Health
Hospital wants to pull the plug on inhumanely neglected 23-year-old woman who is not brain dead

From LifeSiteNews
Montefiore Hospital in Brooklyn is neglecting Amber Ebanks, but experts who have seen the student say her body is functioning and that she could improve with proper treatment.
Amber Ebanks, a 23-year-old Jamaican business student, drove herself to Montefiore Hospital in the Bronx for elective surgery on July 30. But her procedure went awry, leading to an intraoperative stroke and brain swelling that worsened over time. Now, her family is fighting for Amber’s life while the hospital wants to pull the plug.
In February, Amber was found to have a ruptured arteriovenous malformation (AVM), a tangle of abnormal arteries and veins in her brain. Thankfully, after the rupture she was able to return to life as normal. Her doctors recommended that she undergo an embolization procedure to clot off the abnormal blood vessels in her brain in hopes of preventing further rupturing and brain damage. Unfortunately, during the embolization procedure, one of the major arteries supplying blood to Amber’s brain was unintentionally occluded, and her procedure was also complicated by a type of bleeding around the brain called a subarachnoid hemorrhage. Thus, she was taken to the ICU, placed in a medically induced coma, and treated for brain swelling.
Just 10 days later, on August 9, her doctors declared her to be “brain dead.” But there were problems with this diagnosis. The Determination of Death statute in New York and the Uniform Determination of Death Act (UDDA) both state:
“An individual who has sustained either:
- irreversible cessation of circulatory and respiratory functions; or
- irreversible cessation of all functions of the entire brain, including the brain stem, is dead.”
Amber Ebanks meets neither the first nor the second of these criteria. Her circulatory and respiratory functions continue: her heart is still beating, and her lungs are absorbing oxygen and releasing carbon dioxide. And she does not have the irreversible cessation of all functions of her brain, since she is maintaining her own body temperature, which is a brain function.
Moreover, the new 2023 American Academy of Neurology brain death guideline indicates that metabolic derangements such as high serum sodium levels may confound a brain death evaluation. According to Dr. Paul Byrne, Amber’s sodium levels were very high prior to her brain death determination, with readings over 160meq/L (normal sodium levels range from 135-145 meq/L). Not only can high sodium levels cause abnormal brain functioning, but they can also cause blood vessels in the brain to rupture, causing more brain bleeding – the very problems that Amber’s doctors should be interested in preventing. Also, even though high levels of carbon dioxide are known to exacerbate brain swelling, her doctors have not been checking these levels or adjusting her ventilator settings to prevent such derangements.
In addition to her ongoing heart, lung, and brain functions, Amber has continuing liver and kidney function. And presumably she still has digestive function, even though the hospital has been refusing to feed her since she came in for her surgery on July 30th. A patient cannot be expected to improve neurologically without nutrition.
Not only is Montefiore Hospital refusing to feed Amber, it’s refusing to provide her with basic wound care and hygiene. When Dr. Byrne, a board-certified pediatrician and neonatologist and brain death expert, flew to New York to see Amber this past week, Amber’s sister Kay showed him a maggot she had removed from her sister’s hair. Referring to hospital personnel, Kay Ebanks said in an ABC News article, “They are some of the cruelest people I have ever known.” Most of Amber’s family lives in Jamaica, and her father has been struggling to get a visa in order to come and see his daughter. Meanwhile, the hospital actually suggested that family members say goodbye to her over the phone.
Dr. Byrne and Dr. Thomas M. Zabiega, a board-certified psychiatrist and neurologist, have both evaluated Amber’s case. They have submitted sworn affidavits that Amber Ebanks is alive, and believe that she has decreased blood flow to her brain causing a quietness of the brain known as Global Ischemic Penumbra (GIP). During GIP, the brain shuts down its function to save energy, but the brain tissue itself remains viable. Drs. Byrne and Zabiega recommend additional time and treatment such as adjusting Amber’s sodium and carbon dioxide levels and treating hormonal deficiencies. They have testified that with proper medical treatments she is likely to continue to live and may obtain limited to full recovery of brain functions, even possibly recovering consciousness.
And there are other health care professionals who are willing to help Amber heal. A long-term care facility on Long Island called New Beginnings has agreed to care for Ebanks for as long as her family would like. “Everybody needs hope. You can’t just give up. Can’t just take them off life support when she needs more time,” New Beginnings founder Allyson Scerri said.
Nevertheless, doctors at Montefiore Hospital are adamant that Amber is “brain dead” and want to disconnect her from her ventilator over the objections of her family. Despite the testimony of qualified doctors and experts, the judge assigned to her case is requiring that a New York-licensed physician be found to evaluate Amber and give testimony about her condition. Until then, Amber remains unfed, uncared for, and neglected in an American hospital, to the point of her sister having to remove vermin from her hair.
Amber Ebanks is very much alive despite receiving little to no ongoing treatment to assist with the healing of her brain. She does not meet the medical or legal criteria for death. All she needs are proper ventilator therapy, a balancing of her fluids and electrolytes, nutrition via a feeding tube, and hormonal replacement: treatments that are commonplace in medicine today. It is shameful that her family has had to beg for these treatments and even go to court to try to force the hospital to provide them.
Heidi Klessig, MD is a retired anesthesiologist and pain management specialist who writes and speaks on the ethics of organ harvesting and transplantation. She is the author of “The Brain Death Fallacy” and her work may be found at respectforhumanlife.com.
Health
Organ donation industry’s redefinitions of death threaten living people

From LifeSiteNews
Playing fast and loose with the definitions of death for the sake of organ donation must stop.
Another congressional committee is investigating more whistleblowers’ complaints regarding the organ transplantation industry. United States House Ways and Means Committee Chairman Jason Smith and Oversight Subcommittee Chairman David Schweikert are seeking answers from Carolyn Welsh, president and CEO of the New Jersey Organ and Tissue Sharing Network (NJTO), regarding multiple allegations of legal and ethical violations on her watch.
The complaints include the horrific case of a “circulatory death” organ donor who reanimated prior to organ retrieval. Despite the fact that the patient had regained signs of life, NJTO executives actually directed frontline staff to continue the organ recovery process. (Thankfully, hospital personnel at Virtua Our Lady of Lourdes Hospital in Camden, New Jersey, refused this request.) NJTO is also accused of pressuring the families of potential donors by falsely implying the New Jersey Department of Motor Vehicles had registered a consent to donate when that was not known to be the case. NJTO apparently also continued to insist that people were registered donors even after they had removed their consent to donate from their driver’s licenses. The official complaint further states that NJTO allegedly tried to delete evidence pertaining to the committee’s investigation.
Since 1968, when 13 men at Harvard Medical School redefined “desperately injured” people as being dead enough to become organ donors, organ procurement has continued to push the boundaries of life and death in a never-ending quest for more organs. When the first and only multicenter prospective study of brain death discovered in 1972 that a brain death diagnosis did not invariably correlate with a diffusely destroyed brain, principal investigator Dr. Gaetano Molinari pointed out that “brain death” was a prognosis of death, and not death itself. Dr. Molinari wrote:
[D]oes a fatal prognosis permit the physician to pronounce death? It is highly doubtful whether such glib euphemisms as ‘he’s practically dead,’… ‘he can’t survive,’ … ‘he has no chance of recovery anyway,’ will ever be acceptable legally or morally as a pronouncement that death has occurred.
But despite Dr. Molinari’s doubts, history shows this is exactly what has been accepted, and the rising numbers of people who have been taken for organ harvesting while still alive bears this out. Even though “brain dead” TJ Hoover III was still looking around and visibly crying such that two doctors refused to remove his organs, Kentucky Organ Donor Affiliates ordered their staff to find another doctor to perform the procedure. “Circulatory death” donor Misty Hawkins was found to have a beating heart when her breastbone was sawed open for organ procurement. And Larry Black Jr. was rescued from the operating room table just minutes before having his organs removed, and went on to make a full recovery.
Given that we have been stretching the definitions of death for nearly 60 years, is it any wonder that organ procurement personnel appear to be thinking “he’s practically dead,” “he can’t survive,” “he has no chance of recovery anyway” as they push still-living people towards the operating room?
But it’s not just organ procurement teams that are pushing these new definitions of death. Just three weeks after failing in their attempts to broaden the legal definitions of death by revising the Uniform Determination of Death Act (UDDA), the American Academy of Neurology (AAN) published a new brain death guideline that explicitly allows brain death to be declared in the presence of ongoing brain function. Since this obviously does not comply with the UDDA, which requires “the irreversible cessation of all functions of the entire brain including the brain stem,” the AAN has been trying to get around the law by contacting state health departments, medical boards, medical societies, and hospital associations requesting that they acknowledge the AAN’s brain death guideline as the “accepted medical standards” for declaring neurological death.
The AAN has also just published a position statement of additional guidance on brain death discussing how to handle objections to the brain death diagnosis. Even though the AAN’s brain death guideline does not comply with U.S. law and has been proven to be unable to predict whether or not a brain injury is irreversible, the AAN still wants to make the use of their guideline mandatory. If a family’s objection to a brain death diagnosis cannot be overcome, the AAN says that life support may be unilaterally withdrawn – over the family’s objections. The AAN also says that clinicians are professionally obligated to make a brain death determination, and that they should be credentialed to do so according to the standards of the AAN guideline. Laughably, the AAN recommends the Neurocritical Care Society’s brain death determination course, which consists of a one-hour video, followed by unlimited attempts to correctly answer 25 questions, following which a certificate of completion can be had for as little as six dollars.
The Dead Donor Rule is an ethical maxim stating that people must neither be alive when organs are removed nor killed by the process of organ removal. Redefining neurologically injured people as being “brain dead” and redefining people who could still be resuscitated as being dead according to “circulatory death” standards have for too long allowed organ procurement teams to meet the letter of the Dead Donor Rule through sleight of hand. Playing fast and loose with the definitions of death for the sake of organ donation must stop. Patients with a poor prognosis must not be considered “dead enough” to become organ donors. People registering as organ donors must be given fully informed consent as to the risks involved.
Even utilitarian philosopher Dr. Peter Singer has called brain death an ethical choice masquerading as a medical fact. Imposing mandates that force patients and doctors to accept these questionable ethical choices is NOT the best way to establish trust.
Heidi Klessig MD is a retired anesthesiologist and pain management specialist who writes and speaks on the ethics of organ donation and transplantation. She is the author of “The Brain Death Fallacy” and her work may be found at respectforhumanlife.com.
Alberta
Alberta introducing dual practice health care model to increase options and shorten wait times while promising protection for publicly funded services

Enhancing access through dual practice
If passed, Bill 11, the Health Statutes Amendment Act, 2025 (No. 2), would modernize physician participation rules to give doctors flexibility to work in both the public system and private settings. Dual practice would allow physicians to continue providing insured services through the provincial health insurance plan while also delivering private services.
Alberta’s government has looked to proven models in other jurisdictions to guide the development of a model that strengthens access while safeguarding the public system. Dual practice exists in New Brunswick and Quebec and is widely used in countries with top-performing health systems, including Denmark, the Netherlands, United Kingdom, France, Germany, Spain and Australia.
“For years, governments across Canada have tried to fix long wait times by spending more money, yet the problem keeps getting worse. Alberta will not accept the status quo. Dual practice gives us a practical, proven tool that lets surgeons do more without asking taxpayers to pay more. It means shorter waits, better outcomes and a stronger health system for everyone.”
If passed, this dual practice model would be closely monitored to protect Alberta’s public health care system. The government, for example, would ensure that dual practice physicians maintain separate records for the services they provide, so no public funding subsidizes private services.
Bill 11 would include provisions to restrict participation, which could include:
- Mandating that surgeons in dual practice must perform a dedicated number or ratio of surgeries in the public system to be eligible to perform surgeries privately.
- Restricting specialties to public practice if shortages would compromise public care.
- Potentially restricting private practice to evenings, weekends or to underutilized rural sites, as required.
Alberta’s government remains committed to its public health guarantee: No Albertan will ever have to pay out of pocket to see their family doctor or to get the medical treatment they need. These proposed changes comply with the Canada Health Act.
Alberta’s government is also committed to getting Alberta’s dual practice model right and to taking a thoughtful approach to ensure the best path forward. At this time, family medicine providers will not be eligible to be flexible participants within this new model. The priority is to focus on making sure all Albertans have access to a primary care provider. Additionally, surgeries for life-threatening conditions such as cancer and emergency procedures will remain entirely publicly funded with no private option available.
“Albertans are waiting too long for the health care they need, so we are taking bold and decisive action to shorten wait times, increase access and give Albertans more choices over their own health care. At the same time, we will continue building a strong public health system where no one is denied access to the services they need because of an inability to pay.”
If passed, Bill 11 would create new options for doctors and patients. It would expand Alberta’s health system to provide more care by allowing doctors to treat more patients. Each time a patient chooses to pay for care in a private clinic or a clinic operating on evenings and weekends, for example, resources would be freed up so another patient could receive publicly funded care. This proposed new model would also support physician attraction and retention.
“As dual practice enhances flexibility for Albertans, physicians and medical professionals, safeguards will be established and utilized to protect and grow hospital and public health system capacity.”
“Albertans deserve choice and timely access to safe care, whether in a private or public setting. With the creation of the dual practice model, we can extend treatment options to patients while helping hospitals focus their resources on the highest-acuity patients.”
“I believe all options to improve access to health care for Albertans should be on the table. Therefore, the government’s dual practice legislation is a welcome option. Appropriate guardrails must be in place to ensure the spirit of the Canada Health Act is maintained.”
Quick facts
- Physicians would continue to bill the provincial plan for public services and may offer private services separately.
- Physicians may still choose to work entirely in public or entirely in private settings.
Proposed legislation would modernize physician rules, drug coverage, food safety and health cards while improving oversight and administration in Alberta’s health system.
If passed, Bill 11, the Health Statutes Amendment Act, 2025 (No. 2), would amend several pieces of legislation to reflect Alberta’s evolving health needs, strengthen the ability of health care professionals to deliver care and improve accountability and efficiency across the system.
“This legislation represents a new era for health care in Alberta. By putting patients first and supporting providers, we are improving transparency, flexibility and access. With modernized physician rules, stronger drug coverage, enhanced food safety and better health information sharing, Albertans will have world-class care.”
Protecting drug coverage for Albertans
If passed, amendments would improve coordination between public and private drug plans, ensuring taxpayer-funded programs are used efficiently and remain available for those who need them most.
Private plans would become the first payer for individuals who have them, with public programs acting as a safety net. The legislation would also protect older Albertans by ensuring employers cannot reduce or terminate health benefits for employees aged 65 and older who remain actively employed.
“People shouldn’t be punished for getting older – it’s that straightforward. With this legislation, we’re protecting Albertans by ensuring employers can no longer kick folks off their health benefits when they need them most.”
Ensuring consistent billing and remuneration practices
Alberta’s government is also proposing amendments to the Alberta Health Care Insurance Act to ensure health care providers and clinics are not engaging in improper billing practices and making inappropriate claims. The proposed amendments would strengthen accountability and transparency while generating cost savings by introducing penalties for systemic non-compliance.
Strengthening food safety in Alberta
If passed, amendments to the Public Health Act and related regulations would strengthen food safety across all establishments by improving training for staff, increasing transparency of inspection results and giving inspectors new tools for oversight and investigation.
The changes would also update the Food Regulation, Food Retail and Food Services Code, Institutions Regulation and create a new Public Health Investigator Regulation, ensuring consistent standards, better reporting and increased public confidence in Alberta’s food safety system.
“Enhancing food safety in Alberta is an important step to making sure Albertans have the safeguards and protections in place to keep them healthy and well. If passed, these amendments to the Public Health Act will ensure food establishments are following best practices and that enforcement measures are in place to support proper food safety.”
Improving health cards and information sharing
If passed, the legislation would create a new process for health card renewal, prevent card misuse and allow cards to be seized or suspended if tampered with. The changes would also permit information sharing with the ministries of Technology and Innovation and Service Alberta and Red Tape Reduction to support continued efforts to modernize health cards.
Amendments to the Health Information Act would support a more integrated health care system and seamless patient experience to help improve care for Albertans who are accessing the system.
It would also add new authority to enable health foundations to better connect with patients to support innovation and advancement of care in their community in an appropriate manner, in accordance with the requirements set out in regulations.
“Albertans generously support enhancements to health care delivery, innovation and research in their communities each year. We look forward to working with our health partners across the continuum to better communicate with grateful patients. With these changes, we will join other Canadian jurisdictions in connecting patients with health foundations in their community while ensuring the strongest protection of Albertans’ private health data.”
Advancing a new era of health care
If passed, proposed amendments to the Alberta Health Care Insurance Act and the Provincial Health Agencies Act would support operational changes to implement previously announced objectives like transitioning Alberta Health Services to a hospital-based acute care service provider.
The proposed amendments would also result in the repealing of the Hospitals Act, as all hospital governance and operational provisions would be moved into the Provincial Health Agencies Act.
New dual practice model to increase access and choice
The Health Statutes Amendment Act, 2025 (No. 2) includes proposed amendments to the Alberta Health Care Insurance Act that would modernize how physicians participate in Alberta’s publicly funded health insurance plan. The changes would introduce a new dual practice model, giving physicians greater flexibility to provide care in both public and private settings while maintaining safeguards to ensure Albertans continue to have access to publicly funded health services.
-

 Alberta2 days ago
Alberta2 days agoRed Deer’s Jason Stephan calls for citizen-led referendum on late-term abortion ban in Alberta
-

 espionage2 days ago
espionage2 days agoSoros family has been working with State Department for 50 years, WikiLeaks shows
-

 Indigenous2 days ago
Indigenous2 days agoIndigenous activist wins landmark court ruling for financial transparency
-

 Artificial Intelligence20 hours ago
Artificial Intelligence20 hours agoGoogle denies scanning users’ email and attachments with its AI software
-

 Business1 day ago
Business1 day agoIs affirming existing, approved projects truly the best we can do in Canada?
-
 Business1 day ago
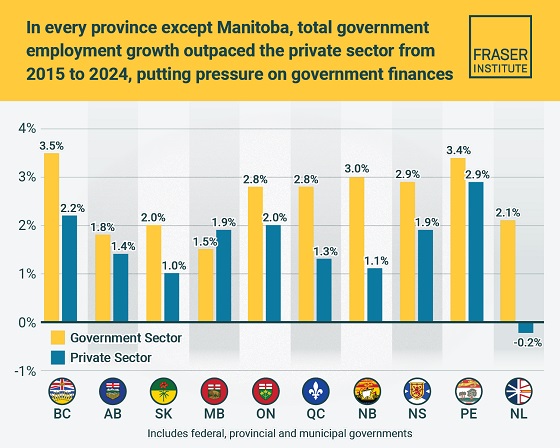
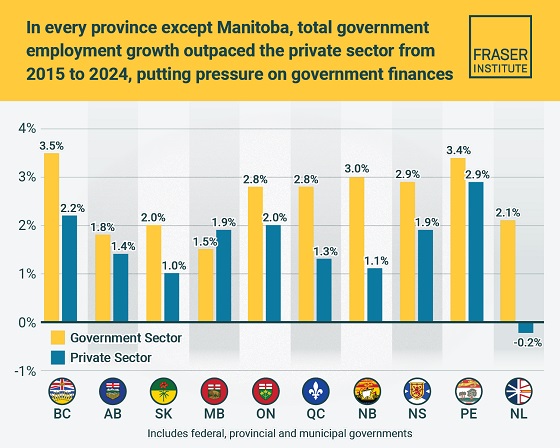
Business1 day agoTaxpayers paying wages and benefits for 30% of all jobs created over the last 10 years
-

 MAiD1 day ago
MAiD1 day agoHealth Canada suggests MAiD expansion by pre-approving ‘advance requests’
-

 International1 day ago
International1 day agoTrump closes in on peace in Ukraine






