Addictions
Does America’s ‘drug czar’ hold lessons for Canada?

Harry Anslinger (center) discussing cannabis control with Canadian narcotics chief Charles Henry Ludovic Sharman and Assistant Secretary of the Treasury Stephen B. Gibbons in 1938. (Photo credit: United States Library of Congress’ Prints and Photographs division)
The US has had a drug czar for decades. Experts share how this position has shaped US drug policy—and what it could mean for Canada
Last week, Canada announced it would appoint a “fentanyl czar” to crack down on organized crime and border security.
The move is part of a suite of security measures designed to address US President Donald Trump’s concerns about fentanyl trafficking and forestall the imposition of 25 per cent tariffs on Canadian goods.
David Hammond, a health sciences professor and research chair at the University of Waterloo, says, “There is no question that Canada would benefit from greater leadership and co-ordination in substance use policy.”
But whether Canada’s fentanyl czar “meets these needs will depend entirely on the scope of their mandate,” he told Canadian Affairs in an email.
Canadian authorities have so far provided few details about the fentanyl czar’s powers and mandate.
A Feb. 4 government news release says the czar will focus on intelligence sharing and collaborating with US counterparts. Canada’s Public Safety Minister, David McGuinty, said in a Feb. 4 CNN interview that the position “will transcend any one part of the government … [It] will pull together a full Canadian national response — between our provinces, our police of local jurisdiction, and work with our American authorities.”
Canada’s approach to the position may take cues from the US, which has long had its own drug czar. Canadian Affairs spoke to several US historians of drug policy to better understand the nature and focus of this role in the US.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
The first drug czar
The term “czar” refers to high-level officials who oversee specific policy areas and have broad authority across agencies.
Today, the US drug czar’s official title is director of the Office of National Drug Control Policy. The director is appointed by the president and responsible for advising the president and coordinating a national drug strategy.
Taleed El-Sabawi, a legal scholar and public health policy expert at Wayne State University in Detroit, Mich., said the Office of National Drug Control Policy has two branches: a law enforcement branch focused on drug supply, and a public health branch focused on demand for drugs.
“Traditionally, the supply side has been the focus and the demand side has taken a side seat,” El-Sabawi said.
David Herzberg, a historian at University at Buffalo in Buffalo, N.Y., made a similar observation.
“US drug policy has historically been dominated by moral crusading — eliminating immoral use of drugs, and policing [or] punishing the immoral people (poor, minority, and foreign/traffickers) responsible for it,” Herzberg told Canadian Affairs in an email.
Harry Anslinger, who was appointed in 1930 as the first commissioner of the Federal Bureau of Narcotics, is considered the earliest iteration of the US drug czar. The bureau later merged into the Drug Enforcement Administration, the lead federal agency responsible for enforcing US drug laws.
Anslinger prioritized enforcement, and his impact was complex.
“He was part of a movement to characterize addicts as depraved and inferior individuals and he supported punitive responses not just to drug dealing but also to drug use,” said Caroline Acker, professor emerita of history at Carnegie Mellon University in Pittsburgh, Pa.
But Anslinger also cracked down on the pharmaceutical industry. He restricted opioid production, effectively making it a low-profit, tightly controlled industry, and countered pharmaceutical public relations campaigns with his own.
“The Federal Bureau of Narcotics [at the time could] in fact be seen as the most robust national consumer protection agency, with powers to regulate and constrain major corporations that the [Food and Drug Administration] could only dream of,” said Herzberg.
The punitive approach to drugs put in place by Anslinger was the dominant model until the Nixon administration. In 1971, President Richard Nixon created an office dedicated to drug abuse prevention and appointed Jerome Jaffe as drug czar.
Jaffe established a network of methadone treatment facilities across the US. Nixon initially combined public health and law enforcement to combat rising heroin use among Vietnam War soldiers, calling addiction the nation’s top health issue.
However, Nixon later reverted back to an enforcement approach when he used drug policy to target Black communities and anti-war activists.
“We knew we couldn’t make it illegal to be either against the war or Black, but by getting the public to associate the hippies with marijuana and Blacks with heroin, and then criminalizing both heavily, we could disrupt those communities,” Nixon’s top domestic policy aide, John Ehrlichman, said in a 1994 interview.
 |
Michael Botticelli, Acting Director of the Office of National Drug Control Policy March 7, 2014 – Jan. 20, 2017 under President Barack Obama. [Photo Credit: Executive Office of the President of the United States]
Back and forth
More recently, in 2009, President Barack Obama appointed Michael Botticelli as drug czar. Botticelli was the first person in active recovery to hold the role.
The Obama administration recognized addiction as a chronic brain disease, a view already accepted in scientific circles but newly integrated into national drug policy. It reduced drug possession sentences and emphasized prevention and treatment.
Trump, who succeeded Obama in 2016, prioritized law enforcement while rolling back harm reduction. In 2018, his administration called for the death penalty for drug traffickers, and in 2019, sued to block a supervised consumption site in Philadelphia, Pa.
Trump appointed James Carroll as drug czar in 2017. But in 2018 Trump proposed slashing the office’s budget by more than 90 per cent and transferring authority for key drug programs to other agencies. Lawmakers blocked the plan, however, and the Office of National Drug Control Policy remained intact.
In 2022, President Joe Biden appointed Dr. Rahul Gupta, the first medical doctor to serve as drug czar. Herzberg says Gupta also prioritized treatment, by, for example, expanding access to naloxone and addiction medications. But he also cracked down on drug trafficking.
In December 2024, Gupta outlined America’s international efforts to combat fentanyl trafficking, naming China, Mexico, Colombia and India as key players — but not Canada.
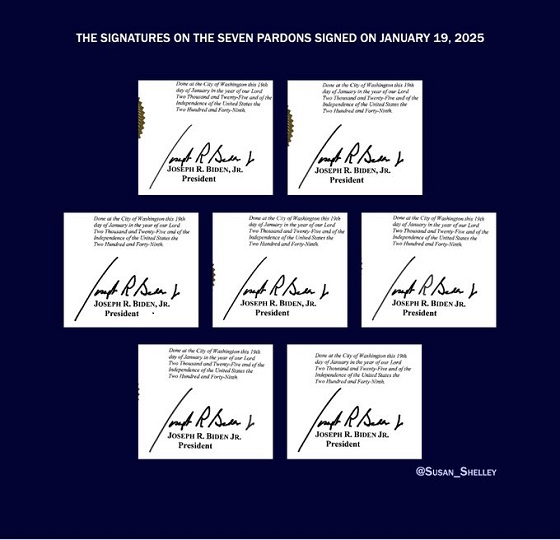
Gupta’s last day was Jan. 19. Trump has yet to appoint someone to the role.
Canada’s fentanyl czar
El-Sabawi says she views Canada’s appointment of a drug czar as a signal that the government will be focused on supply side, law enforcement initiatives.
Hammond, the University of Waterloo professor, says he hopes efforts to address Canada’s drug problems focus on both the supply and demand sides of the equation.
“Supply-side measures are an important component of substance use policy, but limited in their effectiveness when they are not accompanied by demand-side policies,” he said.
The Canada Border Services Agency and Health Canada redirected Canadian Affairs’ inquiries about the new fentanyl czar role to Public Safety Canada. Public Safety Canada did not respond to multiple requests for comment before publication.
El-Sabawi suggests the entire drug czar role needs rethinking.
“I think the role needs to be re-envisioned as one that is more of a coordinator [across] the administrative branch on addiction and overdose issues … as opposed to what it is now, which is really a mouthpiece — symbolic,” she said.
“Most drug czars don’t get much done.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle.
Our content is always free – but if you want to help us commission more high-quality journalism, consider getting a voluntary paid subscription.
Addictions
The War on Commonsense Nicotine Regulation

From the Brownstone Institute
Cigarettes kill nearly half a million Americans each year. Everyone knows it, including the Food and Drug Administration. Yet while the most lethal nicotine product remains on sale in every gas station, the FDA continues to block or delay far safer alternatives.
Nicotine pouches—small, smokeless packets tucked under the lip—deliver nicotine without burning tobacco. They eliminate the tar, carbon monoxide, and carcinogens that make cigarettes so deadly. The logic of harm reduction couldn’t be clearer: if smokers can get nicotine without smoke, millions of lives could be saved.
Sweden has already proven the point. Through widespread use of snus and nicotine pouches, the country has cut daily smoking to about 5 percent, the lowest rate in Europe. Lung-cancer deaths are less than half the continental average. This “Swedish Experience” shows that when adults are given safer options, they switch voluntarily—no prohibition required.
In the United States, however, the FDA’s tobacco division has turned this logic on its head. Since Congress gave it sweeping authority in 2009, the agency has demanded that every new product undergo a Premarket Tobacco Product Application, or PMTA, proving it is “appropriate for the protection of public health.” That sounds reasonable until you see how the process works.
Manufacturers must spend millions on speculative modeling about how their products might affect every segment of society—smokers, nonsmokers, youth, and future generations—before they can even reach the market. Unsurprisingly, almost all PMTAs have been denied or shelved. Reduced-risk products sit in limbo while Marlboros and Newports remain untouched.
Only this January did the agency relent slightly, authorizing 20 ZYN nicotine-pouch products made by Swedish Match, now owned by Philip Morris. The FDA admitted the obvious: “The data show that these specific products are appropriate for the protection of public health.” The toxic-chemical levels were far lower than in cigarettes, and adult smokers were more likely to switch than teens were to start.
The decision should have been a turning point. Instead, it exposed the double standard. Other pouch makers—especially smaller firms from Sweden and the US, such as NOAT—remain locked out of the legal market even when their products meet the same technical standards.
The FDA’s inaction has created a black market dominated by unregulated imports, many from China. According to my own research, roughly 85 percent of pouches now sold in convenience stores are technically illegal.
The agency claims that this heavy-handed approach protects kids. But youth pouch use in the US remains very low—about 1.5 percent of high-school students according to the latest National Youth Tobacco Survey—while nearly 30 million American adults still smoke. Denying safer products to millions of addicted adults because a tiny fraction of teens might experiment is the opposite of public-health logic.
There’s a better path. The FDA should base its decisions on science, not fear. If a product dramatically reduces exposure to harmful chemicals, meets strict packaging and marketing standards, and enforces Tobacco 21 age verification, it should be allowed on the market. Population-level effects can be monitored afterward through real-world data on switching and youth use. That’s how drug and vaccine regulation already works.
Sweden’s evidence shows the results of a pragmatic approach: a near-smoke-free society achieved through consumer choice, not coercion. The FDA’s own approval of ZYN proves that such products can meet its legal standard for protecting public health. The next step is consistency—apply the same rules to everyone.
Combustion, not nicotine, is the killer. Until the FDA acts on that simple truth, it will keep protecting the cigarette industry it was supposed to regulate.
Addictions
The Shaky Science Behind Harm Reduction and Pediatric Gender Medicine


By Adam Zivo
Both are shaped by radical LGBTQ activism and questionable evidence.
Over the past decade, North America embraced two disastrous public health movements: pediatric gender medicine and “harm reduction” for drug use. Though seemingly unrelated, these movements are actually ideological siblings. Both were profoundly shaped by extremist LGBTQ activism, and both have produced grievous harms by prioritizing ideology over high-quality scientific evidence.
While harm reductionists are known today for championing interventions that supposedly minimize the negative effects of drug consumption, their movement has always been connected to radical “queer” activism. This alliance began during the 1980s AIDS crisis, when some LGBTQ activists, hoping to reduce HIV infections, partnered with addicts and drug-reform advocates to run underground needle exchanges.
The Bureau is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
In the early 2000s, after the North American AIDS epidemic was brought under control, many HIV organizations maintained their relevance (and funding) by pivoting to addiction issues. Despite having no background in addiction medicine, their experience with drug users in the context of infectious diseases helped them position themselves as domain experts.
These organizations tended to conceptualize addiction as an incurable infection—akin to AIDS or Hepatitis C—and as a permanent disability. They were heavily staffed by progressives who, influenced by radical theory, saw addicts as a persecuted minority group. According to them, drug use itself was not the real problem—only society’s “moralizing” norms.
These factors drove many HIV organizations to lobby aggressively for harm reduction at the expense of recovery-oriented care. Their efforts proved highly successful in Canada, where I am based, as HIV researchers were a driving force behind the implementation of supervised consumption sites and “safer supply” (free, government-supplied recreational drugs for addicts).
From the 2010s onward, the association between harm reductionism and queer radicalism only strengthened, thanks to the popularization of “intersectional” social justice activism that emphasized overlapping forms of societal oppression. Progressive advocates demanded that “marginalized” groups, including drug addicts and the LGBTQ community, show enthusiastic solidarity with one another.
These two activist camps sometimes worked on the same issues. For example, the gay community is struggling with a silent epidemic of “chemsex” (a dangerous combination of drugs and anonymous sex), which harm reductionists and queer theorists collaboratively whitewash as a “life-affirming cultural practice” that fosters “belonging.”
For the most part, though, the alliance has been characterized by shared tones and tactics—and bad epistemology. Both groups deploy politicized, low-quality research produced by ideologically driven activist-researchers. The “evidence-base” for pediatric gender medicine, for example, consists of a large number of methodologically weak studies. These often use small, non-representative samples to justify specious claims about positive outcomes. Similarly, harm reduction researchers regularly conduct semi-structured interviews with small groups of drug users. Ignoring obvious limitations, they treat this testimony as objective evidence that pro-drug policies work or are desirable.
Gender clinicians and harm reductionists are also averse to politically inconvenient data. Gender clinicians have failed to track long-term patient outcomes for medically transitioned children. In some cases, they have shunned detransitioners and excluded them from their research. Harm reductionists have conspicuously ignored the input of former addicts, who generally oppose laissez-faire drug policies, and of non-addict community members who live near harm-reduction sites.
Both fields have inflated the benefits of their interventions while concealing grievous harms. Many vulnerable children, whose gender dysphoria otherwise might have resolved naturally, were chemically castrated and given unnecessary surgeries. In parallel, supervised consumption sites and “safer supply” entrenched addiction, normalized public drug use, flooded communities with opioids, and worsened public disorder—all without saving lives.
In both domains, some experts warned about poor research practices and unmeasured harms but were silenced by activists and ideologically captured institutions. In 2015, one of Canada’s leading sexologists, Kenneth Zucker, was fired from the gender clinic he had led for decades because he opposed automatically affirming young trans-identifying patients. Analogously, dozens of Canadian health-care professionals have told me that they feared publicly criticizing aspects of the harm-reduction movement. They thought doing so could invite activist harassment while jeopardizing their jobs and grants.
By bullying critics into silence, radical activists manufactured false consensus around their projects. The harm reductionists insist, against the evidence, that safer supply saves lives. Their idea of “evidence-based policymaking” amounts to giving addicts whatever they ask for. “The science is settled!” shout the supporters of pediatric gender medicine, though several systematic reviews proved it was not.
Both movements have faced a backlash in recent years. Jurisdictions throughout the world are, thankfully, curtailing irreversible medical procedures for gender-confused youth and shifting toward a psychotherapy-based “wait and see” approach. Drug decriminalization and safer supply are mostly dead in North America and have been increasingly disavowed by once-supportive political leaders.
Harm reductionists and queer activists are trying to salvage their broken experiments, occasionally by drawing explicit parallels between their twin movements. A 2025 paper published in the International Journal of Drug Policy, for example, asserts that “efforts to control, repress, and punish drug use and queer and trans existence are rising as right-wing extremism becomes increasingly mainstream.” As such, there is an urgent need to “cultivate shared solidarity and action . . . whether by attending protests, contacting elected officials, or vocally defending these groups in hostile spaces.”
How should critics respond? They should agree with their opponents that these two radical movements are linked—and emphasize that this is, in fact, a bad thing. Large swathes of the public understand that chemically and surgically altering vulnerable children is harmful, and that addicts shouldn’t be allowed to commandeer public spaces. Helping more people grasp why these phenomena arose concurrently could help consolidate public support for reform and facilitate a return to more restrained policies.
Adam Zivo is director of the Canadian Centre for Responsible Drug Policy.
For the full experience, please upgrade your subscription and support a public interest startup.
We break international stories and this requires elite expertise, time and legal costs.
-

 Agriculture2 days ago
Agriculture2 days agoDanish Cows Collapsing Under Mandatory Methane-Reducing Additive
-

 Alberta2 days ago
Alberta2 days agoAlberta government’s plan will improve access to MRIs and CT scans
-

 Business2 days ago
Business2 days agoNo Jobs Clause: Liberals Under Fire Over Stellantis Deal in Fiery Committee Showdown
-

 Economy2 days ago
Economy2 days agoWelcome to the Energy Humanist Club! Bill Gates breaks the moral monopoly against fossil fuels
-

 Business2 days ago
Business2 days agoBudget 2025 continues to balloon spending and debt
-

 Censorship Industrial Complex1 day ago
Censorship Industrial Complex1 day agoHow the UK and Canada Are Leading the West’s Descent into Digital Authoritarianism
-

 Business1 day ago
Business1 day agoCapital Flight Signals No Confidence In Carney’s Agenda
-

 Business2 days ago
Business2 days agoFederal budget: Carney government posts largest deficit in Canadian history outside pandemic