Health
Canada remains poor performer among countries with universal health care

From the Fraser Institute
By Mackenzie Moir and Bacchus Barua
Canada reported far fewer physicians (ranking 28th of 30) and hospital beds (23rd of 29) per 1,000 people in 2021. And ranked low for the availability of MRI machines (25th of 29) and CT scanners (26thof 30) per million people in 2019
Earlier this year, the Trudeau government announced it will increase health-care spending to provinces and territories by $196.1 billion over the next decade. But patients hoping for improved access will likely be disappointed. In reality, Canada’s health-care system already ranks as one of the most expensive systems in the world, but only has mediocre results to show for it. In other words, the problem isn’t the amount of money we spend, it’s the poor value we get for our health-care dollars.
A new study compared the spending and performance of Canada’s system with 29 other universal health-care systems worldwide. According to the study (after adjusting for population age in each country), Canada was the highest spender on health care as a share of the economy (at 12.6 per cent) and ninth-highest on a per person basis in 2021, the latest year of available data.
And yet, compared to other universal countries, Canada reported far fewer physicians (ranking 28th of 30) and hospital beds (23rd of 29) per 1,000 people in 2021. And ranked low for the availability of MRI machines (25th of 29) and CT scanners (26thof 30) per million people in 2019 (the latest year of available data).
Unsurprisingly, scarce health-care resources are accompanied by long wait times. Using data collected in 2020 by the Commonwealth Fund, the study found that only 38 per cent of Canadians reported waiting less than four weeks for a specialist appointment—a much smaller percentage than countries such as Switzerland (68 per cent) and Germany (67 per cent). On this indicator, Canada ranked 10th out of 10 countries. Canada also ranked dead last (10th) on timely access to elective surgery—with 62 per cent of Canadians reporting waiting less than four months—compared to 99 per cent of Germans and 94 per cent of Swiss.
While these results were disappointing, Canada reported mixed results in other areas of performance. For example, although Canada performed poorly on safety indicators such as obstetric trauma during birth (23rd of 23 countries), it performed above the OECD average on other indicators including heart attack survival rates (9th of 25 countries). But while the Canadian system has in some areas performed in line with its high spending levels, overall it’s struggled to meet many of its basic obligations—especially timely access to care.
With its latest increase in health-care spending, the Trudeau government again ignores the fact that Canada already has one of the most expensive universal health-care systems in the world. And although some of this new spending is predicated on provinces tracking progress and demonstrating improvement on certain indicators, international data reveal a simple truth—Canadians do not receive commensurate value for their health-care dollars. Without fundamental reform, it’s unlikely the new spending promised by the Trudeau government will produce improved performance for Canadian patients and their families.
Authors:
Health
All 12 Vaccinated vs. Unvaccinated Studies Found the Same Thing: Unvaccinated Children Are Far Healthier

I joined Del Bigtree in studio on The HighWire to discuss what the data now make unavoidable: the CDC’s 81-dose hyper-vaccination schedule is driving the modern epidemics of chronic disease and autism.
This was not a philosophical debate or a clash of opinions. We walked through irrefutable, peer-reviewed evidence showing that whenever vaccinated and unvaccinated children are compared directly, the unvaccinated group is far healthier—every single time.
Reanalyzing the Largest Vaccinated vs. Unvaccinated Birth-Cohort Study Ever Conducted
At the center of our discussion was our peer-reviewed reanalysis of the Henry Ford Health System vaccinated vs. unvaccinated birth-cohort study (Lamerato et al.)—the largest and most rigorous comparison of its kind ever conducted.
|
The original authors relied heavily on Cox proportional hazards models, a time-adjusted approach that can soften absolute disease burden. Even so, nearly all chronic disease outcomes were higher in vaccinated children.
Our reanalysis used direct proportional comparisons, stripping away the smoothing and revealing the full magnitude of the signal.
- All 22 chronic disease categories favored the unvaccinated cohort when proportional disease burden was examined
- Cancer incidence was 54% higher in vaccinated children (0.0102 vs. 0.0066)
- When autism-associated conditions were grouped appropriately—including autism, ADHD, developmental delay, learning disability, speech disorder, neurologic impairment, seizures, and related diagnoses—the vaccinated cohort showed a 549% higher odds of autism-spectrum–associated clinical outcomes
The findings are internally consistent, biologically coherent, and concordant with every prior vaccinated vs. unvaccinated study, all of which show drastically poorer health outcomes among vaccinated children
The 12 Vaccinated vs. Unvaccinated Studies Regulators Ignore
In the McCullough Foundation Autism Report, we compiled all 12 vaccinated vs. unvaccinated pediatric studies currently available. These studies span different populations, countries, study designs, and data sources.
Every single one reports the same overall pattern. Across all 12 studies, unvaccinated children consistently exhibit substantially lower rates of chronic disease, including:
- Autism and other neurodevelopmental disorders
- ADHD, tics, learning and speech disorders
- Asthma, allergies, eczema, and autoimmune conditions
- Chronic ear infections, skin disorders, and gastrointestinal illness
This level of consistency across independent datasets is precisely what epidemiology looks for when assessing causality. It also explains why no federal agency has ever conducted—or endorsed—a fully vaccinated vs. fully unvaccinated safety study.
Flu Shot Failure
We also addressed the persistent failure of seasonal influenza vaccination.
A large Cleveland Clinic cohort study of 53,402 employees followed participants during the 2024–2025 respiratory viral season and found:
- 82.1% of employees were vaccinated against influenza
- Vaccinated individuals had a 27% higher adjusted risk of influenza compared with the unvaccinated state (HR 1.27; 95% CI 1.07–1.51; p = 0.007)
- This corresponded to a negative vaccine effectiveness of −26.9% (95% CI −55.0 to −6.6%), meaning vaccination was associated with increased—not reduced—risk of influenza
When vaccination exposure increases, chronic disease, neurodevelopmental disorders, and inflammatory illness increase with it. When children are unvaccinated, they are measurably healthier across virtually every outcome that matters.
The science needed to confront the chronic disease and autism epidemics already exists. What remains is the willingness to acknowledge it.
Epidemiologist and Foundation Administrator, McCullough Foundation
Support our mission: mcculloughfnd.org
Please consider following both the McCullough Foundation and my personal account on X (formerly Twitter) for further content.
FOCAL POINTS (Courageous Discourse) is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Alberta
A Christmas wish list for health-care reform

From the Fraser Institute
By Nadeem Esmail and Mackenzie Moir
It’s an exciting time in Canadian health-care policy. But even the slew of new reforms in Alberta only go part of the way to using all the policy tools employed by high performing universal health-care systems.
For 2026, for the sake of Canadian patients, let’s hope Alberta stays the path on changes to how hospitals are paid and allowing some private purchases of health care, and that other provinces start to catch up.
While Alberta’s new reforms were welcome news this year, it’s clear Canada’s health-care system continued to struggle. Canadians were reminded by our annual comparison of health care systems that they pay for one of the developed world’s most expensive universal health-care systems, yet have some of the fewest physicians and hospital beds, while waiting in some of the longest queues.
And speaking of queues, wait times across Canada for non-emergency care reached the second-highest level ever measured at 28.6 weeks from general practitioner referral to actual treatment. That’s more than triple the wait of the early 1990s despite decades of government promises and spending commitments. Other work found that at least 23,746 patients died while waiting for care, and nearly 1.3 million Canadians left our overcrowded emergency rooms without being treated.
At least one province has shown a genuine willingness to do something about these problems.
The Smith government in Alberta announced early in the year that it would move towards paying hospitals per-patient treated as opposed to a fixed annual budget, a policy approach that Quebec has been working on for years. Albertans will also soon be able purchase, at least in a limited way, some diagnostic and surgical services for themselves, which is again already possible in Quebec. Alberta has also gone a step further by allowing physicians to work in both public and private settings.
While controversial in Canada, these approaches simply mirror what is being done in all of the developed world’s top-performing universal health-care systems. Australia, the Netherlands, Germany and Switzerland all pay their hospitals per patient treated, and allow patients the opportunity to purchase care privately if they wish. They all also have better and faster universally accessible health care than Canada’s provinces provide, while spending a little more (Switzerland) or less (Australia, Germany, the Netherlands) than we do.
While these reforms are clearly a step in the right direction, there’s more to be done.
Even if we include Alberta’s reforms, these countries still do some very important things differently.
Critically, all of these countries expect patients to pay a small amount for their universally accessible services. The reasoning is straightforward: we all spend our own money more carefully than we spend someone else’s, and patients will make more informed decisions about when and where it’s best to access the health-care system when they have to pay a little out of pocket.
The evidence around this policy is clear—with appropriate safeguards to protect the very ill and exemptions for lower-income and other vulnerable populations, the demand for outpatient healthcare services falls, reducing delays and freeing up resources for others.
Charging patients even small amounts for care would of course violate the Canada Health Act, but it would also emulate the approach of 100 per cent of the developed world’s top-performing health-care systems. In this case, violating outdated federal policy means better universal health care for Canadians.
These top-performing countries also see the private sector and innovative entrepreneurs as partners in delivering universal health care. A relationship that is far different from the limited individual contracts some provinces have with private clinics and surgical centres to provide care in Canada. In these other countries, even full-service hospitals are operated by private providers. Importantly, partnering with innovative private providers, even hospitals, to deliver universal health care does not violate the Canada Health Act.
So, while Alberta has made strides this past year moving towards the well-established higher performance policy approach followed elsewhere, the Smith government remains at least a couple steps short of truly adopting a more Australian or European approach for health care. And other provinces have yet to even get to where Alberta will soon be.
Let’s hope in 2026 that Alberta keeps moving towards a truly world class universal health-care experience for patients, and that the other provinces catch up.
-

 Business22 hours ago
Business22 hours agoICYMI: Largest fraud in US history? Independent Journalist visits numerous daycare centres with no children, revealing massive scam
-

 Alberta13 hours ago
Alberta13 hours agoAlberta project would be “the biggest carbon capture and storage project in the world”
-
 Bruce Dowbiggin2 days ago
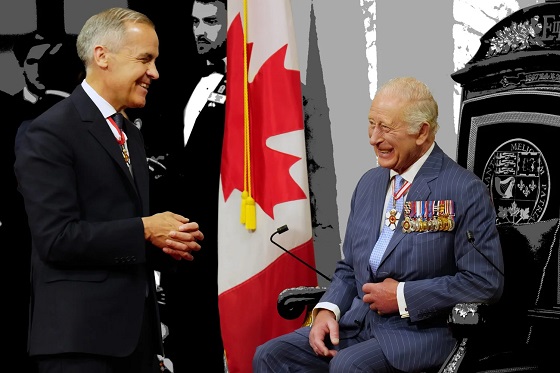
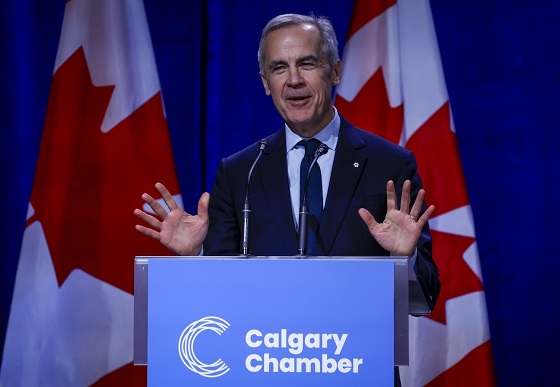
Bruce Dowbiggin2 days agoBe Careful What You Wish For In 2026: Mark Carney With A Majority
-
 Energy10 hours ago
Energy10 hours agoCanada’s debate on energy levelled up in 2025
-

 Energy12 hours ago
Energy12 hours agoNew Poll Shows Ontarians See Oil & Gas as Key to Jobs, Economy, and Trade
-

 Business11 hours ago
Business11 hours agoSocialism vs. Capitalism
-

 International2 days ago
International2 days agoChina Stages Massive Live-Fire Encirclement Drill Around Taiwan as Washington and Japan Fortify
-

 Energy2 days ago
Energy2 days agoRulings could affect energy prices everywhere: Climate activists v. the energy industry in 2026