Fraser Institute
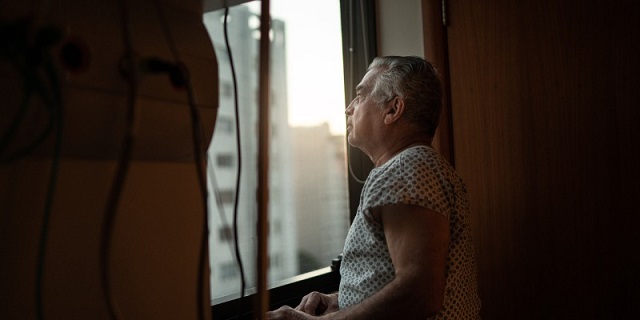
Ottawa’s health-care deal cements failed status quo in Canada
From the Fraser Institute
By Mackenzie Moir and Jake Fuss
Canada will reach a projected $244.1 billion in 2023, which translates to $6,205 per person—nearly double the level of per-person spending (inflation-adjusted) three decades ago. And yet, last year Canadians endured the longest median wait time (27.7 weeks) ever recorded for non-emergency surgery.
Last week, as part of Ottawa’s promised $46 billion in additional health-care spending, the Trudeau government agreed to increase Quebec’s share of federal health-care dollars by $900 million annually. Quebec was the last province to reach an agreement with Ottawa before the March 31 deadline. With the closure of this agreement, Canadian taxpayers are on the hook for more health-care spending than ever before. For the same old broken health-care system.
Of course, it ultimately doesn’t matter whether the $46 billion originates from Ottawa or the provinces. In the end, Canadian taxpayers foot the bill. And what do we get in return for our health-care dollars?
In 2021, the latest year of comparable data, Canada’s total health-care spending (as a percentage of the economy) was the highest among 29 other comparable countries with universal health care (after adjusting for differences in population age). This isn’t a new development. Canada has a long history of having one of most expensive systems among high-income universal health-care countries.
Despite this, according to the latest comparable data, Canada ranks among the poorest performing universal health-care countries in key areas such as the number of physicians, hospital beds and diagnostic technology (e.g. MRI machines). Further, according to the Commonwealth Fund, in 2020 Canada ranked dead last on timely access to specialist consultations and non-emergency surgery.
Meanwhile, public health-care spending in Canada will reach a projected $244.1 billion in 2023, which translates to $6,205 per person—nearly double the level of per-person spending (inflation-adjusted) three decades ago. And yet, last year Canadians endured the longest median wait time (27.7 weeks) ever recorded for non-emergency surgery.
In short, Canada’s health-care system is in shambles, but the answer does not lie in simply throwing more money in its general direction. Federal politicians should instead look to the example of welfare reform during the Chrétien era in the 1990s. Those reforms, which reduced federal transfers to provinces and eliminated most of the “strings” attached to federal funding, resulted in increased provincial autonomy, greater policy experimentation, fewer Canadians needing welfare and savings for the federal government (i.e. taxpayers).
This is the opposite of today’s approach to health care, where the existing vehicle for federal funding (the Canada Health Transfer) is connected to the Canada Health Act (CHA), which prevents provincial governments from innovating and experimenting in health care by threatening financial penalties for non-compliance with often vaguely defined federal preferences. The result is a stalemate that satisfies no one and ensures that Canada’s policies remain at odds with the policies of our better-performing universal health-care peers.
While new federal dollars for health care are undoubtedly appealing to premiers, they will not improve the state of health care for Canadians. Until our federal politicians have the courage to reform the CHA and follow the example of 1990s welfare reform to improve outcomes, our health-care system’s unacceptable status quo will continue.
Authors:
Business
Residents in economically free states reap the rewards

From the Fraser Institute
A report published by the Fraser Institute reaffirms just how much more economically free some states are compared with others. These are places where citizens are allowed to make more of their economic choices. Their taxes are lighter, and their regulatory burdens are easier. The benefits for workers, consumers and businesses have been clear for a long time.
There’s another group of states to watch: “movers” that have become much freer in recent decades. These are states that may not be the freest, but they have been cutting taxes and red tape enough to make a big difference.
How do they fare?
I recently explored this question using 22 years of data from the same Economic Freedom of North America index. The index uses 10 variables encompassing government spending, taxation and labour regulation to assess the degree of economic freedom in each of the 50 states.
Some states, such as New Hampshire, have long topped the list. It’s been in the top five for three decades. With little room to grow, the Granite State’s level of economic freedom hasn’t budged much lately. Others, such as Alaska, have significantly improved economic freedom over the last two decades. Because it started so low, it remains relatively unfree at 43rd out of 50.
Three states—North Carolina, North Dakota and Idaho—have managed to markedly increase and rank highly on economic freedom.
In 2000, North Carolina was the 19th most economically free state in the union. Though its labour market was relatively unhindered by the state’s government, its top marginal income tax rate was America’s ninth-highest, and it spent more money than most states.
From 2013 to 2022, North Carolina reduced its top marginal income tax rate from 7.75 per cent to 4.99 per cent, reduced government employment and allowed the minimum wage to fall relative to per-capita income. By 2022, it had the second-freest labour market in the country and was ninth in overall economic freedom.
North Dakota took a similar path, reducing its 5.54 per cent top income tax rate to 2.9 per cent, scaling back government employment, and lowering its minimum wage to better reflect local incomes. It went from the 27th most economically free state in the union in 2000 to the 10th freest by 2022.
Idaho saw the most significant improvement. The Gem State has steadily improved spending, taxing and labour market freedom, allowing it to rise from the 28th most economically free state in 2000 to the eighth freest in 2022.
We can contrast these three states with a group that has achieved equal and opposite distinction: California, Delaware, New Jersey and Maryland have managed to decrease economic freedom and end up among the least free overall.
What was the result?
The economies of the three liberating states have enjoyed almost twice as much economic growth. Controlling for inflation, North Carolina, North Dakota and Idaho grew an average of 41 per cent since 2010. The four repressors grew by just 24 per cent.
Among liberators, statewide personal income grew 47 per cent from 2010 to 2022. Among repressors, it grew just 26 per cent.
In fact, when it comes to income growth per person, increases in economic freedom seem to matter even more than a state’s overall, long-term level of freedom. Meanwhile, when it comes to population growth, placing highly over longer periods of time matters more.
The liberators are not unique. There’s now a large body of international evidence documenting the freedom-prosperity connection. At the state level, high and growing levels of economic freedom go hand-in-hand with higher levels of income, entrepreneurship, in-migration and income mobility. In economically free states, incomes tend to grow faster at the top and bottom of the income ladder.
These states suffer less poverty, homelessness and food insecurity and may even have marginally happier, more philanthropic and more tolerant populations.
In short, liberation works. Repression doesn’t.
Alberta
Alberta Next Panel calls for less Ottawa—and it could pay off

From the Fraser Institute
By Tegan Hill
Last Friday, less than a week before Christmas, the Smith government quietly released the final report from its Alberta Next Panel, which assessed Alberta’s role in Canada. Among other things, the panel recommends that the federal government transfer some of its tax revenue to provincial governments so they can assume more control over the delivery of provincial services. Based on Canada’s experience in the 1990s, this plan could deliver real benefits for Albertans and all Canadians.
Federations such as Canada typically work best when governments stick to their constitutional lanes. Indeed, one of the benefits of being a federalist country is that different levels of government assume responsibility for programs they’re best suited to deliver. For example, it’s logical that the federal government handle national defence, while provincial governments are typically best positioned to understand and address the unique health-care and education needs of their citizens.
But there’s currently a mismatch between the share of taxes the provinces collect and the cost of delivering provincial responsibilities (e.g. health care, education, childcare, and social services). As such, Ottawa uses transfers—including the Canada Health Transfer (CHT)—to financially support the provinces in their areas of responsibility. But these funds come with conditions.
Consider health care. To receive CHT payments from Ottawa, provinces must abide by the Canada Health Act, which effectively prevents the provinces from experimenting with new ways of delivering and financing health care—including policies that are successful in other universal health-care countries. Given Canada’s health-care system is one of the developed world’s most expensive universal systems, yet Canadians face some of the longest wait times for physicians and worst access to medical technology (e.g. MRIs) and hospital beds, these restrictions limit badly needed innovation and hurt patients.
To give the provinces more flexibility, the Alberta Next Panel suggests the federal government shift tax points (and transfer GST) to the provinces to better align provincial revenues with provincial responsibilities while eliminating “strings” attached to such federal transfers. In other words, Ottawa would transfer a portion of its tax revenues from the federal income tax and federal sales tax to the provincial government so they have funds to experiment with what works best for their citizens, without conditions on how that money can be used.
According to the Alberta Next Panel poll, at least in Alberta, a majority of citizens support this type of provincial autonomy in delivering provincial programs—and again, it’s paid off before.
In the 1990s, amid a fiscal crisis (greater in scale, but not dissimilar to the one Ottawa faces today), the federal government reduced welfare and social assistance transfers to the provinces while simultaneously removing most of the “strings” attached to these dollars. These reforms allowed the provinces to introduce work incentives, for example, which would have previously triggered a reduction in federal transfers. The change to federal transfers sparked a wave of reforms as the provinces experimented with new ways to improve their welfare programs, and ultimately led to significant innovation that reduced welfare dependency from a high of 3.1 million in 1994 to a low of 1.6 million in 2008, while also reducing government spending on social assistance.
The Smith government’s Alberta Next Panel wants the federal government to transfer some of its tax revenues to the provinces and reduce restrictions on provincial program delivery. As Canada’s experience in the 1990s shows, this could spur real innovation that ultimately improves services for Albertans and all Canadians.
-

 International2 days ago
International2 days agoOttawa is still dodging the China interference threat
-

 Business2 days ago
Business2 days agoThere’s No Bias at CBC News, You Say? Well, OK…
-

 Automotive2 days ago
Automotive2 days agoCanada’s EV gamble is starting to backfire
-

 International2 days ago
International2 days ago2025: The Year The Narrative Changed
-

 Energy2 days ago
Energy2 days agoNew Poll Shows Ontarians See Oil & Gas as Key to Jobs, Economy, and Trade
-
 Energy2 days ago
Energy2 days agoCanada’s debate on energy levelled up in 2025
-

 Business2 days ago
Business2 days agoSocialism vs. Capitalism
-

 Daily Caller2 days ago
Daily Caller2 days agoIs Ukraine Peace Deal Doomed Before Zelenskyy And Trump Even Meet At Mar-A-Lago?









