Health
How the once-blacklisted Dr. Jay Bhattacharya could help save healthcare

From LifeSiteNews
Now seated at the helm of the National Institutes of Health, Dr. Jay Bhattacharya is poised to reshape not only the agency’s research priorities but the very culture that pushed him to the fringe.
Imagine spending your career studying infectious diseases, only to find that the real virus spreading uncontrollably is censorship. That was the reality for Dr. Jay Bhattacharya, a Stanford epidemiologist who committed the unpardonable sin of questioning the COVID-19 lockdown orthodoxy. His punishment? Digital exile, courtesy of Silicon Valley’s Ministry of Truth.
In December 2022, the Twitter Files exposed what many had long suspected: Twitter had quietly placed Bhattacharya’s account on a Trends Blacklist. This ensured that his posts, often critical of lockdowns and mask mandates, would never see the light of day on the platform’s trending topics. In other words, Twitter’s algorithm worked like a digital bouncer, making sure his dissenting opinions never made it past the velvet rope.

And Twitter wasn’t alone. Facebook, ever eager to please its government handlers, scrubbed the Great Barrington Declaration from its pages. That document, co-authored by Bhattacharya and other esteemed scientists, dared to suggest that maybe, just maybe, locking down entire populations wasn’t the best strategy. Instead, it proposed focused protection for the most vulnerable while allowing the rest of society to function. For this, it was sent to the digital equivalent of a gulag.
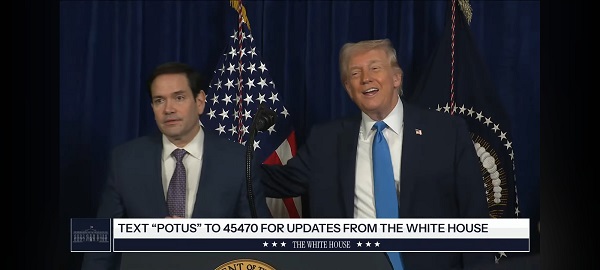
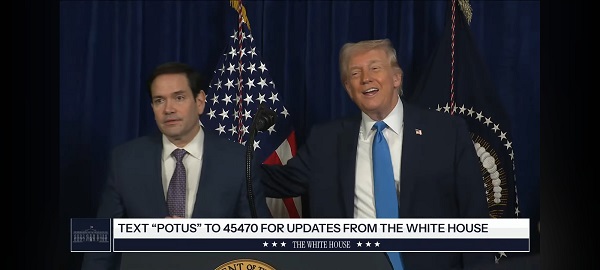
These experiences took center stage during Bhattacharya’s Senate confirmation hearing for the directorship of the National Institutes of Health (NIH). Republican lawmakers, who suddenly found themselves cast as the last defenders of free speech in scientific discourse, saw his nomination as a win.
During his testimony, Bhattacharya didn’t mince words. He detailed how the Biden administration played an active role in orchestrating the suppression of alternative views. It wasn’t enough for officials to push their own pandemic policies — they needed to ensure that no one, regardless of expertise, could challenge them in the public square.
The Science™ vs. The Science
Bhattacharya’s testimony laid bare an uncomfortable truth: the pandemic was a crisis of speech. “The root problem was that people who had alternative ideas were suppressed,” he told Sen. Ashley Moody (R-Fla.). “I personally was subject to censorship by the actions of the Biden administration during the pandemic.”
In a functioning society, that statement would spark bipartisan outrage. Instead, it barely registered. The people who spent years chanting “trust the science” were never interested in science at all.
Real science thrives on debate, skepticism, and the understanding that no single expert — no matter how credentialed—holds absolute truth. But during COVID, science became The Science™ — a government-approved doctrine enforced by Silicon Valley moderators and federal bureaucrats. Deviate from it, and you weren’t just wrong. You were dangerous.
A government-sanctioned muzzle
Bhattacharya wasn’t silenced in some haphazard, accidental way. The Biden administration actively leaned on social media companies to “moderate” voices like his. In practice, that meant tech executives — most of whom couldn’t tell a virus from a viral tweet — decided which epidemiologists the public was allowed to hear.
He responded with a lawsuit against the administration, accusing it of colluding with Big Tech to crush dissent. But in a ruling as predictable as it was revealing, the Supreme Court dismissed the case, arguing that Bhattacharya and his fellow plaintiffs lacked standing. Meaning: Yes, the government may have pressured private companies into silencing critics, but unless you can prove exactly how that harmed you, don’t expect the courts to care.
The real role of science
Despite everything, Bhattacharya didn’t argue for scientists to dictate policy. Unlike the public health bureaucrats who spent the pandemic issuing commandments from their Zoom thrones, he made it clear: “Science should be an engine for freedom,” he said. “Not something where it stands on top of society and says, ‘You must do this, this or this, or else.’”
That distinction matters. Science informs, but policy is about trade-offs. The problem wasn’t that officials got things wrong — it’s that they refused to admit the possibility. Instead of allowing open debate, they silenced critics. Instead of acknowledging uncertainty, they imposed rules with absolute certainty.
Bhattacharya wasn’t censored because he was wrong. He was censored because he questioned people who couldn’t afford to be.
His confirmation hearing made one thing clear: science wasn’t about data. It was about power. And in Washington, power doesn’t like to be questioned.
Science, money and power
At the heart of the hearing was a fundamental question: Who controls science that people are allowed to talk about? The NIH, with its $48 billion budget, is less a research institution and more a financial leviathan, shaping the direction of American science through the projects it funds (or doesn’t) fund.
Bhattacharya’s nomination comes at a moment when the battle lines around scientific freedom, government intervention, and public trust in research are more entrenched than ever. The pandemic shattered the illusion that science was above politics. Instead, it exposed just how much political and corporate interests shape what counts as “settled” science.
The irony is thick enough to cut with a knife. The man once branded too dangerous for social media, blacklisted for questioning lockdowns, and effectively erased from mainstream discourse is now being handed a key role in the very government that tried to silence him. Dr. Jay Bhattacharya, once forced to the margins, is now at the center of power.
A new administration has decided that maybe — just maybe — silencing dissenting scientists wasn’t the best pandemic strategy. And in a twist no Hollywood scriptwriter would dare to pitch for being too on-the-nose, Bhattacharya wasn’t being welcomed back into the conversation — he’s being put in charge of it.
Bhattacharya was confirmed following a party-line vote Tuesday evening. The decision came after a similarly partisan endorsement from the Senate Committee on Health, Education, Labor and Pensions (HELP), clearing the final hurdle for President Donald Trump’s nominee.
Equally central to his testimony was Bhattacharya’s call for a sweeping shift in NIH priorities. He proposed a decentralization of research funding, stressing the need for greater inclusion of dissenting voices in the scientific process, an apparent rebuke of the consensus-driven culture that dominated during the pandemic. He emphasized targeting resources toward projects with a clear and measurable impact on public health, dismissing other NIH initiatives as “frivolous.”
Now seated at the helm of the National Institutes of Health, Dr. Jay Bhattacharya is poised to reshape not only the agency’s research priorities but the very culture that pushed him to the fringe. His confirmation, hard-won and unapologetically political, is already shaking the scaffolding of a scientific establishment that long equated conformity with consensus.
Reprinted with permission from Reclaim The Net.
Addictions
Coffee, Nicotine, and the Politics of Acceptable Addiction

From the Brownstone Institute
By
Every morning, hundreds of millions of people perform a socially approved ritual. They line up for coffee. They joke about not being functional without caffeine. They openly acknowledge dependence and even celebrate it. No one calls this addiction degenerate. It is framed as productivity, taste, wellness—sometimes even virtue.
Now imagine the same professional discreetly using a nicotine pouch before a meeting. The reaction is very different. This is treated as a vice, something vaguely shameful, associated with weakness, poor judgment, or public health risk.
From a scientific perspective, this distinction makes little sense.
Caffeine and nicotine are both mild psychoactive stimulants. Both are plant-derived alkaloids. Both increase alertness and concentration. Both produce dependence. Neither is a carcinogen. Neither causes the diseases historically associated with smoking. Yet one has become the world’s most acceptable addiction, while the other remains morally polluted even in its safest, non-combustible forms.
This divergence has almost nothing to do with biology. It has everything to do with history, class, marketing, and a failure of modern public health to distinguish molecules from mechanisms.
Two Stimulants, One Misunderstanding
Nicotine acts on nicotinic acetylcholine receptors, mimicking a neurotransmitter the brain already uses to regulate attention and learning. At low doses, it improves focus and mood. At higher doses, it causes nausea and dizziness—self-limiting effects that discourage excess. Nicotine is not carcinogenic and does not cause lung disease.
Caffeine works differently, blocking adenosine receptors that signal fatigue. The result is wakefulness and alertness. Like nicotine, caffeine indirectly affects dopamine, which is why people rely on it daily. Like nicotine, it produces tolerance and withdrawal. Headaches, fatigue, and irritability are routine among regular users who skip their morning dose.
Pharmacologically, these substances are peers.
The major difference in health outcomes does not come from the molecules themselves but from how they have been delivered.
Combustion Was the Killer
Smoking kills because burning organic material produces thousands of toxic compounds—tar, carbon monoxide, polycyclic aromatic hydrocarbons, and other carcinogens. Nicotine is present in cigarette smoke, but it is not what causes cancer or emphysema. Combustion is.
When nicotine is delivered without combustion—through patches, gum, snus, pouches, or vaping—the toxic burden drops dramatically. This is one of the most robust findings in modern tobacco research.
And yet nicotine continues to be treated as if it were the source of smoking’s harm.
This confusion has shaped decades of policy.
How Nicotine Lost Its Reputation
For centuries, nicotine was not stigmatized. Indigenous cultures across the Americas used tobacco in religious, medicinal, and diplomatic rituals. In early modern Europe, physicians prescribed it. Pipes, cigars, and snuff were associated with contemplation and leisure.
The collapse came with industrialization.
The cigarette-rolling machine of the late 19th century transformed nicotine into a mass-market product optimized for rapid pulmonary delivery. Addiction intensified, exposure multiplied, and combustion damage accumulated invisibly for decades. When epidemiology finally linked smoking to lung cancer and heart disease in the mid-20th century, the backlash was inevitable.
But the blame was assigned crudely. Nicotine—the named psychoactive component—became the symbol of the harm, even though the damage came from smoke.
Once that association formed, it hardened into dogma.
How Caffeine Escaped
Caffeine followed a very different cultural path. Coffee and tea entered global life through institutions of respectability. Coffeehouses in the Ottoman Empire and Europe became centers of commerce and debate. Tea was woven into domestic ritual, empire, and gentility.
Crucially, caffeine was never bound to a lethal delivery system. No one inhaled burning coffee leaves. There was no delayed epidemic waiting to be discovered.
As industrial capitalism expanded, caffeine became a productivity tool. Coffee breaks were institutionalized. Tea fueled factory schedules and office routines. By the 20th century, caffeine was no longer seen as a drug at all but as a necessity of modern life.
Its downsides—dependence, sleep disruption, anxiety—were normalized or joked about. In recent decades, branding completed the transformation. Coffee became lifestyle. The stimulant disappeared behind aesthetics and identity.
The Class Divide in Addiction
The difference between caffeine and nicotine is not just historical. It is social.
Caffeine use is public, aesthetic, and professionally coded. Carrying a coffee cup signals busyness, productivity, and belonging in the middle class. Nicotine use—even in clean, low-risk forms—is discreet. It is not aestheticized. It is associated with coping rather than ambition.
Addictions favored by elites are rebranded as habits or wellness tools. Addictions associated with stress, manual labor, or marginal populations are framed as moral failings. This is why caffeine is indulgence and nicotine is degeneracy, even when the physiological effects are similar.
Where Public Health Went Wrong
Public health messaging relies on simplification. “Smoking kills” was effective and true. But over time, simplification hardened into distortion.
“Smoking kills” became “Nicotine is addictive,” which slid into “Nicotine is harmful,” and eventually into claims that there is “No safe level.” Dose, delivery, and comparative risk disappeared from the conversation.
Institutions now struggle to reverse course. Admitting that nicotine is not the primary harm agent would require acknowledging decades of misleading communication. It would require distinguishing adult use from youth use. It would require nuance.
Bureaucracies are bad at nuance.
So nicotine remains frozen at its worst historical moment: the age of the cigarette.
Why This Matters
This is not an academic debate. Millions of smokers could dramatically reduce their health risks by switching to non-combustion nicotine products. Countries that have allowed this—most notably Sweden—have seen smoking rates and tobacco-related mortality collapse. Countries that stigmatize or ban these alternatives preserve cigarette dominance.
At the same time, caffeine consumption continues to rise, including among adolescents, with little moral panic. Energy drinks are aggressively marketed. Sleep disruption and anxiety are treated as lifestyle issues, not public health emergencies.
The asymmetry is revealing.
Coffee as the Model Addiction
Caffeine succeeded culturally because it aligned with power. It supported work, not resistance. It fit office life. It could be branded as refinement. It never challenged institutional authority.
Nicotine, especially when used by working-class populations, became associated with stress relief, nonconformity, and failure to comply. That symbolism persisted long after the smoke could be removed.
Addictions are not judged by chemistry. They are judged by who uses them and whether they fit prevailing moral narratives.
Coffee passed the test. Nicotine did not.
The Core Error
The central mistake is confusing a molecule with a method. Nicotine did not cause the smoking epidemic. Combustion did. Once that distinction is restored, much of modern tobacco policy looks incoherent. Low-risk behaviors are treated as moral threats, while higher-risk behaviors are tolerated because they are culturally embedded.
This is not science. It is politics dressed up as health.
A Final Thought
If we applied the standards used against nicotine to caffeine, coffee would be regulated like a controlled substance. If we applied the standards used for caffeine to nicotine, pouches and vaping would be treated as unremarkable adult choices.
The rational approach is obvious: evaluate substances based on dose, delivery, and actual harm. Stop moralizing chemistry. Stop pretending that all addictions are equal. Nicotine is not harmless. Neither is caffeine. But both are far safer than the stories told about them.
This essay only scratches the surface. The strange moral history of nicotine, caffeine, and acceptable addiction exposes a much larger problem: modern institutions have forgotten how to reason about risk.
Health
All 12 Vaccinated vs. Unvaccinated Studies Found the Same Thing: Unvaccinated Children Are Far Healthier

I joined Del Bigtree in studio on The HighWire to discuss what the data now make unavoidable: the CDC’s 81-dose hyper-vaccination schedule is driving the modern epidemics of chronic disease and autism.
This was not a philosophical debate or a clash of opinions. We walked through irrefutable, peer-reviewed evidence showing that whenever vaccinated and unvaccinated children are compared directly, the unvaccinated group is far healthier—every single time.
Reanalyzing the Largest Vaccinated vs. Unvaccinated Birth-Cohort Study Ever Conducted
At the center of our discussion was our peer-reviewed reanalysis of the Henry Ford Health System vaccinated vs. unvaccinated birth-cohort study (Lamerato et al.)—the largest and most rigorous comparison of its kind ever conducted.
|
The original authors relied heavily on Cox proportional hazards models, a time-adjusted approach that can soften absolute disease burden. Even so, nearly all chronic disease outcomes were higher in vaccinated children.
Our reanalysis used direct proportional comparisons, stripping away the smoothing and revealing the full magnitude of the signal.
- All 22 chronic disease categories favored the unvaccinated cohort when proportional disease burden was examined
- Cancer incidence was 54% higher in vaccinated children (0.0102 vs. 0.0066)
- When autism-associated conditions were grouped appropriately—including autism, ADHD, developmental delay, learning disability, speech disorder, neurologic impairment, seizures, and related diagnoses—the vaccinated cohort showed a 549% higher odds of autism-spectrum–associated clinical outcomes
The findings are internally consistent, biologically coherent, and concordant with every prior vaccinated vs. unvaccinated study, all of which show drastically poorer health outcomes among vaccinated children
The 12 Vaccinated vs. Unvaccinated Studies Regulators Ignore
In the McCullough Foundation Autism Report, we compiled all 12 vaccinated vs. unvaccinated pediatric studies currently available. These studies span different populations, countries, study designs, and data sources.
Every single one reports the same overall pattern. Across all 12 studies, unvaccinated children consistently exhibit substantially lower rates of chronic disease, including:
- Autism and other neurodevelopmental disorders
- ADHD, tics, learning and speech disorders
- Asthma, allergies, eczema, and autoimmune conditions
- Chronic ear infections, skin disorders, and gastrointestinal illness
This level of consistency across independent datasets is precisely what epidemiology looks for when assessing causality. It also explains why no federal agency has ever conducted—or endorsed—a fully vaccinated vs. fully unvaccinated safety study.
Flu Shot Failure
We also addressed the persistent failure of seasonal influenza vaccination.
A large Cleveland Clinic cohort study of 53,402 employees followed participants during the 2024–2025 respiratory viral season and found:
- 82.1% of employees were vaccinated against influenza
- Vaccinated individuals had a 27% higher adjusted risk of influenza compared with the unvaccinated state (HR 1.27; 95% CI 1.07–1.51; p = 0.007)
- This corresponded to a negative vaccine effectiveness of −26.9% (95% CI −55.0 to −6.6%), meaning vaccination was associated with increased—not reduced—risk of influenza
When vaccination exposure increases, chronic disease, neurodevelopmental disorders, and inflammatory illness increase with it. When children are unvaccinated, they are measurably healthier across virtually every outcome that matters.
The science needed to confront the chronic disease and autism epidemics already exists. What remains is the willingness to acknowledge it.
Epidemiologist and Foundation Administrator, McCullough Foundation
Support our mission: mcculloughfnd.org
Please consider following both the McCullough Foundation and my personal account on X (formerly Twitter) for further content.
FOCAL POINTS (Courageous Discourse) is a reader-supported publication.
To receive new posts and support my work, consider becoming a free or paid subscriber.
-

 Energy2 days ago
Energy2 days agoThe U.S. Just Removed a Dictator and Canada is Collateral Damage
-
 International2 days ago
International2 days agoUS Justice Department Accusing Maduro’s Inner Circle of a Narco-State Conspiracy
-

 Haultain Research2 days ago
Haultain Research2 days agoTrying to Defend Maduro’s Legitimacy
-
 International2 days ago
International2 days agoU.S. Claims Western Hemispheric Domination, Denies Russia Security Interests On Its Own Border
-
 Daily Caller1 day ago
Daily Caller1 day agoTrump Says US Going To Run Venezuela After Nabbing Maduro
-

 Opinion1 day ago
Opinion1 day agoHell freezes over, CTV’s fabrication of fake news and our 2026 forecast is still searching for sunshine
-

 International2 days ago
International2 days ago“It’s Not Freedom — It’s the First Step Toward Freedom”
-

 Daily Caller1 day ago
Daily Caller1 day agoScathing Indictment Claims Nicolás Maduro Orchestrated Drug-Fueled ‘Culture Of Corruption’ Which Plagued Entire Region









