Alberta
Province commits $4 million for overdose response teams and 35 detox and pre-treatment beds in Calgary

Expanding access to detox and recovery in Calgary
Alberta’s government is investing in detox, recovery and dynamic overdose response services at the Drop-In Centre in Calgary.
Every Albertan struggling with addiction deserves the opportunity to pursue recovery. As part of building a recovery-oriented system of care, Alberta’s government is providing more than $4 million to the Calgary Drop-In Centre to create dynamic overdose response teams and establish 35 medical detox and pre-treatment beds, capable of supporting up to 1,000 Calgarians every year.
This partnership stems from the efforts led by the Calgary Public Safety and Community Response Task Force to improve public safety while treating addiction and mental health as healthcare issues.
“We’re continuing to treat mental health and addiction as health-care issues by building recovery-oriented systems of care to ensure every Albertan has the opportunity to pursue recovery. Whether it’s rapidly responding to an overdose, accessing medical detox or pre-treatment, the impact of this funding will be life-saving and life-changing for so many Albertans.”
“Our government’s focus on addiction recovery and supports for those facing homelessness is bringing positive change for Calgary. The Calgary Drop-In Centre does incredible work to provide services for many individuals facing homelessness. With more access to addiction recovery treatment, more Albertans will be able to get the help they need to overcome their challenges.”
With this funding, the Calgary Drop-In Centre will significantly increase its treatment capacity. This includes:
- 15 medical detox beds and 20 pre-treatment beds: Albertans struggling with addiction will be supported to safely withdraw from drugs or alcohol under medical supervision. They will also be provided with pre-treatment support to prevent relapse and better understand treatment options as they continue their pursuit of recovery.
- Dynamic overdose response teams: To keep communities safe while treating addiction as a health-care issue, the Calgary Drop-In Centre will work in conjunction with local paramedics, first responders and community organizations to respond to overdoses both at the Drop-In Centre as well as in the community.
“People struggling with mental health and addiction deserve compassion and support, and at the Drop-In Centre they receive both. We’re pleased to work with Alberta’s government to deliver critical services to those in need and help more vulnerable people in our communities pursue recovery from addiction.”
These additional medical detox and pre-treatment beds, capable of supporting up to 1,000 Calgarians every year, will be life-saving and life-changing for countless people in the years to come. All publicly funded detox, treatment and recovery spaces are free for Albertans, with no user fees.
Alberta’s government is continuing to build a recovery-oriented system of care, where everyone struggling with addiction and mental health challenges is supported in their pursuit of recovery. This includes initiatives like eliminating fees for residential addiction treatment, launching the Digital Overdose Response System (DORS) app and expanding access to opioid agonist treatment.
In December 2022, Alberta’s government established two new cabinet task forces to bring community partners together to address the issues of addiction, homelessness and public safety in Calgary and Edmonton. The two Public Safety and Community Response Task Forces are responsible for implementing $187 million in provincial funding to further build out a recovery-oriented system of addiction and mental health care. The initiatives being implemented are part of a fair, firm and compassionate approach to keeping communities safe while treating addiction and mental health as health-care issues.
Quick facts
- Alberta’s government is providing $3.8 million per year, with $1.6 million for dynamic overdose response services and nearly $2.2 million to offer 15 detox and 20 pre-treatment beds, capable of supporting up to 1,000 Calgarians annually. There was also a one-time investment of about $450,000 for capital improvements.
- Clients with opioid addiction will also be able to immediately start on evidence-based opioid treatment medications like suboxone and sublocade through Alberta’s Virtual Opioid Dependency Program.
- Alberta spends more than $1 billion annually on addiction and mental health care and supports, including prevention, intervention, treatment and recovery.
- Any Albertan struggling with addiction can contact 211 Alberta to connect with local services and virtual supports. 211 is free, confidential and available 24-7.
- The Virtual Opioid Dependency Program provides same-day access to addiction medicine physicians and life-saving medications to Albertans across the province. Albertans can call 1-844-383-7688 seven days a week, from 8 a.m. to 8 p.m. daily.
Agriculture
Lacombe meat processor scores $1.2 million dollar provincial tax credit to help expansion

Alberta’s government continues to attract investment and grow the provincial economy.
The province’s inviting and tax-friendly business environment, and abundant agricultural resources, make it one of North America’s best places to do business. In addition, the Agri-Processing Investment Tax Credit helps attract investment that will further diversify Alberta’s agriculture industry.
Beretta Farms is the most recent company to qualify for the tax credit by expanding its existing facility with the potential to significantly increase production capacity. It invested more than $10.9 million in the project that is expected to increase the plant’s processing capacity from 29,583 to 44,688 head of cattle per year. Eleven new employees were hired after the expansion and the company plans to hire ten more. Through the Agri-Processing Investment Tax Credit, Alberta’s government has issued Beretta Farms a tax credit of $1,228,735.
“The Agri-Processing Investment Tax Credit is building on Alberta’s existing competitive advantages for agri-food companies and the primary producers that supply them. This facility expansion will allow Beretta Farms to increase production capacity, which means more Alberta beef across the country, and around the world.”
“This expansion by Beretta Farms is great news for Lacombe and central Alberta. It not only supports local job creation and economic growth but also strengthens Alberta’s global reputation for producing high-quality meat products. I’m proud to see our government supporting agricultural innovation and investment right here in our community.”
The tax credit provides a 12 per cent non-refundable, non-transferable tax credit when businesses invest $10 million or more in a project to build or expand a value-added agri-processing facility in Alberta. The program is open to any food manufacturers and bio processors that add value to commodities like grains or meat or turn agricultural byproducts into new consumer or industrial goods.
Beretta Farms’ facility in Lacombe is a federally registered, European Union-approved harvesting and meat processing facility specializing in the slaughter, processing, packaging and distribution of Canadian and United States cattle and bison meat products to 87 countries worldwide.
“Our recent plant expansion project at our facility in Lacombe has allowed us to increase our processing capacities and add more job opportunities in the central Alberta area. With the support and recognition from the Government of Alberta’s tax credit program, we feel we are in a better position to continue our success and have the confidence to grow our meat brands into the future.”
Alberta’s agri-processing sector is the second-largest manufacturing industry in the province and meat processing plays an important role in the sector, generating millions in annual economic impact and creating thousands of jobs. Alberta continues to be an attractive place for agricultural investment due to its agricultural resources, one of the lowest tax rates in North America, a business-friendly environment and a robust transportation network to connect with international markets.
Quick facts
- Since 2023, there are 16 applicants to the Agri-Processing Investment Tax Credit for projects worth about $1.6 billion total in new investment in Alberta’s agri-processing sector.
- To date, 13 projects have received conditional approval under the program.
- Each applicant must submit progress reports, then apply for a tax credit certificate when the project is complete.
- Beretta Farms has expanded the Lacombe facility by 10,000 square feet to include new warehousing, cooler space and an office building.
- This project has the potential to increase production capacity by 50 per cent, thereby facilitating entry into more European markets.
Related information
Alberta
Alberta Independence Seekers Take First Step: Citizen Initiative Application Approved, Notice of Initiative Petition Issued

Alberta’s Chief Electoral Officer, Gordon McClure, has issued a Notice of Initiative Petition.
This confirms a Citizen Initiative application has been received and the Chief Electoral Officer has determined the requirements of section 2(3) of the Citizen Initiative Act have been met.
Approved Initiative Petition Information
The approved citizen initiative application is for a policy proposal with the following proposed question:
Do you agree that Alberta should remain in Canada?
The Notice of Initiative Petition, application, and statement provided by the proponent are available on Elections Alberta’s website on the Current Initiatives Petition page.
As the application was received and approved prior to coming into force of Bill 54: Election Statutes Amendment Act, the Citizen Initiative process will follow requirements set out in the Citizen Initiative Act as of June 30, 2025.
Next Steps
- The proponent must appoint a chief financial officer within 30 days (by July 30, 2025).
- Once the 30-day publication period is complete and a chief financial officer has been appointed, Elections Alberta will:
- issue the citizen initiative petition,
- publish a notice on the Current Initiatives Petition page of our website indicating the petition has been issued, specifying the signing period dates, and the number of signatures required for a successful petition, and
- issue the citizen initiative petition signature sheets and witness affidavits. Signatures collected on other forms will not be accepted.
More information on the process, the status of the citizen initiative petition, financing rules, third party advertising rules, and frequently asked questions may be found on the Elections Alberta website.
Elections Alberta is an independent, non-partisan office of the Legislative Assembly of Alberta responsible for administering provincial elections, by-elections, and referendums.
-

 Alberta14 hours ago
Alberta14 hours agoAlberta Independence Seekers Take First Step: Citizen Initiative Application Approved, Notice of Initiative Petition Issued
-
 Crime13 hours ago
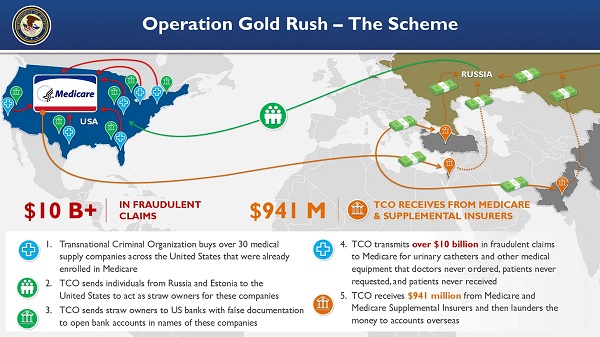
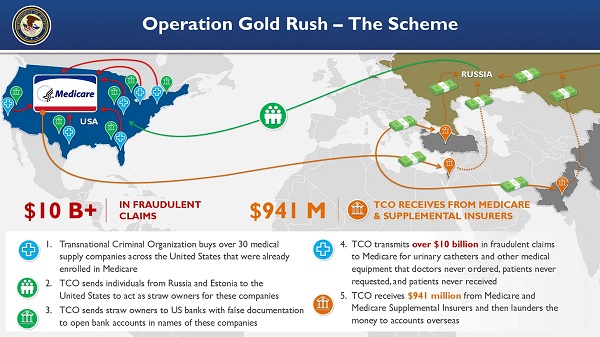
Crime13 hours agoNational Health Care Fraud Takedown Results in 324 Defendants Charged in Connection with Over $14.6 Billion in Alleged Fraud
-

 Health12 hours ago
Health12 hours agoRFK Jr. Unloads Disturbing Vaccine Secrets on Tucker—And Surprises Everyone on Trump
-

 Bruce Dowbiggin15 hours ago
Bruce Dowbiggin15 hours agoThe Game That Let Canadians Forgive The Liberals — Again
-

 Alberta1 day ago
Alberta1 day agoCOVID mandates protester in Canada released on bail after over 2 years in jail
-

 Business1 day ago
Business1 day agoCanada’s loyalty to globalism is bleeding our economy dry
-

 Crime2 days ago
Crime2 days agoProject Sleeping Giant: Inside the Chinese Mercantile Machine Linking Beijing’s Underground Banks and the Sinaloa Cartel
-

 Alberta2 days ago
Alberta2 days agoAlberta uncorks new rules for liquor and cannabis