Alberta
Moustaches for Men’s Health – The Meaning of Movember

It’s that time of year again! Whether it’s your least favorite month, or this is your time to shine – Movember is back!
 While the fun is certainly in the facial hair … Movember is more than just the opportunity to fill in those mutton chops or grow a socially acceptable handlebar moustache. The meaning of this month goes further than flexing the best (or worst) facial hair fashion, it’s the chance to take part in a global movement to support and promote men’s health.
While the fun is certainly in the facial hair … Movember is more than just the opportunity to fill in those mutton chops or grow a socially acceptable handlebar moustache. The meaning of this month goes further than flexing the best (or worst) facial hair fashion, it’s the chance to take part in a global movement to support and promote men’s health.
“The moustache is something of a Trojan Horse that encourages men to engage with their health and talk about the things they often don’t, but should,” says Mitch Hermansen, Western Canada Lead for Movember, “There’s no such thing as a bad moustache. They can all start conversations and save lives.”
Founded in 2003 among four friends, Movember is now the world’s leading men’s health charity, with more than 6 million global supporters all committed to changing the narrative surrounding male health and helping men live “happier, healthier, longer lives”.

The average life expectancy of a man is 6 years shorter than that of the average woman. Movember is working to minimize this gap by focusing on the three factors that pose the greatest risk to mens health worldwide: prostate cancer, testicular cancer and suicide.
Globally, there are 9.9 million men living with or experiencing the effects of prostate cancer. According to the American Cancer Society, prostate cancer is the second leading cause of cancer death in American men, with 1 in 9 men being diagnosed with prostate cancer in their lifetime, and approximately 1 in 41 men dying as a result.
Testicular cancer is the world’s most common cancer among men ages 15-39, and the American Cancer Society estimates 1 in every 250 males will develop testicular cancer during their lifetime. Education, early detection and effective treatments have put the survival rate for this diagnosis at greater than 95%, however the long-term side effects and impacts can have lasting negative implications on quality of life for survivors.
The Movember foundation works to minimize the global impact of these dominant male cancers by funding initiatives and collaborating with innovative global organizations that promote education, early detection and personalized and affordable treatment.
 As a holistic men’s health organization, the Movember approach prioritizes mental health as much as physical. Globally, the male suicide rate is shockingly high, with one man dying by suicide every minute of every day, and 6 out of 10 suicides being committed by men (1).
As a holistic men’s health organization, the Movember approach prioritizes mental health as much as physical. Globally, the male suicide rate is shockingly high, with one man dying by suicide every minute of every day, and 6 out of 10 suicides being committed by men (1).
Movember examines and addresses the complex structural factors that contribute to the male suicide rate and keep men from speaking out and seeking help. “We provide men with the tools, avenues and resources to support and engage with their own mental health,” says Hermansen, “as well as ways to support one another.” By facilitating a global conversation surrounding male health and focusing on the three top health risks men currently face worldwide, Movember aims to reduce the number of men dying prematurely by 25% by the year 2030.
This November, there are 4 opportunities to get involved with Movember and contribute to men’s health.
1. Grow your own Mo and raise funds with your face
2. Run or walk 60 km as a part of Move for Movember in recognition of the 60 men lost to suicide each hour, every hour
3. Gather a group and Host a virtual Mo-Ment, and have a good time for a good cause
4. Design your own fundraising challenge and Mo Your Own Way.

Visit movember.com to learn more about men’s health and how to get involved, or to create a profile and start fundraising.
For more stories, visit Todayville Calgary.
Alberta
Alberta school boards required to meet new standards for school library materials with regard to sexual content

Alberta’s government has introduced new standards to ensure school library materials are age-appropriate.
School libraries should be safe and supportive places where students can learn and explore without being exposed to inappropriate sexual content. However, in the absence of a consistent standard for selecting age-appropriate library materials, school boards have taken different approaches, leading to concerns about safeguards in place.
In response to these concerns, and informed by feedback from education partners and the public, Alberta’s government has created standards to provide school boards with clear direction on the selection, availability and access to school library materials, such as books.
“Our actions to ensure that materials in school libraries don’t expose children to sexual content were never about banning books. These new standards are to ensure that school boards have clear guidance to ensure age-appropriate access to school library materials, while reflecting the values and priorities of Albertans.”
The new standards set clear expectations for school library materials with regard to sexual content and require school boards to implement policies to support these standards.
Standards for school library materials
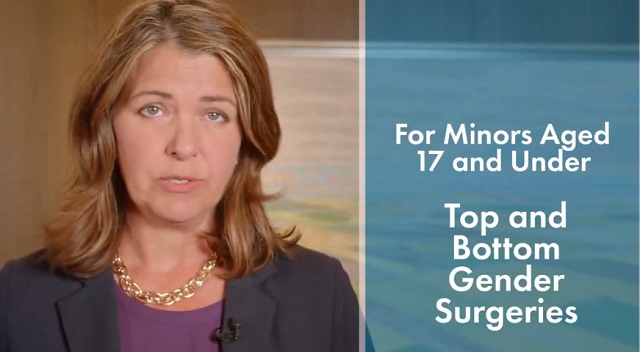
Under the new standards, school libraries are not permitted to include library materials containing explicit sexual content. Non-explicit sexual content may be accessible to students in Grade 10 and above, provided it is age-appropriate.
“Protecting kids from explicit content is common sense. LGBTQ youth, like all children, deserve to see themselves in stories that are age-appropriate, supportive and affirming – not in material that sexualizes or confuses them.”
School boards must also regularly review their school library collections, publish a full list of available materials and ensure that a staff member supervises students’ access to school library materials. School boards will have to remove any materials with explicit sexual content from their school libraries by October 1.
School board policies and procedures
All school boards must have publicly available policies that align with the new standards for selecting and managing library materials by January 1, 2026. School boards can either create new policies or update existing ones to meet these requirements.
These policies must outline how school library materials are selected and reviewed, how staff supervise students’ access throughout the school day, and how a student, parent, school board employee or other member of the school community can request a review or removal of materials in the school library. School boards are also required to clearly communicate these policies to employees, students and parents before January 2026.
“A robust, grade- and age-appropriate library catalogue is vital for student success. We welcome the ministry’s initiative to establish consistent standards and appreciate the ongoing consultation to help craft a plan that will serve our families and communities well.”
“Red Deer Public Schools welcomes the new provincial standards for school library materials. Our division is committed to maintaining welcoming, respectful learning spaces where students can grow and thrive. Under the new standards for school libraries, we remain dedicated to providing learning resources that reflect our values and support student success.”
Quick facts
- The new standards will apply to public, separate, francophone, charter and independent schools.
- The ministerial order does not apply to municipal libraries located within schools or materials selected for use by teachers as learning and teaching resources.
- From May 26 to June 6, almost 80,000 people completed an online survey to provide feedback on the creation of consistent standards to ensure the age-appropriateness of materials available to students in school libraries.
Related information
- Ministerial Order
- School library standards engagement
- Reference Materials: Content warning: this document contains graphic content that may be disturbing to viewers and is not appropriate for young viewers. Viewer discretion is advised.
Alberta
Fourteen regional advisory councils will shape health care planning and delivery in Alberta

Regional health councils give Albertans a voice
Albertans want a health care system that reflects where they live and adapts to the unique needs of their communities. As part of the province’s health care refocus, Alberta’s government committed to strengthening community voices by providing more opportunities for Albertans to bring forward their local priorities and offer input on how to improve the system.
The regional advisory councils, made up of 150 members from 71 communities, will advise Alberta’s four health ministries and the newly refocused health agencies: Primary Care Alberta, Acute Care Alberta, Assisted Living Alberta and Recovery Alberta. Each council will explore solutions to local challenges and identify opportunities for the health system to better support community decision-making.
“By hearing first-hand community feedback directly, we can build a system that is more responsive, more inclusive and ultimately more effective for everyone. I am looking forward to hearing the councils’ insights, perspectives and solutions to improve health care in all corners of our province.”
“Regional advisory councils will strengthen acute care by giving communities a direct voice. Their insights will help us address local needs, improve patient outcomes and ensure timely access to hospital services.”
“A ‘one-size-fits-all’ approach does not address unique regional needs when it comes to mental health and addiction challenges. These councils will help us hear directly from communities, allowing us to tailor supports and services to meet the needs of Albertans where they are.”
“Every community has unique needs, especially when it comes to seniors and vulnerable populations. These regional advisory councils will help us better understand those needs and ensure that assisted living services are shaped by the people who rely on them.”
Members include Albertans from all walks of life, health care workers, community leaders, Indigenous and municipal representatives, and others with a strong tie to their region. About one-third of members work in health care, and more than half of the council chairs are health professionals. Almost one-quarter are elected municipal officials, including 10 serving as chairs or vice-chairs. Ten councils also include a representative from a local health foundation.
Council members will share local and regional perspectives on health care services, planning and priorities to help ensure decisions reflect the realities of their communities. By engaging with residents, providers and organizations, they will gather feedback, identify challenges and bring forward ideas that may not otherwise reach government.
Through collaboration and community-informed solutions, members will help make the health system more responsive, accessible and better able to meet the needs of Albertans across the province.
“As Primary Care Alberta works to improve access to primary health care services and programs across Alberta, we are grateful to have the opportunity to tap into a dedicated group of community leaders and representatives. These people know their communities and local needs, and we look forward to learning from their experiences and knowledge as we shape the future of primary care in Alberta.”
“The regional advisory councils will help to bring forward the voices of patients, families and front-line providers from every corner of Alberta. Their insights will help us plan smarter and deliver care that’s timely, effective and truly local. We look forward to working closely with them to strengthen hospital and surgical services across the province.”
“Nobody understands the health care challenges unique to a community better than the people who live there. The regional health advisory councils are made up of those living and working on the front lines across the province, ensuring we are getting the perspective of Albertans most affected by our health care system.”
“Alongside Recovery Alberta’s staff and physician team, these regional advisory councils will build upon the high standard of mental health, addiction and correctional health services delivered in Alberta.”
Indigenous Advisory Council
Alberta’s government continues to work directly with Indigenous leaders across the province to establish the Indigenous Advisory Council to strengthen health care services for First Nation, Métis and Inuit communities.
With up to 22 members, including Indigenous health care workers, community leaders and individuals receiving health care services, the council will represent diverse perspectives across Alberta. Members will provide community perspectives about clinical service planning, capital projects, workforce development and cultural integration in health care.
Related information
-

 International2 days ago
International2 days agoSecret Service suspends six agents nearly a year after Trump assassination attempt
-

 Bruce Dowbiggin1 day ago
Bruce Dowbiggin1 day agoThe Covid 19 Disaster: When Do We Get The Apologies?
-

 Crime19 hours ago
Crime19 hours agoSweeping Boston Indictment Points to Vast Chinese Narco-Smuggling and Illegal Alien Labor Plot via Mexican Border
-

 Alberta1 day ago
Alberta1 day agoAlberta school boards required to meet new standards for school library materials with regard to sexual content
-

 Business2 days ago
Business2 days agoWEF-linked Linda Yaccarino to step down as CEO of X
-

 Automotive2 days ago
Automotive2 days agoAmerica’s EV Industry Must Now Compete On A Level Playing Field
-

 Environment20 hours ago
Environment20 hours agoEPA releases report on chemtrails, climate manipulation
-

 Business2 days ago
Business2 days ago‘Experts’ Warned Free Markets Would Ruin Argentina — Looks Like They Were Dead Wrong