Health
Quadriplegic man dies via euthanasia after developing bed sores waiting at Quebec hospital

66-year-old Quebec man Normand Meunier who died via euthanasia after a 4-day hospital stay left him with severe bed sores
From LifeSiteNews
‘I don’t want to be a burden,’ the 66-year-old man said prior to his death after he developed bed sores due to a lack of specialized care at a hospital in Saint-Jérôme, Quebec.
A quadriplegic man in Quebec was killed via euthanasia after he developed severe bed sores while waiting in a hospital for an extended period of time.
On March 29, Normand Meunier, a 66-year-old quadriplegic man in Quebec, was euthanized in his home after developing bed sores due to a lack of specialized care at the hospital in Saint-Jérôme, Quebec, according to a report by Radio-Canada.
“I don’t want to be a burden. At any rate, the medical opinions say I won’t be a burden for long; as the old folks say, it’s better to kick the can,” Meunier told Radio-Canada in an interview the day before he was killed.
Meunier, whose arms and legs have been paralyzed since 2022 due to a spinal cord injury, went to the hospital’s intensive care for a respiratory virus. According to his partner Sylvie Brosseau, the hospital placed Meunier on a stretcher for 95 hours.
Bosseau revealed that she asked medical staff to provide a specialized bed for Meunier but was told that the hospital would have to order one. According to the hospital, they are investigating the incident, adding that they do have beds available.
After spending four days on a hospital cot, Meunier developed bed sores and a major pressure ulcer on his buttocks, which were so severe that the muscle and bone were exposed and visible.
While Meunier had previously experienced bedsores, he determined to end his life via Medical Assistance in Dying (MAiD), the euphemistic name for Canada’s euthanasia regime, rather than continue to receive treatment.
Unfortunately, Meunier is not the first Canadians to choose MAiD after being given insufficient medical care.
As a result of a healthcare worker shortage, wait times to receive care in Canada have increased to an average of 27.7 weeks, leading some Canadians to despair and opt for euthanasia instead of waiting for assistance.
This was the case of 52-year-old Dan Quayle, a grandfather from British Columbia. On November 24, he chose to be killed via lethal injection after being unable to receive cancer treatment due to the increased wait times.
Throughout the agonizing wait, his family “prayed he would change his mind or get an 11th-hour call that chemo had been scheduled,” but were instead told consistently by the hospital that they were “backlogged.”
Similarly, in 2022, a Winnipeg woman wrote in her posthumously published obituary that she chose to die by assisted suicide after being refused the treatments she needed: “I could have had more time if I had more help.”
However, instead of supporting the healthcare system to prevent Canadians from taking their own lives, the Trudeau government is working to expand access to MAiD by loosening its requirements.
On March 9, 2024, MAiD was set to expand to include those suffering solely from mental illness. This is a result of the 2021 passage of Bill C-7, which also allowed the chronically ill – not just the terminally ill – to qualify for so-called doctor-assisted death.
After massive pushback from doctors, pro-life groups and politicians, the program’s expansion was temporarily paused until 2027.
According to Health Canada, in 2022, 13,241 Canadians died by MAiD lethal injection, which is 4.1 percent of all deaths in the country for that year, and a 31.2 percent increase from 2021.
The number of Canadians killed by lethal injection since 2016 now stands at 44,958.
Health
New report warns WHO health rules erode Canada’s democracy and Charter rights
The Justice Centre for Constitutional Freedoms has released a new report titled Canada’s Surrender of Sovereignty: New WHO health regulations undermine Canadian democracy and Charter freedoms. Authored by Nigel Hannaford, a veteran journalist and researcher, the report warns that Canada’s acceptance of the World Health Organization’s (WHO) revised International Health Regulations (IHR) represents a serious erosion of national independence and democratic accountability.
The IHR amendments, which took effect on September 19, 2025, authorize the WHO Director-General to declare global “health emergencies” that could require Canada to follow directives from bureaucrats in Geneva, bypassing the House of Commons and the will of Canadian voters.
The WHO regards these regulations as “binding,” despite having no ability or legal authority to impose such regulations. Even so, Canada is opting to accept the regulations as binding.
By accepting the WHO’s revised IHR, the report explains, Canada has relinquished its own control over future health crises and instead has agreed to let the WHO determine when a “pandemic emergency” exists and what Canada must do to respond to it, after which Canada must report back to the WHO.
In fact, under these International Health Regulations, the WHO could demand countries like Canada impose stringent freedom-violating health policies, such as lockdowns, vaccine mandates, or travel restrictions without debate, evidence review, or public accountability, the report explains.
Once the WHO declares a “Pandemic Emergency,” member states are obligated to implement such emergency measures “without delay” for a minimum of three months.
Importantly, following these WHO directives would undermine government accountability as politicians may hide behind international “commitments” to justify their actions as “simply following international rules,” the report warns.
Canada should instead withdraw from the revised IHR, following the example of countries like Germany, Austria, Italy, Czech Republic, and the United States. The report recommends continued international cooperation without surrendering control over domestic health policies.
Constitutional lawyer Allison Pejovic said, “[b]y treating WHO edicts as binding, the federal government has effectively placed Canadian sovereignty on loan to an unelected international body.”
“Such directives, if enforced, would likely violate Canadians’ Charter rights and freedoms,” she added.
Mr. Hannaford agreed, saying, “Canada’s health policies must be made in Canada. No free and democratic nation should outsource its emergency powers to unelected bureaucrats in Geneva.”
The Justice Centre urges Canadians to contact their Members of Parliament and demand they support withdrawing from the revised IHR to restore Canadian sovereignty and reject blind compliance with WHO directives.
Business
Cutting Red Tape Could Help Solve Canada’s Doctor Crisis

From the Frontier Centre for Public Policy
By Ian Madsen
Doctors waste millions of hours on useless admin. It’s enough to end Canada’s doctor shortage. Ian Madsen says slashing red tape, not just recruiting, is the fastest fix for the clogged system.
Doctors spend more time on paperwork than on patients and that’s fueling Canada’s health care wait lists
Canada doesn’t just lack doctors—it squanders the ones it has. Mountains of paperwork and pointless admin chew up tens of millions of physician hours every year, time that could erase the so-called shortage and slash wait lists if freed for patient care.
Recruiting more doctors helps, but the fastest cure for our sick system is cutting the bureaucracy that strangles the ones already here.
The Canadian Medical Association found that unnecessary non-patient work consumes millions of hours annually. That’s the equivalent of 50.5 million patient visits, enough to give every Canadian at least one appointment and likely erase the physician shortage. Meanwhile, the Canadian Institute for Health Information estimates more than six million Canadians don’t even have a family doctor. That’s roughly one in six of us.
And it’s not just patients who feel the shortage—doctors themselves are paying the price. Endless forms don’t just waste time; they drive doctors out of the profession. Burned out and frustrated, many cut their hours or leave entirely. And the foreign doctors that health authorities are trying to recruit? They might think twice once they discover how much time Canadian physicians spend on paperwork that adds nothing to patient care.
But freeing doctors from forms isn’t as simple as shredding them. Someone has to build systems that reduce, rather than add to, the workload. And that’s where things get tricky. Trimming red tape usually means more Information Technology (IT), and big software projects have a well-earned reputation for spiralling in cost.
Bent Flyvbjerg, the global guru of project disasters, and his colleagues examined more than 5,000 IT projects in a 2022 study. They found outcomes didn’t follow a neat bell curve but a “power-law” distribution, meaning costs don’t just rise steadily, they explode in a fat tail of nasty surprises as variables multiply.
Oxford University and McKinsey offered equally bleak news. Their joint study concluded: “On average, large IT projects run 45 per cent over budget and seven per cent over time while delivering 56 per cent less value than predicted.” If that sounds familiar, it should. Canada’s Phoenix federal payroll fiasco—the payroll software introduced by Ottawa that left tens of thousands of federal workers underpaid or unpaid—is a cautionary tale etched into the national memory.
The lesson isn’t to avoid technology, but to get it right. Canada can’t sidestep the digital route. The question is whether we adapt what others have built or design our own. One option is borrowing from the U.S. or U.K., where electronic health record (EHR) systems (the digital patient files used by doctors and hospitals) are already in place. Both countries have had headaches with their systems, thanks to legal and regulatory differences. But there are signs of progress.
The U.K. is experimenting with artificial intelligence to lighten the administrative load, and a joint U.K.-U.S. study gives a glimpse of what’s possible:
“… AI technologies such as Robotic Process Automation (RPA), predictive analytics, and Natural Language Processing (NLP) are transforming health care administration. RPA and AI-driven software applications are revolutionizing health care administration by automating routine tasks such as appointment scheduling, billing, and documentation. By handling repetitive, rule-based tasks with speed and accuracy, these technologies minimize errors, reduce administrative burden, and enhance overall operational efficiency.”
For patients, that could mean fewer missed referrals, faster follow-up calls and less time waiting for paperwork to clear before treatment. Still, even the best tools come with limits. Systems differ, and customization will drive up costs. But medicine is medicine, and AI tools can bridge more gaps than you might think.
Run the math. If each “freed” patient visit is worth just $20—a conservative figure for the value of a basic appointment—the payoff could hit $1 billion in a single year.
Updating costs would continue, but that’s still cheap compared to the human and financial toll of endless wait lists. Cost-sharing between provinces, Ottawa, municipalities and even doctors themselves could spread the risk. Competitive bidding, with honest budgets and realistic timelines, is non-negotiable if we want to dodge another Phoenix-sized fiasco.
The alternative—clinging to our current dysfunctional patchwork of physician information systems—isn’t really an option. It means more frustrated doctors walking away, fewer new ones coming in, and Canadians left to languish on wait lists that grow ever longer.
And that’s not health care—it’s managed decline.
Ian Madsen is a senior policy analyst at the Frontier Centre for Public Policy.
-
 Alberta1 day ago
Alberta1 day agoClick here to help choose Alberta’s new licence plate design
-

 National1 day ago
National1 day agoDemocracy Watch Renews Push for Independent Prosecutor in SNC-Lavalin Case
-

 Business1 day ago
Business1 day agoOver two thirds of Canadians say Ottawa should reduce size of federal bureaucracy
-

 Business2 days ago
Business2 days agoTrump Admin Blows Up UN ‘Global Green New Scam’ Tax Push, Forcing Pullback
-

 Business2 days ago
Business2 days agoTrump Blocks UN’s Back Door Carbon Tax
-
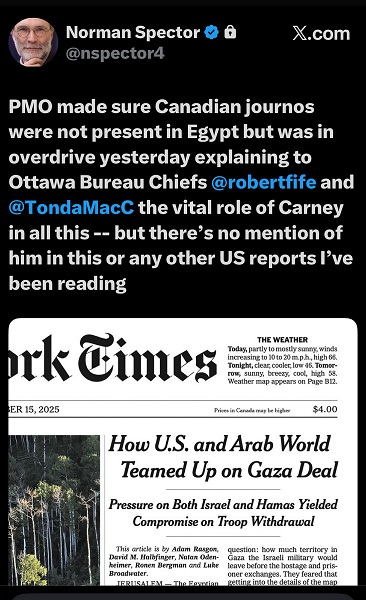
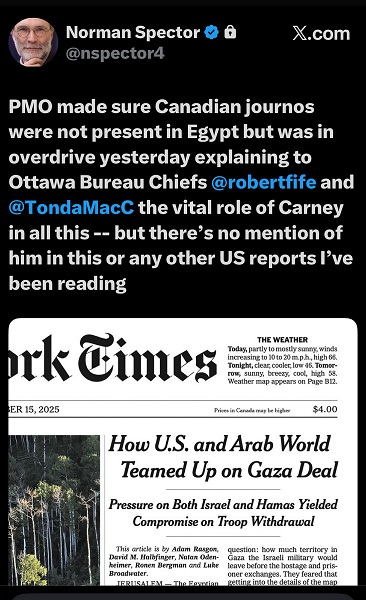 Media1 day ago
Media1 day agoCanada’s top Parliamentary reporters easily manipulated by the PMO’s “anonymous sources”
-

 Agriculture1 day ago
Agriculture1 day agoIs the CFIA a Rogue Agency or Just Taking Orders from a Rogue Federal Government?
-

 Red Deer2 days ago
Red Deer2 days agoYour last minute election prep: Common Sense Red Deer talks to the candidates




