave, every forest fire, every hint of drought, every reported case of heatstroke, and even observations of jumping catfish will be proof of a climate crisis where extreme weather will eventually kill us all.
But in a recent study, I found that the evidence of increases in extreme weather events in Canada and around the world is spotty and of limited quality, and often contradictory of the narrative.
First, what about wildfires? The United Nations Intergovernmental Panel on Climate Change (IPCC), in its latest climate report, only assigns “medium confidence” to the idea that climate change has actually caused increased “fire weather” in some regions on Earth.
Here at home, as average atmospheric temperatures have risen from 1970 to 2017, Canadian forest fires have actually declined sharply in number and show little obvious trend in areas burnt. As economist/professor Ross McKitrick observes: “Canadian forest fire data are available from the Wildland Fire Information System. Wildfires have been getting less frequent in Canada over the past 30 years. The annual number of fires grew from 1959 to 1990, peaking in 1989 at just over 12,000 that year, and has been trending down since. From 2017 to 2021 (the most recent interval available), there were about 5,500 fires per year, half the average from 1987 to 1991. The annual area burned also peaked 30 years ago. It grew from 1959 to 1990, peaking in 1989 at 7.6 million hectares before declining to the current average of 2.4 million hectares per year over 2017-21. And 2020 marked the lowest point on record with only 760,000 hectares burned.”
Well, but what about drought? According to an international research team, “In the vast majority of the world, trends in meteorological drought duration and magnitude are not statistically significant, with the exception of some small regions of Africa and South America, which is also where data uncertainty is greater.” The International Energy Agency (IEA) in a 2021 report suggests that drought severity in Canada from 2000 to 2020 was only slightly above the global average.
Well, but what about floods? The IPCC says floods have likely increased globally since 1950, but in Canada, at least, “there is a lack of detectable trends in observed annual maximum daily (or shorter duration) precipitation.”
So, summertime and the living is easy. Ignore the shrieks of the climate-obsessed about extreme weather coming for us all, and have some fun in the sun.
Author:
Business
Taxpayers paying wages and benefits for 30% of all jobs created over the last 10 years
From the Fraser Institute
By Jason Childs
From 2015 to 2024, the government sector in Canada—including federal, provincial and municipal—added 950,000 jobs, which accounted for roughly 30 per cent of total employment growth in the country, finds a new study published today by the Fraser Institute, an independent, non-partisan Canadian public policy think-tank.
“In Canada, employment in the government sector has skyrocketed over the last 10 years,” said Jason Childs, a professor of economics at the University of Regina, senior fellow at the Fraser Institute and author of Examining the Growth of Public-Sector Employment Since 2015.
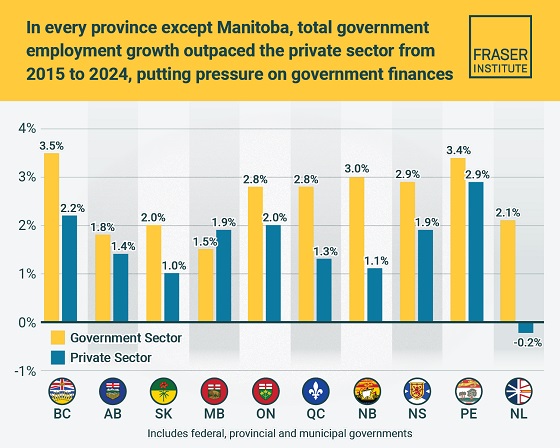
Over the same 10-year period (2015-2024), government-sector employment grew at an annual average rate of 2.7 per cent compared to only 1.7 per cent for the private sector. The study also examines employment growth by province. Government employment (federal, provincial, municipal) grew at a higher annual rate than the private sector in every province except Manitoba over the 10-year period.
The largest gaps between government-sector employment growth compared to the private sector were in Newfoundland and Labrador, New Brunswick, Quebec and British Columbia. The smallest gaps were in Alberta and Prince Edward Island.
“The larger government’s share of employment, the greater the ultimate burden on taxpayers to support government workers—government does not pay for itself,” Childs said.
A related study (Measuring the Cost to Canadians from the Growth in Public Administration, also authored by Childs) finds that, from 2015 to 2024, across all levels of government in Canada, the number of public administrators (many of who
work in government ministries, agencies and other offices that do not directly provide services to the public) grew by more than 328,000—or 3.5 per cent annually (on average).
“If governments want to reduce costs, they should look closely at the size of their public administration,” Childs said.
Examining the Growth of Public Sector Employment Since 2015
Business
US Supreme Court may end ‘emergency’ tariffs, but that won’t stop the President

From the Fraser Institute
By Scott Lincicome
The U.S. Supreme Court will soon decide the fate of the global tariffs President Donald J. Trump has imposed under the International Emergency Powers Act (IEEPA). A court decision invalidating the tariffs is widely expected—hovering around 75 per cent on various betting markets—and would be welcome news for American importers, the United States economy and the rule of law. Even without IEEPA, however, other U.S. laws all but ensure that much higher tariffs will remain the norm. Realizing that protection will just take a little longer and, perhaps, be a little more predictable.
As my Cato Institute colleague Clark Packard and I wrote last year, the Constitution grants Congress the power to impose tariffs, but the legislative branch during the 20th century delegated much of that authority to the president under the assumption that he would be the least likely to abuse it. Thus, U.S. trade law is today littered with provisions granting the president broad powers to impose tariffs for various reasons. No IEEPA needed.
This includes laws that Trump has already invoked. Today, for example, we have “Section 301” tariffs of up to 25 per cent on around half of all Chinese imports, due to alleged “unfair trade” practices by Beijing. We also have global “Section 232” tariffs of up to 50 per cent on imports of steel and aluminum, automotive goods, heavy-duty trucks, copper and wood products—each imposed on the grounds that these goods threaten U.S. national security. The Trump administration also has created a process whereby “derivative” products made from goods subject to Section 232 tariffs will be covered by those same tariffs. Several other Section 232 investigations—on semiconductors, pharmaceuticals, critical minerals, commercial aircraft, and more—were also initiated earlier this year, setting the stage for more U.S. tariffs in the weeks ahead.
Trump administration officials admit that they’ve been studying these and other laws as fallback options if the Supreme Court invalidates the IEEPA tariffs. Their toolkit reportedly includes completing the actions above, initiating new investigations under Section 301 (targeting specific countries) and Section 232 (targeting certain products), and imposing tariffs under other laws that have not yet been invoked. Most notably, there’s strong administration interest in Section 122 of the Trade Act of 1974, which empowers the president to address “large and serious” balance-of-payments deficits via global tariffs of up to 15 per cent for no more than 150 days (after which Congress must act to continue the tariffs). The administration might also consider Section 338 of the Tariff Act of 1930—a short and ambiguous law that authorizes the president to impose tariffs of up to 50 per cent on imports from countries that have “discriminated” against U.S. commerce—but this is riskier because the law may have been superseded by Section 301.
We should expect the administration to move quickly to use these measures to reverse engineer Trump’s global tariff regime under IEEPA. The main difference would be in how he does so. IEEPA was essentially a tariff switch in the Oval Office that could be flipped on and off instantly, creating massive uncertainty for businesses, foreign governments and the U.S. economy. The alternative authorities, by contrast, all have substantive and procedural guardrails that limit their size and scope, or, at the very least, give American and foreign companies time to prepare for forthcoming tariffs (or lobby against them).
Section 301, for example, requires an investigation of a foreign country’s trade and economic policies—cases that typically take nine months and involve public hearings and formal findings. Section 232 requires an investigation into and a report on whether imports threaten national security—actions that also typically take months. Section 122 has fewer procedures, but its limited duration and 15 per cent cap make it far less dangerous than IEEPA, under which Trump has repeatedly threatened tariffs of 100 per cent or more.
Of course, “procedural guardrails” is a relative term for an administration that has already stretched Section 232’s “national security” rationale to cover bathroom vanities. The courts also have largely rubber-stamped the administration’s previous moves under Section 232 and Section 301—a big reason why we should expect the Trump administration’s tariff “Plan B” to feature them.
Thus, a court ruling against the IEEPA tariffs would be an important victory for constitutional governance and would eliminate the most destabilizing element of Trump’s tariff regime. But until the U.S. Congress reclaims some of its constitutional authority over U.S. trade policy, high and costly tariffs will remain.
-

 Alberta2 days ago
Alberta2 days agoAlberta to protect three pro-family laws by invoking notwithstanding clause
-

 Artificial Intelligence2 days ago
Artificial Intelligence2 days agoLawsuit Claims Google Secretly Used Gemini AI to Scan Private Gmail and Chat Data
-

 Health2 days ago
Health2 days agoCDC’s Autism Reversal: Inside the Collapse of a 25‑Year Public Health Narrative
-

 Business2 days ago
Business2 days agoCanada is failing dismally at our climate goals. We’re also ruining our economy.
-

 Crime2 days ago
Crime2 days ago‘Modern-Day Escobar’: U.S. Says Former Canadian Olympian Ran Cocaine Pipeline with Cartel Protection and a Corrupt Toronto Lawyer
-

 Crime1 day ago
Crime1 day agoCocaine, Manhunts, and Murder: Canadian Cartel Kingpin Prosecuted In US
-

 Health1 day ago
Health1 day agoBREAKING: CDC quietly rewrites its vaccine–autism guidance
-

 Alberta20 hours ago
Alberta20 hours agoPremier Smith explains how private clinics will be introduced in Alberta








