Health
Canada surrenders control of future health crises to WHO with ‘pandemic agreement’: report

From LifeSiteNews
Canada’s top constitutional freedom group warned that government officials have “relinquished” control over “future health crises” by accepting the terms of the World Health Organization’s (WHO) revised International Health Regulations (IHR).
The warning came in a report released by the Justice Centre for Constitutional Freedoms (JCCF). The group said that Prime Minister Mark Carney’s acceptance earlier this year of the WHO’s globalist-minded “pandemic agreement” has “placed Canadian sovereignty on loan to an unelected international body.”
“By accepting the WHO’s revised IHR, the report explains, Canada has relinquished its own control over future health crises and instead has agreed to let the WHO determine when a ‘pandemic emergency’ exists and what Canada must do to respond to it, after which Canada must report back to the WHO,” the JCCF noted.
The report, titled Canada’s Surrender of Sovereignty: New WHO health regulations undermine Canadian democracy and Charter freedoms, was authored by Nigel Hannaford, a veteran journalist and researcher.
The WHO’s IHR amendments, which took effect on September 19, are “binding,” according to the organization.
As reported by LifeSiteNews, Canada’s government under Carney signed onto them in May.
Hannaford warned in his report that “(t)he WHO has no legal authority to impose orders on any country, nor does the WHO possess an army, police, or courts to enforce its orders or regulations.”
“Nevertheless, the WHO regards its own regulations as ‘an instrument of international law that is legally binding on 196 countries, including Canada” he wrote.
Hannaford noted that “Surrendering Canada’s sovereignty” to the IHR bodies is itself “contrary to the constitutional principle of democratic accountability, also found in the Canadian Charter of Rights and Freedoms.”
“Canada’s health policies must reflect the needs, desires, and freedoms of Canadians – not the mandates of distant bureaucrats in Geneva or global elites in Davos. A free and democratic Canada requires vigilance and action on the part of Canadians. The time to act is now” he wrote.
Among the most criticized parts of the agreement is the affirmation that “the World Health Organization is the directing and coordinating authority on international health work, including on pandemic prevention, preparedness and response.”
While the agreement claims to uphold “the principle of the sovereignty of States in addressing public health matters,” it also calls for a globally unified response in the event of a pandemic, stating plainly that “(t)he Parties shall promote a One Health approach for pandemic prevention, preparedness and response.”
Constitutional lawyer Allison Pejovic noted that “(b)y treating WHO edicts as binding, the federal government has effectively placed Canadian sovereignty on loan to an unelected international body.”
“Such directives, if enforced, would likely violate Canadians’ Charter rights and freedoms,” she added.
Hannaford said that “Canada’s health policies must be made in Canada.”
“No free and democratic nation should outsource its emergency powers to unelected bureaucrats in Geneva,” he wrote.
The report warned that new IHR regulations could mandate that signatory nations impose strict health-related policies, such as vaccine mandates or lockdowns, with no “public accountability.”
“Once the WHO declares a ‘Pandemic Emergency,’ member states are obligated to implement such emergency measures ‘without delay’ for a minimum of three months,” the JCCF said.
“Canada should instead withdraw from the revised IHR, following the example of countries like Germany, Austria, Italy, the Czech Republic, and the United States,” the JCCF continued. “The report recommends continued international cooperation without surrendering control over domestic health policies.”
Earlier this year, Conservative MP Leslyn Lewis condemned the Liberal government for accepting the WHO’s IHR.
Brownstone Institute
The Doctor Will Kill You Now

From the Brownstone Institute
Way back in the B.C. era (Before Covid), I taught Medical Humanities and Bioethics at an American medical school. One of my older colleagues – I’ll call him Dr. Quinlan – was a prominent member of the faculty and a nationally recognized proponent of physician-assisted suicide.
Dr. Quinlan was a very nice man. He was soft-spoken, friendly, and intelligent. He had originally become involved in the subject of physician-assisted suicide by accident, while trying to help a patient near the end of her life who was suffering terribly.
That particular clinical case, which Dr. Quinlan wrote up and published in a major medical journal, launched a second career of sorts for him, as he became a leading figure in the physician-assisted suicide movement. In fact, he was lead plaintiff in a challenge of New York’s then-prohibition against physician-assisted suicide.
The case eventually went all the way to the US Supreme Court, which added to his fame. As it happened, SCOTUS ruled 9-0 against him, definitively establishing that there is no “right to die” enshrined in the Constitution, and affirming that the state has a compelling interest to protect the vulnerable.
SCOTUS’s unanimous decision against Dr. Quinlan meant that his side had somehow pulled off the impressive feat of uniting Antonin Scalia, Ruth Bader Ginsberg, and all points in between against their cause. (I never quite saw how that added to his luster, but such is the Academy.)
At any rate, I once had a conversation with Dr. Quinlan about physician-assisted suicide. I told him that I opposed it ever becoming legal. I recall he calmly, pleasantly asked me why I felt that way.
First, I acknowledged that his formative case must have been very tough, and allowed that maybe, just maybe, he had done right in that exceptionally difficult situation. But as the legal saying goes, hard cases make bad law.
Second, as a clinical physician, I felt strongly that no patient should ever see their doctor and have to wonder if he was coming to help keep them alive or to kill them.
Finally, perhaps most importantly, there’s this thing called the slippery slope.
As I recall, he replied that he couldn’t imagine the slippery slope becoming a problem in a matter so profound as causing a patient’s death.
Well, maybe not with you personally, Dr. Quinlan, I thought. I said no more.
But having done my residency at a major liver transplant center in Boston, I had had more than enough experience with the rather slapdash ethics of the organ transplantation world. The opaque shuffling of patients up and down the transplant list, the endless and rather macabre scrounging for donors, and the nebulous, vaguely sinister concept of brain death had all unsettled me.
Prior to residency, I had attended medical school in Canada. In those days, the McGill University Faculty of Medicine was still almost Victorian in its ways: an old-school, stiff-upper-lip, Workaholics-Anonymous-chapter-house sort of place. The ethic was hard work, personal accountability for mistakes, and above all primum non nocere – first, do no harm.
Fast forward to today’s soft-core totalitarian state of Canada, the land of debanking and convicting peaceful protesters, persecuting honest physicians for speaking obvious truth, fining people $25,000 for hiking on their own property, and spitefully seeking to slaughter harmless animals precisely because they may hold unique medical and scientific value.
To all those offenses against liberty, morality, and basic decency, we must add Canada’s aggressive policy of legalizing, and, in fact, encouraging industrial-scale physician-assisted suicide. Under Canada’s Medical Assistance In Dying (MAiD) program, which has been in place only since 2016, physician-assisted suicide now accounts for a terrifying 4.7 percent of all deaths in Canada.
MAiD will be permitted for patients suffering from mental illness in Canada in 2027, putting it on par with the Netherlands, Belgium, and Switzerland.
To its credit, and unlike the Netherlands and Belgium, Canada does not allow minors to access MAiD. Not yet.
However, patients scheduled to be terminated via MAiD in Canada are actively recruited to have their organs harvested. In fact, MAiD accounts for 6 percent of all deceased organ donors in Canada.
In summary, in Canada, in less than 10 years, physician-assisted suicide has gone from illegal to both an epidemic cause of death and a highly successful organ-harvesting source for the organ transplantation industry.
Physician-assisted suicide has not slid down the slippery slope in Canada. It has thrown itself off the face of El Capitan.
And now, at long last, physician-assisted suicide may be coming to New York. It has passed the House and Senate, and just awaits the Governor’s signature. It seems that the 9-0 Supreme Court shellacking back in the day was just a bump in the road. The long march through the institutions, indeed.
For a brief period in Western history, roughly from the introduction of antibiotics until Covid, hospitals ceased to be a place one entered fully expecting to die. It appears that era is coming to an end.
Covid demonstrated that Western allopathic medicine has a dark, sadistic, anti-human side – fueled by 20th-century scientism and 21st-century technocratic globalism – to which it is increasingly turning. Physician-assisted suicide is a growing part of this death cult transformation. It should be fought at every step.
I have not seen Dr. Quinlan in years. I do not know how he might feel about my slippery slope argument today.
I still believe I was correct.
Business
Canada has fewer doctors, hospital beds, MRI machines—and longer wait times—than most other countries with universal health care
From the Fraser Institute
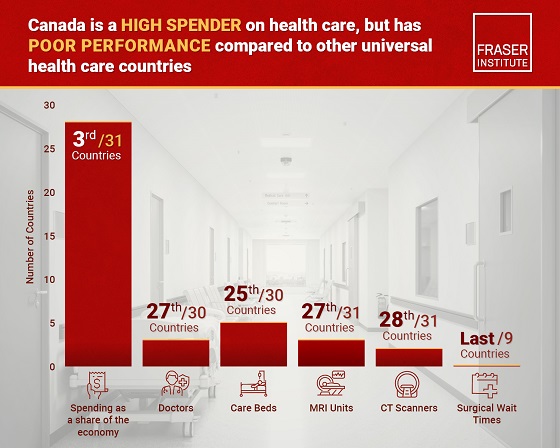
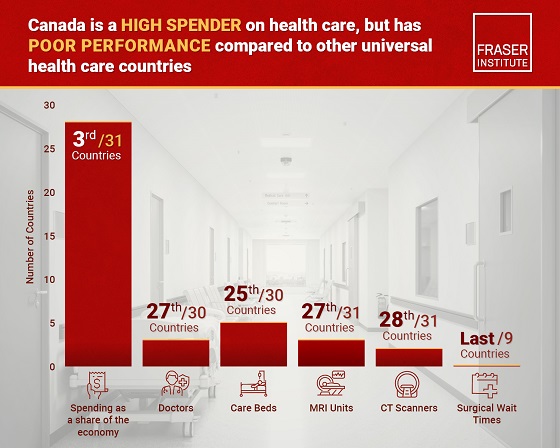
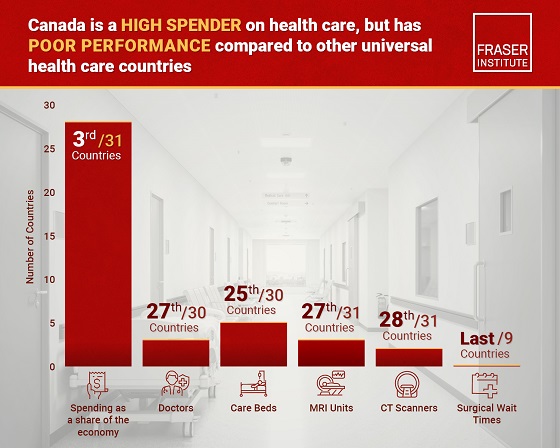
Despite a relatively high level of spending, Canada has significantly fewer doctors, hospital beds, MRI machines and CT scanners compared to other countries with universal health care, finds a new study released today by the Fraser Institute, an independent, non-partisan Canadian public policy think-tank.
“There’s a clear imbalance between the high cost of Canada’s health-care system and the actual care Canadians receive in return,” said Mackenzie Moir, senior policy
analyst at the Fraser Institute and author of Comparing Performance of Universal Health-Care Countries, 2025.
In 2023, the latest year of available comparable data, Canada spent more on health care (as a percentage of the economy/GDP, after adjusting for population age) than
most other high-income countries with universal health care (ranking 3rd out of 31 countries, which include the United Kingdom, Australia and the Netherlands).
And yet, Canada ranked 27th (of 30 countries) for the availability of doctors and 25th (of 30) for the availability of hospital beds.
In 2022, the latest year of diagnostic technology data, Canada ranked 27th (of 31 countries) for the availability of MRI machines and 28th (of 31) for CT scanners.
And in 2023, among the nine countries with universal health-care systems included in the Commonwealth Fund’s International Health Policy Survey, Canada ranked last for the percentage of patients able to make same- or next-day appointments when sick (22 per cent) and had the highest percentage of patients (58 per cent) who waited two months or more for non-emergency surgery. For comparison, the Netherlands had much higher rates of same- or next-day appointments (47 per cent) and much lower waits of two months or more for non-emergency surgery (20 per cent).
“To improve health care for Canadians, our policymakers should learn from other countries around the world with higher-performing universal health-care systems,”
said Nadeem Esmail, director of health policy at the Fraser Institute.
Comparing Performance of Universal Health Care Countries, 2025
- Of the 31 high-income universal health-care countries, Canada ranks among the highest spenders, but ranks poorly on both the availability of most resources and access to services.
- After adjustments for differences in the age of the population of these 31 countries, Canada ranked third highest for spending as a percentage of GDP in 2023 (the most recent year of comparable data).
- Across 13 indictors measured, the availability of medical resources and timely access to medical services in Canada was generally below that of the average OECD country.
- In 2023, Canada ranked 27th (of 30) for the relative availability of doctors and 25th (of 30) for hospital beds dedicated to physical care. In 2022, Canada ranked 27th (of 31) for the relative availability of Magnetic Resonance Im-aging (MRI) machines, and 28th (of 31) for CT scanners.
- Canada ranked last (or close to last) on three of four indicators of timeliness of care.
- Notably, among the nine countries for which comparable wait times measures are available, Canada ranked last for the percentage of patients reporting they were able to make a same- or next-day appointment when sick (22%).
- Canada also ranked eighth worst for the percentage of patients who waited more than one month to see a specialist (65%), and reported the highest percentage of patients (58%) who waited two months or more for non-emergency surgery.
- Clearly, there is an imbalance between what Canadians get in exchange for the money they spend on their health-care system.
Mackenzie Moir
Senior Policy Analyst, Fraser Institute
-

 Courageous Discourse2 days ago
Courageous Discourse2 days agoNo Exit Wound – EITHER there was a very public “miracle” OR Charlie Kirk’s murder is not as it appears
-

 Business2 days ago
Business2 days agoEmission regulations harm Canadians in exchange for no environmental benefit
-

 Alberta2 days ago
Alberta2 days agoPetition threatens independent school funding in Alberta
-

 Business2 days ago
Business2 days agoQuebecers want feds to focus on illegal gun smuggling not gun confiscation
-
 National2 days ago
National2 days agoPolitically Connected Canadian Weed Sellers Push Back in B.C. Court, Seek Distance from Convicted Heroin Trafficker
-

 Business1 day ago
Business1 day agoCanada Revenue Agency found a way to hit “Worse Than Rock Bottom”
-

 MAiD1 day ago
MAiD1 day agoDisabled Canadians increasingly under pressure to opt for euthanasia during routine doctor visits
-
 Business2 days ago
Business2 days agoCanada has fewer doctors, hospital beds, MRI machines—and longer wait times—than most other countries with universal health care