Crime
“A Dangerous Experiment”: Doctor Says Ideological Canadian Governments Ignored Evidence as Safer Supply Exacerbated Fentanyl Death Surge
Dr. Lori Regenstreif warns: No other country would hand bottles of opioids to addicts ‘with the assumption that this will solve their risk of overdose death’
A scathing new study by a Canadian addictions physician concludes that ideologically driven “social justice” governments have worsened the country’s fentanyl crisis by aggressively funding and promoting so-called “safer supply” programs—despite a lack of evidence they save lives. Instead, as mounting proof showed that thousands of government-distributed opioid tablets—as potent as heroin—were being diverted into the black market by organized crime, Health Canada, public health officials, and sympathetic media outlets continued to defend the controversial programs and attack critics.
Even as violent incidents emerged—including a shooting outside a Toronto safer supply clinic—the study notes that some advocates called for medical professionals to be removed from program oversight entirely.
In a paper published by the Macdonald-Laurier Institute, Dr. Lori Regenstreif, a veteran addictions physician, argues that Canada’s “safe supply” programs—widely expanded after 2019—have not only failed to reduce overdose deaths, but have coincided with a steep rise in fatalities. The number of opioid-related deaths in Canada surged from 3,023 in 2016 to more than 7,300 by 2021, despite increased distribution of government-supplied hydromorphone tablets. Regenstreif warns that the policy, intended as harm reduction, has morphed into a dangerous social justice experiment, sidelining evidence-based treatments like methadone and buprenorphine in favour of unproven, unsupervised opioid dispensing.
What Canada has chosen to do to address opioid overdose is unique, Regenstreif states of her findings, released today.
“No other country would envision a policy in which people with opioid addiction are simply given bottles of opioid pills with the assumption that this will solve their risk of overdose death.”
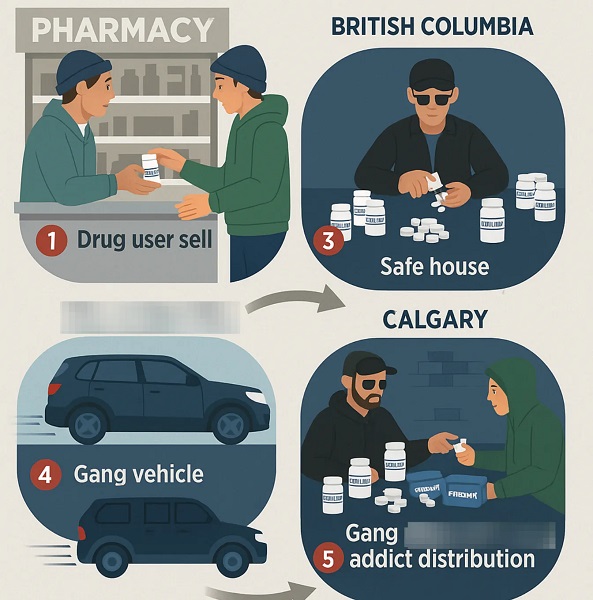
Instead of curbing fatalities, safe supply programs have unleashed a wave of diversion—with powerful 8mg hydromorphone tablets, known on the street as “Dillies,” leaking into illicit markets and being trafficked across the country. She cites a growing body of evidence, also covered in reports from The Bureau, that these pills are not only widely sold and traded by program participants, but also used as currency by organized crime groups.
Cited in the study, like-minded addiction experts Dr. Sharon Koivu and Dr. Jenny Melamed report that the street price of Dilaudid 8mg tablets collapsed from $15–$20 in 2020 to as low as $0.50 by late 2021. “Things changed within weeks of the hydromorphone hitting the streets,” Melamed said. This sudden flood of pharmaceutical-grade opioids reshaped local drug economies—allowing criminal networks to exploit the government-funded supply chain and expand access to hard opioids far beyond clinical settings.
Regenstreif also highlights systemic flaws in the program’s implementation. Staff at supervised injection sites often appeared well-meaning, but lacked clinical experience and a clear understanding of untreated addiction behaviour.
“They did not grasp the constant pressure felt by users to acquire more drugs, money, or other currency to maintain use.”
One notable case cited in the report occurred in 2023, when a peer support worker at the Parkdale Community Health Centre in Toronto was implicated in a shooting incident.
“A peer support worker, perhaps with naïve but good intentions, ended up on the wrong side of the law in attempting to protect a safe consumption site client involved in a shooting,” Regenstreif writes.
Yet despite such outcomes, advocates continued to push for a “non-medicalized” model of opioid distribution, in which trained addiction specialists were sidelined.
Regenstreif traces how media coverage of the safer supply programs has shifted in tone amid growing investigative scrutiny and backlash from program advocates and public health officials.
Health Canada is described as having dismissed or re-framed concerns over diversion. One federally funded guidance document, titled Re-Framing Diversion for Health Care Providers, argued that diversion should not be stigmatized. “The current medical and criminal-legal framing of diversion perpetuates stigmatizing and patronizing views of people who use drugs,” the document reads.
The Globe and Mail’s Andrea Woo wrote in 2024 citing British Columbia’s Coroners Service and noting no definitive link between prescribed safe supply and overdose deaths. However, Regenstreif points out that coroners cannot determine how a victim first encountered opioids—only which drug was in their system at death. “A coroner cannot determine if the opioid came from a diverted prescription,” she writes.
National Post contributor Adam Zivo—who has reported on diversion for The Bureau—was among the first to investigate pill diversion in 2023, interviewing clinicians who used pseudonyms due to fear of backlash. The study cites his reporting in describing a pattern: as police across the country seized tens of thousands of prescription opioid pills, and more physicians documented evidence of diversion, the research field remained notably shallow. Meanwhile, advocates of safe supply programs politicized the issue, accusing critics of inciting a “moral panic” and aligning with entrenched institutional interests.
Regenstreif contends that it is frontline addiction physicians—those treating users of fentanyl and working within the safer supply framework—who are best placed to assess its consequences. She recounts one patient under 18 describing a visit to a Burlington, Ontario clinic, where they saw a doctor only on video and were handed a bottle of Dilaudid. Others reported buying diverted Dilaudid bottles openly on the streets of Peterborough, Thunder Bay, and Windsor in Ontario, or Victoria and Nanaimo in British Columbia.
Not all supporters of the program are acting in bad faith, Regenstreif notes, but many fail to see the bigger picture. Addiction specialists, public health officials, and researchers have each addressed isolated elements of the crisis based on their particular lens—yet none have managed to bring these perspectives together into an effective, unified response.
Corroborating Canadian reports, the U.S. Drug Enforcement Administration identifies hydromorphone—marketed as Dilaudid—as a drug of interest to traffickers, producing effects similar to heroin and fentanyl. The DEA lists common street names such as “D,” “Dillies,” “Dust,” “Footballs,” “Juice,” and “Smack,” and warns that diversion occurs through forged prescriptions, doctor-shopping, and pharmacy theft—risks compounded by unmonitored safe supply systems.
In her conclusion, Regenstreif warns that comparing opioids to alcohol, as some safe supply advocates do, is a false analogy. Alcohol’s harms accumulate gradually; opioids, by contrast, are acutely toxic and deadly. Canada must chart a better path forward, she argues—one that prioritizes evidence-based care, not ideological narratives. That path includes a return to opioid agonist therapy and wraparound services; genuine adherence to medical science; balancing individual and community well-being; and reuniting the four pillars of Canada’s drug strategy: prevention, treatment, harm reduction, and enforcement.
The Bureau is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Invite your friends and earn rewards
Crime
Inside the Fortified Sinaloa-Linked Compound Canada Still Can’t Seize After 12 Years of Legal War

Exclusive analysis shows how a fortified Surrey mansion tied in court filings to the Sinaloa Cartel’s leader has become the core of a stalled civil forfeiture fight, exposing Canada’s weak laws.
A British Columbia government lawsuit seeks to merge almost a decade of litigation into a single, high-stakes test of whether the province can finally seize a fortified mansion near the U.S. border that was first swept up in a 2014 fentanyl investigation, raided in 2016, and is now at the center of a new synthetic-opioid case alleging its occupants contracted with the leader of Mexico’s Sinaloa Cartel to flood narcotics into Canada.
In a notice of application filed in November 2025, the Director of Civil Forfeiture argues that all of the files revolve around one owner — James Sydney Sclater — and his flagship property on 77th Avenue, a multi-million-dollar house about twenty minutes’ drive from the Peace Arch crossing.
The property became newly notorious this spring when the latest effort to seize it pulled back the curtain on a 2024 RCMP raid. Officers say they entered a mansion ringed by compound fencing, steel gates and razor wire, wired with Chinese-made Hikvision surveillance cameras and hardened doors.
Inside, they reported finding hidden compartments in bedrooms and a basement bathroom packed with counterfeit pills and kilograms of raw synthetic opioids — including fentanyl — while assault-style rifles with screw-on suppressors, thousands of bullets and other firearms and body armour were stored in ways that suggested the residents were prepared for urban warfare. Investigators later alleged the targets had “connections to virtually every criminal gang in British Columbia.”
They also seized travel documents, including Mexican visas, before tracing the operation to alleged negotiations with Ismael “El Mayo” Zambada García, the reputed head of the Sinaloa Cartel, which Ottawa has now listed as a terrorist entity.
But for Canadian anti-mafia units, the address tracks the history of fentanyl’s deadly sweep across British Columbia, among the hardest-hit opioid death zones in North America. Their interest in the Surrey mansion stretches back to the first wave of lethal fentanyl trafficking that surged from Vancouver’s Downtown Eastside to Victoria and Vancouver Island around 2013 — making this single property a through-line in the North American opioid crisis, one that now runs through senior offices in Washington, Mexico City, Beijing and Ottawa.
Behind the hundreds of pages of civil filings reviewed by The Bureau lies a failure of governance as urgent as the unchecked advance of Latin cartels into Canadian cities — and as lethal as the synthetic opioids tied to the Surrey home.
British Columbia has been chasing the same house, and the same alleged transnational traffickers, through raids, affidavits and Charter of Rights battles since before fentanyl became a household word — and still has not managed to take the keys away.
The case documents explicitly point to a criminal-defence-friendly Supreme Court of Canada ruling — Stinchcombe, notoriously cited by police leaders — and to its role in undermining numerous major prosecutions involving networks tied to alleged narcoterror suspect Ryan Wedding and modern Canadian fentanyl-lab operators. One of those networks is the Wolfpack, a hybrid of Mexican cartels, Middle Eastern threat networks and biker gangs said to be supplied by Chinese Communist Party–linked criminal organizations and other Latin American cartel interests.
For the Director, the newest chapter begins in earnest with an RCMP raid on September 23, 2024. By then, investigators say, the Surrey mansion was no longer a domestic drug base, but the Canadian end of a supply line reaching into Sinaloa itself. Notably, 38 days later, on October 31, the RCMP announced a separate raid on what U.S. sources describe as the largest fentanyl lab ever discovered in the world, in rugged Falkland, B.C., roughly halfway between Vancouver and Calgary.
“The combined fentanyl and precursors seized at this facility could have amounted to over 95,500,000 potentially lethal doses of fentanyl, which have been prevented from entering our communities, or exported abroad,” the Mounties said.
But Sinaloa does not appear out of nowhere in the Surrey compound. The older case that the Director now wants consolidated onto the same track reaches back to a different phase of the crisis — and sketches an earlier incarnation of the Surrey house as a node in a Lower Mainland fentanyl network.
According to a 2019 notice of civil claim filed in the Victoria registry, the RCMP’s Project E-Probang began in November 2014, targeting a chemical narcotics distribution network that operated across the Lower Mainland and Vancouver Island. At the centre of that probe, police say, was Nicholas Lucier and his associates. The Director alleges that Sclater supplied Lucier’s network with controlled substances, while his father-in-law Gary Van Buuren lived with him at the 77th Avenue property and “assisted him in trafficking of controlled substances.”
The narrative that follows reads like a blueprint for mid-2010s fentanyl tradecraft. In October 2016, Lucier associate Yevgeniy Nagornyy-Kryvonos allegedly drove to the Surrey mansion to receive fentanyl from Sclater. Two days later, Nagornyy-Kryvonos met Daemon Gariepy; Gariepy was arrested shortly after that meeting, with one kilogram of fentanyl in his possession. On November 6, 2016, Sclater and Van Buuren visited the Surrey home of another associate, Azam Abdul. Van Buuren was picked up soon afterwards, allegedly carrying a kilogram of methamphetamine, a kilogram of fentanyl and two cellphones.
That same day, RCMP officers moved in on 16767 77th Avenue with a warrant. Inside, according to the pleadings, they found the kind of infrastructure that exists to supply major drug lines: long guns and improvised weapons scattered through the house, from conventional shotguns and rifles to a deactivated grenade, brass knuckles and a small armoury of knives, batons and throwing stars. There was a money counter parked near vacuum-sealing equipment; shelves of drug-packaging and currency-bundling materials; a body armour vest; and a banknote stash of roughly $20,000 in twenties, bundled with elastic bands and tucked into vacuum-sealed bags.
Fentanyl-containing pills and scoresheets documenting transactions sat alongside a multi-monitor surveillance system and a wiretap-detection kit. In a separate corner, tax records in Sclater’s name showed his declared income stepping down from more than $77,000 in 2010 to just over $11,000 by 2014 — data points that undermined his ability to carry mortgages on two Surrey properties.
The days that followed widened the picture.
A search at Abdul’s residence turned up scales, fentanyl and the tools of drug production and processing. Raids at Lucier’s home and two rentals he allegedly used produced what the Director describes as a haul worth a serious cartel’s attention: weapons and ammunition, more than $2-million in cash, and “thousands of grams” of fentanyl, cocaine, methamphetamine, a heroin-fentanyl mixture, fentanyl “oxy” tablets and MDMA, along with the scoresheets and processing gear that underpin a wholesale operation.
On Vancouver Island, an arrest search of Lucier allegedly produced tens of thousands of dollars in cash and multiple phones.
Lucier had been on Canadian police radar since at least the mid-2000s, and his story intertwines with the murder of B.C. cocaine broker Tom Gisby in Mexico — a killing that, according to a Canadian police source interviewed by The Bureau, formed part of a bloody consolidation of Mexican cartel power over Vancouver’s drug markets.
Lucier’s notoriety stretches back to October 2009, when Victoria police announced what they described as the city’s largest-ever cocaine bust. After a three-month undercover probe triggered by a shooting near Beacon Hill Park, nearly 100 officers carried out pre-dawn raids on five locations around the capital region, seizing roughly 22.5 kilograms of cocaine, four high-powered handguns, two vehicles and about $420,000 in cash. Lucier, then 41 and already on parole from a 2007 trafficking sentence involving multi-kilogram quantities of cocaine and heroin, was the lone suspect to slip away; a Canada-wide warrant was issued for his arrest.
In 2012, police in Mexico’s Nayarit state announced they had arrested Lucier in the Pacific resort city of Nuevo Vallarta on the outstanding Canadian warrant — the same town where Gisby, a longtime player in British Columbia’s cocaine trade, had been shot dead days earlier while ordering coffee at a Starbucks. Mexican authorities said Lucier had been living under an assumed name and socializing with other Canadian expatriates in the Puerto Vallarta area, including people who knew Gisby, although his arrest was not believed to be directly tied to the murder.
For investigators, the episode underscored how Canadian traffickers were deeply embedded in Mexican resort corridors from Mazatlán to Cancún that doubled as hubs for cartel-linked players from the north. In the years that followed, it would be former Canadian snowboarder Ryan Wedding — tightly associated with the Wolfpack networks tied to Western Canada’s fentanyl superlabs — who, according to U.S. government sources, rose above other Canadian narcos in those resort towns to become perhaps the single conduit for Latin American–supplied narcotics imported into Canada for both domestic consumption and onward transshipment.
The Bureau is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
No Charges on Fentanyl Network
E-Probang era investigations underpin the 2019 civil claim that seeks forfeiture of both the 77th Avenue mansion and a second property at 15797 92nd Avenue. The Director’s position is that the homes were purchased and maintained with money that cannot be reconciled with Sclater’s reported earnings and should be treated as the proceeds of crime.
According to an amended notice of civil claim filed in May 2025, Sclater shared the 77th Avenue house with Hector Armando Chavez-Anchondo and John Brian Whalen, while Whalen’s father, John Edwin Whalen, and Brittany Anne Horvey are drawn into the case through their alleged roles in what the Director calls a drug trafficking organization, or DTO. The court filings describe not a loose circle of dealers, but a structured group that trafficked ketamine, methamphetamine, counterfeit Xanax, oxycodone, MDMA and fentanyl, and that “since June 2021 at the latest” had been working to import bulk cocaine from Mexico.
As the Director tells it, those efforts led straight to Sinaloa itself. The Surrey group is alleged to have agreed to purchase cocaine from senior cartel suppliers — operating at such scale, sophistication and power within Canada that they ultimately negotiated directly with alleged cartel boss Ismael “El Mayo” Zambada García.
When U.S. authorities arrested El Mayo on July 25, 2024, the Surrey operation is said to have lurched sideways, searching for “other parties” to keep the cocaine pipeline alive. In early September, Sclater, Chavez-Anchondo and Whalen Jr. allegedly pooled money to secure a shipment, then drove out to a rendezvous where they expected to collect their imported cocaine. According to the filings, their transport contact never materialized, and they returned to Surrey empty-handed.
Eleven days later, the RCMP arrived with a search warrant. Inside the mansion, officers reported walking into what looked more like a mid-level cartel outpost than a suburban home: firearms racked and stashed in multiple rooms, including assault-style rifles with screw-on suppressors and piles of ammunition, suggesting residents lived with the expectation of raids or perhaps clashes with some of the six other Mexican cartel networks aside from Sinaloa that have been identified in Canada by federal police.
Hidden compartments had been carved into bedrooms and a basement bathroom, where police say they found kilogram-scale quantities of ketamine and methamphetamine, counterfeit alprazolam tablets pressed to resemble Xanax, hundreds of oxycodone pills, a smaller but potent stash of fentanyl, and bundles of Canadian cash tucked away in a manner seasoned investigators instantly recognized — elastic-bound bricks, some vacuum-sealed, packed tightly enough to hint at far more money moving through the house than Sclater’s tax returns would ever show.
Downstairs, a kitchen freezer allegedly doubled as a storage vault for nearly a kilogram of MDMA; elsewhere, RCMP catalogued an Azure pleasure boat, a stable of trucks and custom motorcycles, gold jewellery and two Hikvision digital-video recorders that formed the core of a security system surveying the compound. The Director’s case is that neither Sclater nor his co-defendants had legitimate income capable of supporting that lifestyle, and that the house was both the proceeds and instrument of unlawful activity.
The timing was not incidental. Ottawa formally listed the Sinaloa Cartel as a terrorist entity on February 20, 2025, as one of seven Latin American criminal organizations added to Canada’s Criminal Code list in response to the fentanyl crisis and mounting U.S. pressure.
The Director’s pleadings lean into that backdrop, explicitly calling Sinaloa a terrorist entity and portraying 16767 77th Avenue as part of the infrastructure of a cartel now placed at the centre of a transnational security crisis.
While the alleged facts of police raids against the Surrey mansion seem to move steadily, the apparent lack of criminal charges against any of the targets — let alone a racketeering-style case against the network itself, which is effectively impossible to mount in Canada, where there is no U.S.-style RICO statute — reveals a litigation record that can fairly be described as broken and ineffectual, except from the perspective of criminal-defence lawyers and their clients.
The Director’s Victoria-based action was filed on May 22, 2019.
Sclater responded months later, disputing the forfeiture. In December 2019, the province produced its list of documents. Sclater replied in January 2020 with a list that named no documents at all. Over the next two years, Crown counsel sent a steady stream of letters — in March 2020, August 2021, and repeatedly between October 2021 and March 2022 — demanding a proper list and the financial and property records that would show how Sclater funded his holdings.
In a 2022 application, the Director’s frustration spilled onto the record. The submission notes that under the Civil Forfeiture Act, the core question is whether the Surrey properties are proceeds or instruments of unlawful activity — and that without basic financial disclosure, there is no way to test Sclater’s claim that they were acquired lawfully. The Director points out that documents showing income sources, mortgage servicing, and the acquisition and storage of weapons “are critical to a determination of the action on its merits,” and accuses Sclater of refusing or neglecting, for almost three years, to meet even the baseline disclosure duties imposed by the civil-procedure rules.
To head off what it casts as an attempt to turn the case into a criminal-style disclosure standoff, the Director leans on British Columbia v. PacNet Services Ltd., where the court rejected defence arguments that tried to graft the Supreme Court’s Stinchcombe-era criminal disclosure standards onto civil forfeiture proceedings. R. v. Stinchcombe — the 1991 Supreme Court of Canada decision that imposed a broad duty on the Crown to disclose all potentially relevant information so an accused can make full answer and defence under section 7 of the Charter — is firmly rooted in criminal procedure. Echoing that line of authority, the Director argues that there is “no justification” for Sclater to shelter behind Stinchcombe to avoid producing his own financial and property records, and tells the court it is “time to move [the case] forward,” with full document production or a lawful explanation for the default.
The Bureau is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Constitutional Test
The newer Sinaloa-linked file adds another layer of complexity. Four of the five named defendants — Chavez-Anchondo, the two Whalens and Horvey — have not filed responses. In a separate notice of application, the Director now asks the court to treat the core allegations against them as admitted by default: that they were members of a drug trafficking organization; that they used or threatened violence; that they trafficked a catalogue of synthetic drugs and opioids; that they negotiated with Sinaloa; and that the weapons, cash and assets found in the 2024 raid are instruments and proceeds of crime.
For his part, Sclater is trying to turn the Surrey files into a constitutional test case. In his latest defence, he claims a lawful ownership interest in the 77th Avenue property, certain vehicles, cash, jewellery and electronic devices, and denies every allegation that he joined a criminal organization, conspired to import cocaine from Mexico, or negotiated with El Mayo. He acknowledges having a criminal record but disputes the particulars, and insists he had sufficient legitimate income to fund his properties and toys.
More ambitiously, he argues that the Civil Forfeiture Act itself is unconstitutional. By using allegations that he failed to declare taxable income as part of the proceeds-of-crime theory, he says, the province is encroaching on the federal government’s exclusive power over taxation under the Constitution Act, 1867. Assessing taxes owed, he points out, is the business of the Minister of National Revenue and the Tax Court of Canada. Civil forfeiture, in his view, cannot be used as a kind of shadow tax audit. He also asserts that the case “has arisen solely” from breaches of his Charter rights by RCMP officers and other state actors, arguing that the Director — “also an agent of the state” — is improperly relying on those breaches in seeking forfeiture.
It is, in effect, a bid to turn a forfeiture trial about a Surrey mansion into a referendum on how far provincial authorities can go in dismantling alleged drug networks without turning civil litigation into a criminal prosecution by another name.
All of this is unfolding against a national and continental backdrop that makes the Surrey house look less like an isolated problem than a symbol of a wider national failure.
Under National Fentanyl Sprint 2.0, Canadian police and partner agencies seized 386 kilograms of fentanyl and analogues between May 20 and October 31, 2025, with Ontario and British Columbia accounting for more than 90 per cent of that total. British Columbia reported 88 kilograms of seized fentanyl during the sprint. Yet those numbers miss some of the most alarming data points. Just days before the sprint window opened, Canada Border Services Agency officers at the Tsawwassen container facility in Delta intercepted more than 4,300 litres of chemicals from China, including 500 litres of propionyl chloride — a direct fentanyl precursor — and other substances capable of feeding clandestine labs in the Canadian wilderness for years. That shipment was destined for Calgary, and conservative estimates suggest it could have yielded enough fentanyl for billions of potentially lethal doses.
The Carney government continues to insist that Canada is primarily an end market, not a major exporter, and CBSA officials emphasize that only “small, personal doses” of finished fentanyl are being found heading south.
Seen from that angle, the fight over one Surrey mansion and the man who owns it becomes more than a story of Mexican cartels embedding in British Columbia’s wealthy suburbs.
It is a test of whether Canada’s patchwork of civil forfeiture laws, criminal prosecutions and Charter-driven disclosure rules can keep pace with transnational networks that blend Chinese chemical suppliers, Mexican cartels and domestic labs into a single system. For now, many Canadian police experts acknowledge in private — and some senior leaders flag in cautious public statements — that this test is being failed, and failed egregiously.
The Bureau is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
Crime
Vancouver police seize fentanyl and grenade launcher in opioid-overdose crisis zone

Vancouver police say they have seized a grenade launcher, four guns, and nearly 500 grams of fentanyl and other hard drugs from a fortified Downtown Eastside rooming house that was allegedly feeding a synthetic opioid supply line through the city’s most drug-ravaged blocks.
“Task Force Barrage has come to an end, but our work to curb violence and disrupt organized crime in the Downtown Eastside continues,” Sergeant Steve Addison said, adding “the proliferation of violence and weapons in some residential buildings continues to put the neighbourhood at risk.”
The latest investigation began November 13, when a 42-year-old man suffered serious injuries in an assault near Carrall Street and East Cordova and was taken to hospital. Officers followed leads to a rooming house at 50 East Cordova Street, in the heart of a street-level open drug market that has become notorious in photos and news clips around the world.
On November 18, police say they uncovered a stockpile of illicit drugs, guns and weapons in three rooms of the East Cordova building. According to Addison, there are signs that parts of the property, which is supposed to house low-income residents, were repurposed as a hub to store weapons and distribute contraband throughout the neighbourhood, with some areas “fortified with countersurveillance measures to avoid detection from law enforcement.”
Items seized include four firearms, two imitation guns, a grenade launcher, a firearm suppressor, seven machetes, four flare guns, bullwhips, baseball bats, body armour, handcuffs and ammunition. Officers also seized 486 grams of fentanyl, cannabis, Dilaudid pills and methamphetamine – a quantity police say represents more than 2,500 single doses.
Meanwhile, in a separate update posted November 26 — the day before VPD announced the Cordova Street raid — Vancouver Fire Rescue Services said that on Tuesday, November 21, firefighters responded to 54 overdoses, the highest single-day total in the department’s history. The service said it averaged about 16 overdose calls per day in May, but that figure has surged in recent weeks, and during the most recent income-assistance week, firefighters were averaging roughly 45 overdose responses per day.
While police have not publicly linked the East Cordova seizure to any specific cartel, the mix of fentanyl, fortified real estate and a small armoury of weapons closely tracks the profile of a separate, high-profile British Columbia case in which provincial authorities say a Sinaloa Cartel–aligned cell embedded itself just south of Vancouver.
In that case, a civil forfeiture lawsuit alleged a Sinaloa Cartel–linked fentanyl and cocaine trafficking group set up in a multi-million-dollar mansion near the U.S. border, capable of negotiating major cocaine import deals with Ismael Garcia—known as “El Mayo”—the reputed Sinaloa Cartel chief. According to the filings, the Canada-based syndicate involved at least three men, and belonged to a violent drug trafficking organization that “used and continues to use violence, or threats of violence, to achieve its aims.”
Investigators alleged the Surrey-based group trafficked ketamine, methamphetamine, Xanax, oxycodone, MDMA and fentanyl. “As part of these efforts, the drug trafficking organization has agreed to, and made arrangements to, purchase cocaine from the Cártel de Sinaloa in Mexico,” the filings stated. They added: “the Sinaloa Cartel is a terrorist entity, and the government of Canada listed it as such on February 20, 2025.”
RCMP said they uncovered a substantial cache of weapons and narcotics during a search of the Surrey property on 77th Avenue on September 23, 2024. Opioids seized from the mansion included 400 grams of counterfeit Xanax, 810 oxycodone pills, 5.5 grams of fentanyl and nearly a kilogram of Ecstasy. The province is now seeking forfeiture of the house, which sits about 20 minutes from the Peace Arch border crossing north of Seattle.
Court submissions detailed an arsenal of 23 weapons – ten handguns, two sawed-off shotguns, two hunting rifles, seven assault rifles (two reportedly fitted with screw-on suppressors), and a speargun – alongside about 3.5 kilograms of ketamine and methamphetamine hidden in a compartment in one suspect’s room, hundreds of counterfeit alprazolam pills, a stash of oxycodone, and nearly CAD 15,000 in bundled cash “not consistent with standard banking practices.”
Viewed together, the Downtown Eastside raid and the Surrey mansion case sketch out different ends of what appears to be the same continuum, ultimately pointing to senior criminal leaders in Mexico and China.
The Bureau is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
-

 Bruce Dowbiggin17 hours ago
Bruce Dowbiggin17 hours agoIntegration Or Indignation: Whose Strategy Worked Best Against Trump?
-

 COVID-1918 hours ago
COVID-1918 hours agoUniversity of Colorado will pay $10 million to staff, students for trying to force them to take COVID shots
-

 Energy2 days ago
Energy2 days agoCanada following Europe’s stumble by ignoring energy reality
-

 Banks2 days ago
Banks2 days agoTo increase competition in Canadian banking, mandate and mindset of bank regulators must change
-

 Business2 days ago
Business2 days agoLoblaws Owes Canadians Up to $500 Million in “Secret” Bread Cash
-
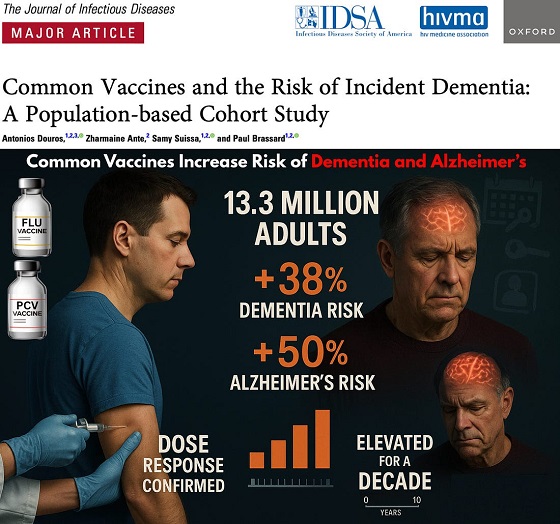
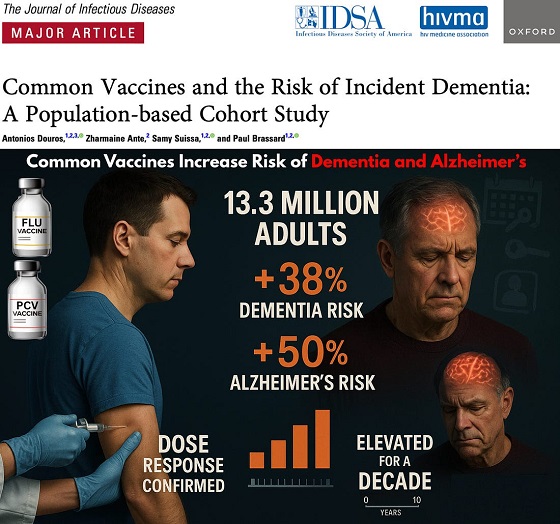 Focal Points2 days ago
Focal Points2 days agoCommon Vaccines Linked to 38-50% Increased Risk of Dementia and Alzheimer’s
-
 Opinion2 days ago
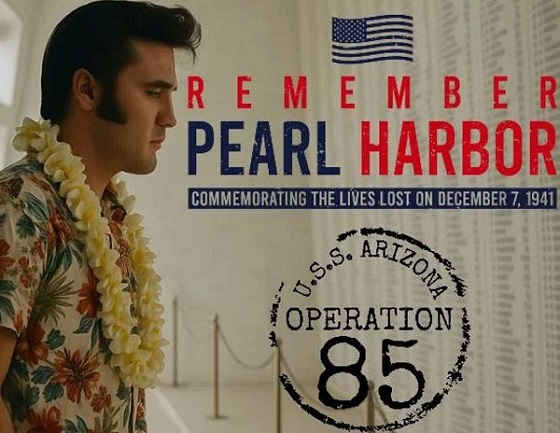
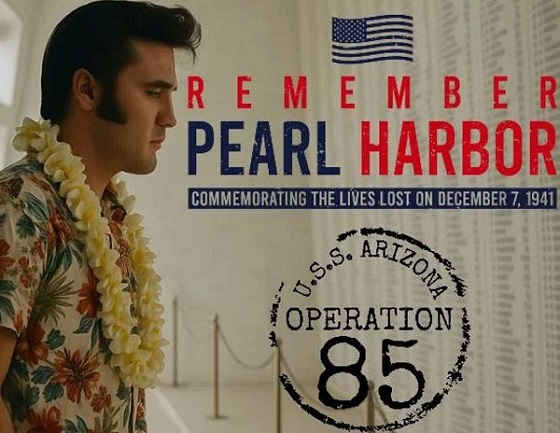
Opinion2 days agoThe day the ‘King of rock ‘n’ roll saved the Arizona memorial
-

 espionage1 day ago
espionage1 day agoWestern Campuses Help Build China’s Digital Dragnet With U.S. Tax Funds, Study Warns