Addictions
From opioids to office: An interview with Alberta’s new addiction minister

By Alexandra Keeler
Rick Wilson shares what led him into — and out of — addiction, his goals for Alberta’s recovery model and the value of an ‘Indigenous lens’
In mid-May, Alberta appointed Rick Wilson as the province’s new minister of mental health and addiction.
Wilson, who represents the Maskwacîs-Wetaskiwin riding south of Edmonton, was Alberta’s longest serving minister of Indigenous relations, serving from 2019 to this year.
Now, Wilson is tasked with accelerating the implementation of the Alberta Model, a recovery-oriented system of care that prioritizes addiction prevention, early intervention and treatment over harm reduction.
Canadian Affairs spoke with Wilson about his priorities in the new role, how his prior work with Indigenous communities shapes his perspective and what lies ahead for mental health and addiction care in Alberta.
AK: I understand you’ve been tasked with advancing the Alberta Recovery Model. What aspects of the model require the most focus in the term ahead?
RW: My goal is going to be to keep the momentum going. [We need to] get all the recovery communities opened up, keep expanding our supports, like CASA Classrooms [classroom-based mental health programs], and just keep filling the gaps for better information.
AK: Why was your predecessor, Dan Williams, shuffled out of the post?
It was a cascading event. Our speaker took a job in Washington, so we voted for a new speaker, Rick McIver. That left a hole in Municipal Affairs, [where Dan was moved]. I’d been bugging Premier Smith for more help with addictions and mental health. She said, ‘Go fix it then, I’ll put you there.’
AK: Do you have personal experience with mental health or addiction struggles?
RW: Do you want the whole sad story here?
I used to raise a lot of cattle and had one really rank bull that was terrorizing the farm. One morning I tried to get him up, and it didn’t end well — he got me down, fractured several vertebrae in my neck and back, and collapsed my lungs. I don’t know how I survived, but somehow I did.
For a year, I couldn’t walk. I was in so much pain I didn’t even know who I was. I would literally pray for one second of relief. Whatever the doctor gives you, you’ll take it — Oxytocin to Percocet; you name it, I was on it. My wife said she’d give me a pill and an hour later, I’d be begging her for more. This went on for close to a year.
I finally had what’s called laser spinal surgery. I was one of the very lucky ones. I went into it in a wheelchair, but I came out walking, and the pain was gone.
About a week later, I told my wife, ‘I think I’m full of infection — I’m burning up with fever, I’m sweating, and I think they’ve nicked a nerve. I feel like I got a giant hole in me.’ She looked at me like I was crazy.
We went to the doctor. He said I was completely healed and asked, ‘What do they have you on?’ Then he said, ‘You just quit taking everything?’ I told him, ‘Yeah, there’s no more pain, so I just quit.’
He said, ‘Well, you’re in withdrawal.’
Once I knew what it was, I was able to tough it out, but it’s not a pleasant experience. I don’t think people are really trying to get high — you just don’t want to feel that alone. I literally felt like there was a hole right through me, like I was just empty inside. So I have a lot of empathy for people that are in addiction.

Rick Wilson was sworn in as the Minister of Mental Health and Addictions on May 16. | Rick Wilson via Facebook
RW: When I was in Indigenous Relations, half my time was spent around addiction issues. It’s horrible. Out on the First Nations, there’s hardly a chief who hasn’t lost a son or somebody close to them. That’s all I did — go to funerals, one after another.
What I learned was you really just have to listen — and that’s one thing the government isn’t good at.
AK: What learnings from that role are you bringing to your new portfolio, and how do you see them benefiting your work in mental health and addiction?
RW: I want to put an Indigenous lens on the whole thing. I think that’s the piece we’re missing. What I found most successful was to use their culture. Get the elders involved. They have the sweats, smudges and language. To take somebody’s language away is devastating.
You hear a lot about reconciliation, but I took it for real. My good friend Willie Littlechild said, ‘Minister, I want to see some reconcili-action.’ He said I could use that — so I do, a lot.
AK: Can Indigenous recovery models work more broadly for non-Indigenous Albertans?
RW: I’ve really seen it work with non-Indigenous folks as well. But everybody’s going to be different. For some people, maybe Christianity is the way to go. And for some people, it’s Alcoholics Anonymous.
I think [the common thread] is that hope. [When you’re addicted] you feel hopeless.
I felt empty, and you need something to replace that emptiness. The problem is, you turn to alcohol, you turn to drugs to fill that gap, and that’s not going to do it. It’s a very temporary fix that just pushes you deeper down the rabbit hole.

Minister Rick Wilson celebrates the Pigeon Lake Regional School Class of 2025 on May 25. | Rick Wilson via Facebook
AK: Can you explain what a recovery community is, and how it fits into the province’s continuum of care?
RW: The way they used to do it, you’d throw someone in recovery for a couple of weeks [and expect] that should cure it, then out you go. Well, that doesn’t work.
[Now] it’s more of a holistic approach: you go into detox, and then from there, you go into rehab. Some people fall out of rehab, [but they go] back into detox, and eventually you start working your way around the circle.
Transitional housing is key. You can’t just send someone back into the community without support — they’ll relapse. After housing, the focus is on community reintegration, finding work, and family support. It’s like an Indigenous healing circle — a full circle to prevent falling back into addiction.
We’re working on 11 sites — one in Red Deer, Gunn, Lethbridge and Calgary opening this summer. Seven more are planned, including Edmonton, Grande Prairie and five with Indigenous communities.
AK: Some critics argue that the Alberta Model leans toward coercive care, and that the benefits of involuntary treatment may not outweigh the risks and costs. How will the Compassionate Intervention Act, which mandates addiction treatment, address those concerns?
RW: Compassionate care isn’t just for the individuals [with substance use disorders]. We have to be compassionate for them, but we also have to be compassionate for the people in their community that are impacted.
In my own riding in the Maskwacîs-Wetaskiwin — some people come in [to the hospital] three times in a day that have overdosed. To overdose several times a day — you’re doing brain damage when you’re at that point.
These people are in dire straits, and we have to intervene with them, because they’re not even capable of thinking for themselves [or] to go for voluntary treatment. We want to give the people that are addicted that opportunity to rebuild their lives. Right now, there’s just a lot of enabling going on.
This interview has been edited and condensed for clarity.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Addictions
Manitoba Is Doubling Down On A Failed Drug Policy

From the Frontier Centre for Public Policy
Manitoba is choosing to expand the same drug policy model that other provinces are abandoning, policies that normalize addiction while sidelining treatment, recovery, and public safety.
The New Democrat premier of British Columbia, David Eby, stood before reporters last spring and called his government’s decision to permit public drug use in certain spaces a failure.
The policy was part of the broader “harm reduction” strategy meant to address overdose deaths. Instead, it had stirred public anger, increased street disorder and had helped neither users nor the communities that host them. “We do not accept street disorder that makes communities feel unsafe,” Eby said. The province scrapped the plan.
In Alberta, the Conservative government began shutting down safer-supply prescribing due to concerns about drug diversion and misuse. The belief that more opioids can resolve the opioid crisis is losing credibility.
Ontario Progressive Conservatives are moving away from harm reduction by shutting down supervised consumption sites near schools and limiting safer-supply prescribing. Federal funding for programs is decreasing, and the province is shifting its focus to treatment models, even though not all sites are yet closed.
Yet amid these non-partisan reversals, Manitoba’s government has announced its intention to open a supervised drug-use site in Winnipeg. Premier Wab Kinew said, “We have too many Manitobans dying from overdose.” True. But it does not follow that repeating failed approaches will yield different results.
Reversing these failed policies is not a rejection of compassion. It is a recognition that good intentions do not produce good outcomes. Vancouver and Toronto have hosted supervised drug-use sites for years. The death toll keeps rising. Drug deaths in British Columbia topped 2,500 in 2023, even with the most expansive harm reduction infrastructure in the country. A peer-reviewed study published this year found that hospitalizations from opioid poisoning rose after B.C.’s safer-supply policy was implemented. Emergency department visits increased by more than three cases per 100,000 population, with no corresponding drop in fatal overdoses.
And the problem persists day to day. Paramedics in B.C. responded to nearly 4,000 overdose calls in July 2024 alone. The monthly call volume has exceeded 3,000 almost every month this year. These are signs of crisis management without a path to recovery.
There are consequences beyond public health. These policies change the character of neighbourhoods. Businesses suffer. Residents feel unsafe. And most tragically, the person using drugs is offered little more than a cot, a nurse and a quiet signal to continue. Real help, like treatment, housing and purpose, remains out of reach.
Somewhere along the way, bureaucracies stopped asking what recovery looks like. They have settled for managing human decline. They call it compassion. But it is really surrender, wrapped in medical language.
Harm reduction had its time. It made sense when it first emerged, during the AIDS crisis, when dirty needles spread HIV. Back then, the goal was to stop a deadly virus. Today, that purpose has been lost.
When policy drifts into ideology, reality becomes an afterthought. Underneath today’s approach is the belief that drug use is inevitable, that people cannot change, that liberty means letting others fade away quietly. These ideas do not reflect science. They do not reflect hope. They reflect despair. They reflect a politics that prioritizes the appearance of compassion over effectiveness.
What Manitoba needs is treatment access that meets the scale of the problem. That means detox beds, recovery homes and long-term care focused on restoring lives. These may not generate the desired headlines, but they work. They are demanding. They are slow. And they offer respect to the person behind the addiction.
There are no shortcuts. No policy will undo decades of pain overnight. But a policy that keeps people stuck using is not mercy. It is maintenance with no way out.
A government that believes in its people should not copy failure.
Marco Navarro-Genie is vice-president of research at the Frontier Centre for Public Policy and co-author, with Barry Cooper, of Canada’s COVID: The Story of a Pandemic Moral Panic (2023).
Addictions
The Death We Manage, the Life We Forget

 Marco Navarro-Génie
Marco Navarro-Génie
Our culture has lost the plot about what it means to live.
Reading that Manitoba is bringing supervised consumption to Winnipeg got me thinking.
Walk through just about any major Canadian city, and you will see them. Figures bent forward at seemingly impossible angles, swaying in the characteristic “fentanyl fold,” suspended between consciousness and oblivion. They resemble the zombies of fiction: bodies that move through space without agency, awareness, or connection to the world around them. We think of zombies as the walking dead. Health workers and bureaucrats reverse their overdoses, send them back to the street, and call it saving lives.
At the same time, Canada offers medical assistance in dying to a woman who cited chemical sensitivities and the inability to find housing. It has been offered to veterans who asked for support and were met instead with an option for death. We fight to prevent one form of death while facilitating another. The contradiction is not accidental. It reveals something about the people involved and the funding behind it. That’s our culture. Us. It appears to me that our culture no longer knows what life is.
Ask any politician or program bureaucrat, and you will hear them explain, in the dry language of bureaucracy, that the twin approach to what they call harm reduction and medical assistance in dying (MAiD) rests on the shared premise of what they believe to be compassion. They think they respect autonomy, prevent suffering, and keep people alive when possible. It sounds humane. It is, in practice, incoherent. Bear with me for a moment.
The medical establishment administers naloxone to reverse overdoses in people who spend as many as twenty hours a day unconscious. They live without meaningful relationships or memories, with little capacity for choice. The technocrats and politicians call that saving lives. They also provide assisted death to people whose suffering comes primarily from poverty, isolation, or lack of housing. There was a time when these factors could, at least in theory, be addressed so that the terminal decision did not need to be made. Now they are accepted as grounds for ending life.
But why is one preference final and the other treated as an error to correct? That question reflects the deeper disorientation.
We saw the same thing during COVID. Elderly people in care homes were left without touch, family, or comfort for days. They often died in solitude, their dementia accelerated by isolation. And those conditions were inflicted upon them in the name of saving their lives. The “system” measured success in preventing infections, not in preserving connections. Je me souviens. Or we should.
There is a pattern here. We have reduced the idea of saving lives to keeping bodies breathing, while ignoring what makes a life human: agency, meaning, development, and relationship. And in doing so, we begin to define life as mere biological persistence. But to define life by the capacity to breathe and perform basic functions is to place ourselves on the same footing as the non-human animals. It is to say, tacitly, that there is no fundamental distinction between a person and a creature. That, too, is a form of forgetting.
To be clear, the argument here is not that hopeless drug users should be administered MAiD. Instead, it is essential to recognize that the intellectual framework behind harm reduction and MAiD must be taken seriously, as it rests on some rationally defensible claims. In an age where most arguments are emotive and unexamined, the mildly logical has become strangely compelling.
It begins with the idea of autonomy. We cannot force others to live by our values. Every person must decide what makes life worth living. To insist otherwise is paternalism.
Then comes pragmatic compassion. People will use drugs whether we approve or not. People will find their lives unbearable, whether we acknowledge it or not. We can support them or moralize while they die.
There is also an emphasis on subjective experience. No one knows another’s pain. If someone says their suffering is intolerable, we are in no position to deny it, they say. If a user would rather face opioids than withdrawal and despair, are we entitled to interfere?
Finally, the comparison to medical ethics: we do not withhold insulin from diabetics who continue to eat poorly. We do not deny cancer treatment to smokers. Medicine responds to suffering, even when the patient has contributed to their condition. Harm reduction, they argue, simply applies that principle to addiction.
These arguments produced tangible benefits, they argue. Needle exchanges reduced HIV transmission. Naloxone kits prevented deaths. Safe injection sites meant fewer people dying alone. MAiD brought relief to those in agony. These were not trivial outcomes. I am aware.
Yet when we look more closely, the very logic that underlies these policies also exposes their fatal limitations.
Addiction undermines choice. It hijacks the brain’s ability to reason, compare, and choose. A person deep in addiction is not selecting between alternatives like someone choosing coffee or tea. The structure of choice, the human will, itself is broken. The addiction decides before the person does. St Augustine knew this. Dostoyevsky knew it too.
And for the empirically minded, the research supports this. In British Columbia, where the “safe supply” model was pioneered, some addiction physicians now say the policy is failing. Worse, it may be creating new opioid dependencies in people who were not previously addicted. A study earlier this year found that opioid‑related hospitalizations increased by about 33 percent, compared with pre‑policy rates. With the later addition of a drug-possession decriminalization policy, hospitalizations rose even more (overall, a 58 percent increase compared to before SOS’s implementation). The study concluded that neither safer supply nor decriminalization was associated with a statistically significant reduction in overdose deaths. This is not freedom. It is a new form of bondage, meticulously paved by official compassion.
Despair disguises itself as autonomy, especially in a spiritually unmoored culture that no longer knows how to cope with suffering. A person requesting assisted death because of chronic, untreatable pain may appear lucid and composed, but lucidity is not the same as wisdom. One can reason clearly from false premises. If life is reduced to the absence of pain and the preservation of comfort, then the presence of suffering will seem like failure, and death will appear rational. But that is not a genuine choice because it is based on a misapprehension of what life is. All life entails pain. Some of it is redemptive. Some of it is endured. But it does not follow that the presence of suffering justifies the conclusion of life.
Someone turning to drugs because of homelessness, abandonment, or despair is often in an even deeper eclipse of the will. Here, there is not even the appearance of deliberation, only the reach for numbness in the absence of meaning. What looks like a decision is the residue of collapse. We are not witnessing two forms of autonomy, one clearer than the other. We are witnessing the breakdown of autonomy in various forms, and pretending that it is freedom.
Biological survival is not life. When we maintain someone in a state of near-constant unconsciousness, with no relationships, no capacity for flourishing, we are not preserving life. We are preserving a body. The person may already be gone. To define life as nothing more than breathing and performing bodily functions is to deny what makes us human. It reduces us to the level of non-human creatures, sentient, perhaps, but without reason, memory, moral reflection, or the possibility of transcendence. It tacitly advances the view that there is no essential difference between a person and a critter, so long as both breathe and respond to some stimuli.
Governments do these things to keep ballooning overdosing deaths down, preferring to maintain drugs users among the undead instead. That reminds me of how the Mexican government hardly moves a finger to find the disappeared, 100,000 strong of lately. For as long ss they’re disappeared, they choose not to count them as homicides, and they feel justified in ignoring the causes of all the killing around them.
Some choices are nefarious. Some choices deserve challenge. Not all autonomous acts are equal. The decision to continue living with pain, or to fight addiction, requires agency. The decision to surrender to despair may signal the absence of it. To say all choices are equal is to empty the word autonomy of meaning.
This reflects a dangerously thin view of the human person that permeates our present. What we now call “harm” is only death or physical pain. What we call good is whatever someone prefers. But people are more than collections of wants.
We should have learned this by now. In Alberta, safer supply prescribing was effectively banned in 2022. Officials cited diversion and lack of measurable improvement. We are forcing some people into treatment because we recognize the impairment of judgement in addiction.
In British Columbia, public drug use was quietly re-criminalized after communities rebelled. This was an admission of policy failure. “Keeping people safe is our highest priority,” Premier David Eby said. Yet safe supply remains. In 2023, the province recorded more than 2,500 overdose deaths. Paramedics continue to respond to thousands of overdose calls each month. This is not success. It is a managed collapse.
Meanwhile, Manitoba is preparing to open its own supervised drug-use site. Premier Wab Kinew said, “We have too many Manitobans dying from overdose… so this is one tool we can use.” That may be so. However, it is a tool that others are beginning to set aside. It is a largely discredited tool. Sadly, in the self-professed age of “Reconciliation” with Aboriginal Canadians, Aboricompassionadians are disproportionately affected by these discredited policies.
The Manitoba example illustrates the broader problem, despite damning evidence. Instead of asking what helps people live, we ask whether they gave consent. We do not ask whether they were capable of it. We ask whether they avoided death. We do not ask whether they found purpose.
We are not asking what might lead someone out of addiction. We are not asking what they need to flourish. We ask only what we can do to prevent them from dying in the short term. And when that becomes impossible, technocracy offers them death in a more organized form, cleanly approved by government. That’s compasson.
The deeper problem is not policy incoherence. It is the cultural despair that skates on the thin ice of meaninglessness. These policies make sense only in a culture that has already decided life is not worth too much. What matters is state endorsement and how it’s done .
It is more cost-effective to distribute naloxone than to construct long-term recovery homes. It is easier to train nurses to supervise injection than to provide months of residential treatment. It is far simpler to legalize euthanasia for the poor and the suffering than to work on solutions that lift them out of both. But is it right?
This is not compassion. It is surrender.
A humane policy would aim to restore agency, not validate its absence. It would seek out what helps people grow in wisdom and self-command, not what leaves them comfortably sedated. It would measure success not in lives prolonged into darker dependency but in persons recovered. In lives better lived.
This vision is harder. It costs time. It requires greater effort. It requires care and what some Christians call love of neighbour. It may require saying no when someone asks for help that could lead to ruin. But anything less is not mercy. It is a slow walk toward death while we leave the “system” to pretend there is no choice.
We did have a choice. We chose shallow comfort over deep obligation. We chose to manage symptoms rather than confront the deeper conditions of our age: loneliness, meaninglessness, despair. And now we live among the results: more, not fewer, people swaying in silence, already gone walking dead.
We might ask what we’ve forgotten about suffering, about responsibility, about what life is. Lives are at stake. True. But when our understanding of life is misdirected, so will be the policies the state gives us.
We are grateful that you’re reading Haultain Research.
For the full experience, and to help us bring you more quality research and commentary,
-

 Automotive6 hours ago
Automotive6 hours agoPoliticians should be honest about environmental pros and cons of electric vehicles
-

 Agriculture2 days ago
Agriculture2 days agoWhy is Canada paying for dairy ‘losses’ during a boom?
-

 Agriculture2 days ago
Agriculture2 days agoCanadians should thank Trump for targeting supply management
-

 Business2 days ago
Business2 days agoWhite House declares inflation era OVER after shock report
-

 Business2 days ago
Business2 days agoCanada Hits the Brakes on Population
-

 Frontier Centre for Public Policy2 days ago
Frontier Centre for Public Policy2 days agoCanada Lets Child-Porn Offenders Off Easy While Targeting Bible Believers
-

 Daily Caller1 day ago
Daily Caller1 day ago‘Almost Sounds Made Up’: Jeffrey Epstein Was Bill Clinton Plus-One At Moroccan King’s Wedding, Per Report
-
 Crime1 day ago
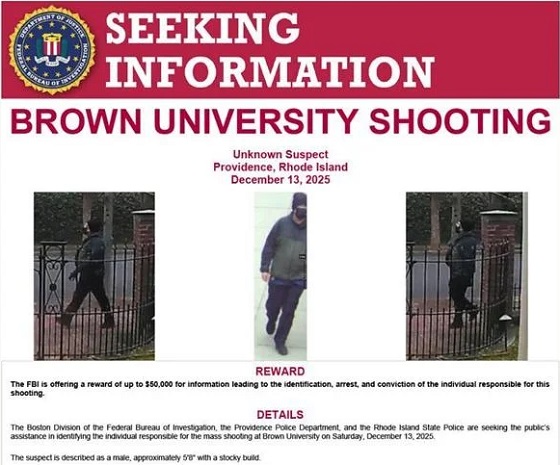
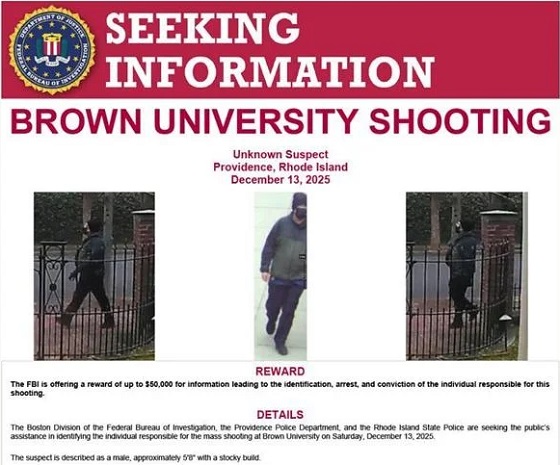
Crime1 day agoBrown University shooter dead of apparent self-inflicted gunshot wound







