Health
MAiD should not be a response to depression
This article supplied by Troy Media.
Canadians need real mental health support, not state-sanctioned suicide
If the law Parliament plans to roll out in 2027 had been on the books 15 years ago, Member of Parliament Andrew Lawton says he’d probably be dead. He’s not exaggerating. He’s referring to Canada’s scheduled expansion of medical assistance in dying (MAiD) to include people suffering only from mental illness.
Lawton, who survived a suicide attempt during a period of deep depression, knows what’s at stake. So do others who’ve shared similar stories. What they needed back then wasn’t a government-approved exit plan. They needed care, time, and something MAiD quietly discards: the possibility of recovery.
MAiD, medical assistance in dying, was legalized in Canada in 2016 for people with grievous and irremediable physical conditions. The 2027 expansion would, for the first time, allow people to request MAiD solely on the basis of a mental illness, even if they have no physical illness or terminal condition.
With the expansion now delayed to March 2027, Parliament will once again have to decide whether it wants to cross this particular moral threshold. Although the legislation was passed in 2021, it has never come into force. First pushed back to 2024, then to 2027, it remains stalled, not because of foot-dragging, but due to intense medical, ethical and public concern.
Parliament should scrap the expansion altogether.
A 2023 repeal attempt came surprisingly close—just 17 votes short, at 167 to 150. That’s despite unanimous support from Conservative, NDP and Green MPs. You read that right: all three parties, often at each other’s throats, agreed that death should not be an option handed out for depression.
Their concern wasn’t just ethical, it was practical. The core issues remain unresolved. There’s no consensus on whether mental illness is ever truly irremediable—whether it can be cured, improved or even reliably assessed as hopeless. Ask 10 psychiatrists and you’ll get 12 opinions. Recovery isn’t rare. But authorizing MAiD sends the opposite message: that some people’s pain is permanent, and the only answer is to make it stop—permanently.
Meanwhile, access to real mental health care is sorely lacking. A 2023 Angus Reid Institute poll found 40 per cent of Canadians who needed treatment faced barriers getting it. Half of Canadians said they outright oppose the expansion. Another 21 per cent weren’t sure—perhaps assuming Canada wouldn’t actually go through with something so dystopian. But 82 per cent agreed on one thing: don’t even think about expanding MAiD before fixing the mental health system.
That disconnect between what people need and what they’re being offered leads to a more profound contradiction. Canada spends millions promoting suicide prevention. There are hotlines, campaigns and mental health initiatives. Offering MAiD to people in crisis sends a radically different message: suicide prevention ends where bureaucracy begins.
Even Quebec, normally Canada’s most enthusiastic adopter of progressive policy experiments, has drawn the line. The province has said mental disorders don’t qualify for MAiD, period. Most provincial premiers and health ministers have called for an indefinite delay.
Internationally, the United Nations Committee on the Rights of Persons with Disabilities has condemned Canada’s approach and urged the government not to proceed. Taken together, the message is clear: both at home and abroad, there’s serious alarm over where this policy leads.
With mounting opposition and the deadline for implementation approaching in 2027, Parliament will again revisit the issue this fall.
A private member’s bill from MP Tamara Jansen, Bill C-218, which seeks to repeal the 2027 expansion clause, will bring the issue back to the floor for debate.
Her speech introducing the bill asked MPs to imagine someone’s child, broken by job loss or heartbreak, reaching a dark place. “Imagine they feel a loss so deep they are convinced the world would be better off without them,” she said. “Our society could end a person’s life solely for a mental health challenge.”
That isn’t compassion. That’s surrender.
Expanding MAiD to mental illness risks turning a temporary crisis into a permanent decision. It treats pain as untreatable, despair as destiny, and bureaucracy as wisdom. It signals to the vulnerable that Canada is no longer offering help—just a final form to sign.
Parliament still has time to reverse course. It should reject the expansion, reinvest in suicide prevention and reassert that mental suffering deserves treatment—not a state-sanctioned exit.
Daniel Zekveld is a Policy Analyst with the Association for Reformed Political Action (ARPA) Canada.
Explore more on Euthanasia, Assisted suicide, Mental health, Human Rights, Ethics
Troy Media empowers Canadian community news outlets by providing independent, insightful analysis and commentary. Our mission is to support local media in helping Canadians stay informed and engaged by delivering reliable content that strengthens community connections and deepens understanding across the country.
Health
RFK Jr’s argument for studying efficacy of various vaccines

From HHS Secretary Robert F Kennedy’s Facebook Page
Addictions
The War on Commonsense Nicotine Regulation

From the Brownstone Institute
Cigarettes kill nearly half a million Americans each year. Everyone knows it, including the Food and Drug Administration. Yet while the most lethal nicotine product remains on sale in every gas station, the FDA continues to block or delay far safer alternatives.
Nicotine pouches—small, smokeless packets tucked under the lip—deliver nicotine without burning tobacco. They eliminate the tar, carbon monoxide, and carcinogens that make cigarettes so deadly. The logic of harm reduction couldn’t be clearer: if smokers can get nicotine without smoke, millions of lives could be saved.
Sweden has already proven the point. Through widespread use of snus and nicotine pouches, the country has cut daily smoking to about 5 percent, the lowest rate in Europe. Lung-cancer deaths are less than half the continental average. This “Swedish Experience” shows that when adults are given safer options, they switch voluntarily—no prohibition required.
In the United States, however, the FDA’s tobacco division has turned this logic on its head. Since Congress gave it sweeping authority in 2009, the agency has demanded that every new product undergo a Premarket Tobacco Product Application, or PMTA, proving it is “appropriate for the protection of public health.” That sounds reasonable until you see how the process works.
Manufacturers must spend millions on speculative modeling about how their products might affect every segment of society—smokers, nonsmokers, youth, and future generations—before they can even reach the market. Unsurprisingly, almost all PMTAs have been denied or shelved. Reduced-risk products sit in limbo while Marlboros and Newports remain untouched.
Only this January did the agency relent slightly, authorizing 20 ZYN nicotine-pouch products made by Swedish Match, now owned by Philip Morris. The FDA admitted the obvious: “The data show that these specific products are appropriate for the protection of public health.” The toxic-chemical levels were far lower than in cigarettes, and adult smokers were more likely to switch than teens were to start.
The decision should have been a turning point. Instead, it exposed the double standard. Other pouch makers—especially smaller firms from Sweden and the US, such as NOAT—remain locked out of the legal market even when their products meet the same technical standards.
The FDA’s inaction has created a black market dominated by unregulated imports, many from China. According to my own research, roughly 85 percent of pouches now sold in convenience stores are technically illegal.
The agency claims that this heavy-handed approach protects kids. But youth pouch use in the US remains very low—about 1.5 percent of high-school students according to the latest National Youth Tobacco Survey—while nearly 30 million American adults still smoke. Denying safer products to millions of addicted adults because a tiny fraction of teens might experiment is the opposite of public-health logic.
There’s a better path. The FDA should base its decisions on science, not fear. If a product dramatically reduces exposure to harmful chemicals, meets strict packaging and marketing standards, and enforces Tobacco 21 age verification, it should be allowed on the market. Population-level effects can be monitored afterward through real-world data on switching and youth use. That’s how drug and vaccine regulation already works.
Sweden’s evidence shows the results of a pragmatic approach: a near-smoke-free society achieved through consumer choice, not coercion. The FDA’s own approval of ZYN proves that such products can meet its legal standard for protecting public health. The next step is consistency—apply the same rules to everyone.
Combustion, not nicotine, is the killer. Until the FDA acts on that simple truth, it will keep protecting the cigarette industry it was supposed to regulate.
-

 Business1 day ago
Business1 day agoTrans Mountain executive says it’s time to fix the system, expand access, and think like a nation builder
-
 International1 day ago
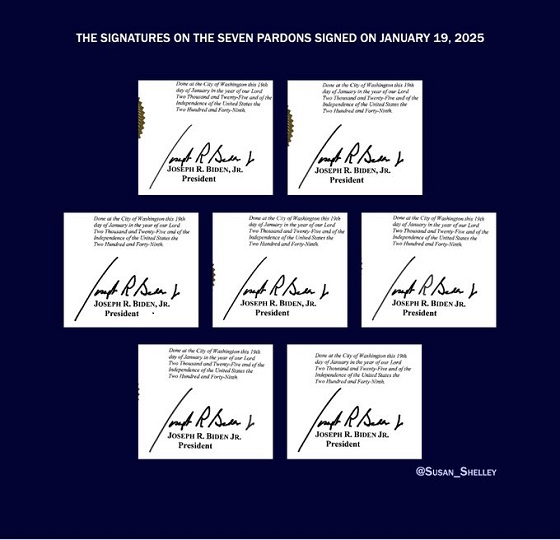
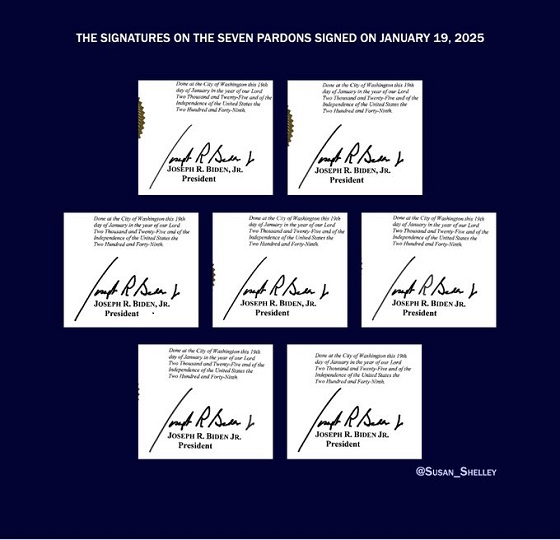
International1 day agoBiden’s Autopen Orders declared “null and void”
-

 MAiD1 day ago
MAiD1 day agoStudy promotes liver transplants from Canadian euthanasia victims
-

 Business1 day ago
Business1 day agoCanada has given $109 million to Communist China for ‘sustainable development’ since 2015
-

 Internet1 day ago
Internet1 day agoMusk launches Grokipedia to break Wikipedia’s information monopoly
-

 Business1 day ago
Business1 day agoCanada’s combative trade tactics are backfiring
-

 Automotive1 day ago
Automotive1 day agoCarney’s Budget Risks Another Costly EV Bet
-

 Business1 day ago
Business1 day agoYou Won’t Believe What Canada’s Embassy in Brazil Has Been Up To