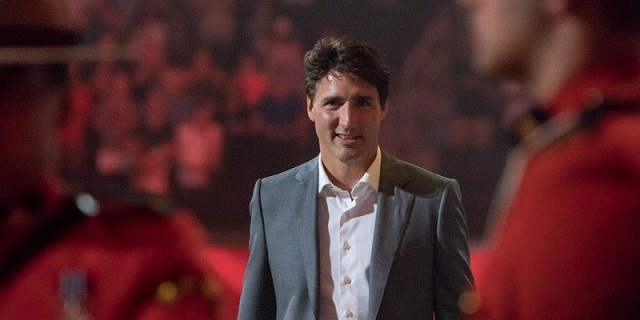
Alberta
Alberta cracking down on mask exemptions – Note required
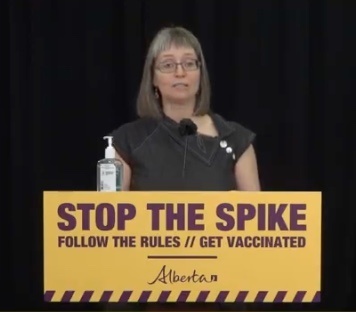
Masking exceptions for health conditions
- Starting May 13, the rules around exemptions from wearing a mask due to a medical condition are changing. Individuals will now be required to obtain a medical exception letter verifying their health condition from an authorized health-care provider.
- The medical exception letter must come from a nurse practitioner, physician or psychologist. It may be presented when in a public setting, if requested by enforcement officials or retrospectively in court if a ticket is issued.
- This is modelled after the approaches currently used in Saskatchewan and other provinces.
Update 221: COVID-19 pandemic in Alberta (May 13, 4:15 p.m.)
Cases remain high in all parts of Alberta. Continue following the restrictions in place to stop the spread of COVID-19 and protect the health-care system.
Latest updates
- Over the last 24 hours, 1,558 new cases were identified.
- There are 722 people in hospital due to COVID-19, including 177 in intensive care.
- There are 24,586 active cases in the province.
- To date, 188,475 Albertans have recovered from COVID-19.
- In the last 24 hours, there were nine additional COVID-related deaths reported: one on April 28, one on May 8, two on May 10, one on May 11, three on May 12, and one on May 13.
- The testing positivity rate was 10.6 per cent.
- There were 15,266 tests (4,375,995 total) completed in the last 24 hours and a total of 2,103,334 people tested overall.
- All zones across the province have cases:
- Calgary Zone: 11,584 active cases and 75,055 recovered
- South Zone: 1,255 active cases and 10,227 recovered
- Edmonton Zone: 5,470 active cases and 67,097 recovered
- North Zone: 3,618 active cases and 20,117 recovered
- Central Zone: 2,647 active cases and 15,961 recovered
- 12 active cases and 18 recovered cases in zones to be confirmed
- Additional information, including case totals, is online.
- Alberta has identified 276 additional cases of variants of concern, bringing the provincial total to 39,989.
- Currently, 907 schools, about 38 per cent, are on alert or have outbreaks, with 6,736 cases in total.
- 439 schools are on alert, with 1,067 total cases.
- Outbreaks are declared in 468 schools, with a total of 5,669 cases.
- In-school transmission has likely occurred in 818 schools. Of these, 273 have had only one new case occur as a result.
- There are currently 115 active and 9,487 recovered cases at long-term care facilities and supportive/home living sites.
- To date, 1,251 of the 2,121 reported deaths (59 per cent) have been in long-term care facilities or supportive/home living sites.
COVID-19 vaccination program
- As of May 12, 2,019,714 doses of COVID-19 vaccine have been administered in Alberta, with 38 per cent of the population having received at least one dose. There are now 322,247 Albertans fully vaccinated with two doses.
- All Albertans age 12 and older are eligible to book appointments through AHS or a participating pharmacy provincewide.
- Legislation now allows Albertans up to three hours of paid, job-protected leave to get a COVID-19 vaccine.
New vaccination campaign launches
- Back to Normal is a new phase of Alberta’s vaccination campaign, intended to emphasize the crucial importance of Albertans getting vaccinated so life can return to normal.
- This advertisement is the first element of the campaign. Additional advertising showing other aspects of daily life will be released soon.
Masking exceptions for health conditions
- Starting May 13, the rules around exemptions from wearing a mask due to a medical condition are changing. Individuals will now be required to obtain a medical exception letter verifying their health condition from an authorized health-care provider.
- The medical exception letter must come from a nurse practitioner, physician or psychologist. It may be presented when in a public setting, if requested by enforcement officials or retrospectively in court if a ticket is issued.
- This is modelled after the approaches currently used in Saskatchewan and other provinces.
Restrictions in place for high case regions
- Restrictions are in place. Outdoor gatherings are limited to five people, most schools have moved to online learning, retail capacity is reduced and in-person dining and services are not allowed at restaurants, bars and cafés.
- Municipalities that have fewer than 50 cases per 100,000 people and/or fewer than 30 active cases are able to return to Step 0 level restrictions.
Enforcement of public health measures
- Fines for non-compliance with public health measures have doubled to $2,000.
- Unpaid fines are backstopped with stronger fine collection actions and restrictions on registry services. For example, a person may have to pay their outstanding fine before they can renew their driver’s licence.
- Repeat offenders will be targeted with a new multi-agency enforcement framework.
- Tickets can be given at the time of an incident or post-infraction – someone who isn’t charged immediately may receive a ticket after authorities do further investigation.
Rapid testing
- The province has launched a new rapid testing partnership with Alberta Chambers of Commerce.
- Businesses and service providers are no longer required to have a health-care provider oversee their rapid testing program.
- Rapid tests are available for employers.
Continuing care
- Restrictions for visitors to continuing care facilities have been eased.
- These changes will vary by site based on the design of the building, wishes of residents and other factors.
- Each site must develop their own visiting approach that falls within the guidelines set out and reflects the risk tolerance of the residents who live at that site.
COVID Care Teams outreach
- If you or others in your home have been directed to self-isolate/quarantine by Alberta Health Services and are unable to do so safely at home, please contact 211 to discuss options, including accessing an assigned hotel to safely isolate (free of charge). Financial assistance may also be available in the amount of $625, upon completion of the self-isolation period.
Albertans downloading tracer app
- All Albertans are encouraged to download the secure ABTraceTogether app, which is integrated with provincial contact tracing. The federal app is not a contact tracing app.
- Secure contact tracing is an effective tool to stop the spread by notifying people who were exposed to a confirmed case so they can isolate and be tested.
- As of May 13, 314,511 Albertans were using the ABTraceTogether app, 69 per cent on iOS and 31 per cent on Android.
- Secure contact tracing is a cornerstone of Alberta’s Relaunch Strategy.
MyHealth Records quick access
- Parents and guardians can access the COVID-19 test results for children under the age of 18 through MyHealth Records (MHR) as soon as they are ready.
- More than 600,000 Albertans have MHR accounts.
Addiction and mental health supports
- Confidential supports are available. The Mental Health Help Line at 1-877-303-2642 and the Addiction Help Line at 1-866-332-2322 operate 24 hours a day, seven days a week. Resources are also available online.
- The Kids Help Phone is available 24-7 and offers professional counselling, information and referrals and volunteer-led, text-based support to young people by texting CONNECT to 686868.
- Online resources provide advice on handling stressful situations and ways to talk with children.
Family violence prevention
- A 24-hour Family Violence Information Line at 310-1818 provides anonymous help in more than 170 languages.
- Alberta’s One Line for Sexual Violence is available at 1-866-403-8000, from 9 a.m. to 9 p.m.
- People fleeing family violence can call local police or the nearest RCMP detachment to apply for an Emergency Protection Order, or follow the steps in the Emergency Protection Orders Telephone Applications (COVID-19).
- Information sheets and other resources on family violence prevention are at alberta.ca/COVID19.
Alberta’s government is responding to the COVID-19 pandemic by protecting lives and livelihoods with precise measures to bend the curve, sustain small businesses and protect Alberta’s health-care system.
Quick facts
- Legally, all Albertans must physically distance and isolate when sick or with symptoms.
- Good hygiene is your best protection: wash your hands regularly for at least 20 seconds, avoid touching your face, cough or sneeze into an elbow or sleeve, and dispose of tissues appropriately.
- Please share acts of kindness during this difficult time at #AlbertaCares.
- Alberta Connects Contact Centre (310-4455) is open Monday to Friday, 8:15 a.m. to 4:30 p.m.
Alberta
Alberta awash in corporate welfare

From the Fraser Institute
By Matthew Lau
To understand Ottawa’s negative impact on Alberta’s economy and living standards, juxtapose two recent pieces of data.
First, in July the Trudeau government made three separate “economic development” spending announcements in Alberta, totalling more than $80 million and affecting 37 different projects related to the “green economy,” clean technology and agriculture. And second, as noted in a new essay by Fraser Institute senior fellow Kenneth Green, inflation-adjusted business investment (excluding residential structures) in Canada’s extraction sector (mining, quarrying, oil and gas) fell 51.2 per cent from 2014 to 2022.
The productivity gains that raise living standards and improve economic conditions rely on business investment. But business investment in Canada has declined over the past decade and total economic growth per person (inflation-adjusted) from Q3-2015 through to Q1-2024 has been less than 1 per cent versus robust growth of nearly 16 per cent in the United States over the same period.
For Canada’s extraction sector, as Green documents, federal policies—new fuel regulations, extended review processes on major infrastructure projects, an effective ban on oil shipments on British Columbia’s northern coast, a hard greenhouse gas emissions cap targeting oil and gas, and other regulatory initiatives—are largely to blame for the massive decline in investment.
Meanwhile, as Ottawa impedes private investment, its latest bundle of economic development announcements underscores its strategy to have government take the lead in allocating economic resources, whether for infrastructure and public institutions or for corporate welfare to private companies.
Consider these federally-subsidized projects.
A gas cloud imaging company received $4.1 million from taxpayers to expand marketing, operations and product development. The Battery Metals Association of Canada received $850,000 to “support growth of the battery metals sector in Western Canada by enhancing collaboration and education stakeholders.” A food manufacturer in Lethbridge received $5.2 million to increase production of plant-based protein products. Ermineskin Cree Nation received nearly $400,000 for a feasibility study for a new solar farm. The Town of Coronation received almost $900,000 to renovate and retrofit two buildings into a business incubator. The Petroleum Technology Alliance Canada received $400,000 for marketing and other support to help boost clean technology product exports. And so on.
When the Trudeau government announced all this corporate welfare and spending, it naturally claimed it create economic growth and good jobs. But corporate welfare doesn’t create growth and good jobs, it only directs resources (including labour) to subsidized sectors and businesses and away from sectors and businesses that must be more heavily taxed to support the subsidies. The effect of government initiatives that reduce private investment and replace it with government spending is a net economic loss.
As 20th-century business and economics journalist Henry Hazlitt put it, the case for government directing investment (instead of the private sector) relies on politicians and bureaucrats—who did not earn the money and to whom the money does not belong—investing that money wisely and with almost perfect foresight. Of course, that’s preposterous.
Alas, this replacement of private-sector investment with public spending is happening not only in Alberta but across Canada today due to the Trudeau government’s fiscal policies. Lower productivity and lower living standards, the data show, are the unhappy results.
Author:
Alberta
‘Fireworks’ As Defence Opens Case In Coutts Two Trial

From the Frontier Centre for Public Policy
By Ray McGinnis
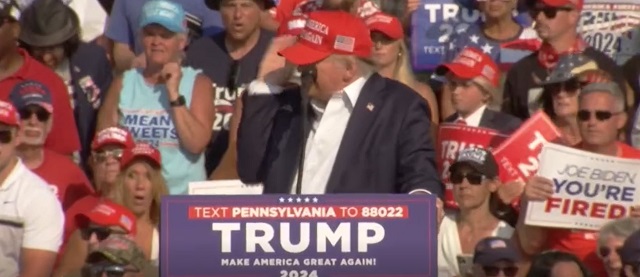
Anthony Olienick and Chris Carbert are on trial for conspiracy to commit murder and firearms charges in relation to the Coutts Blockade into mid-February 2022. In opening her case before a Lethbridge, AB, jury on July 11, Olienick’s lawyer, Marilyn Burns stated “This is a political, criminal trial that is un Canadian.” She told the jury, “You will be shocked, and at the very least, disappointed with how Canada’s own RCMP conducted themselves during and after the Coutts protest,” as she summarized officers’ testimony during presentation of the Crown’s case. Burns also contended that “the conduct of Alberta’s provincial government and Canada’s federal government are entwined with the RCMP.” The arrests of the Coutts Four on the night of February 13 and noon hour of February 14, were key events in a decision by the Clerk of the Privy Council, Janice Charette, and the National Security Advisor to the Prime Minister, Jody Thomas, to advise Prime Minister Justin Trudeau to invoke the Emergencies Act. Chief Justice Paul Rouleau, in submitting his Public Order Emergency Commission Report to Parliament on February 17, 2023, also cited events at the Coutts Blockade as key to his conclusion that the government was justified in invoking the Emergencies Act.
Justice David Labrenz cautioned attorney Burns regarding her language, after Crown prosecutor Stephen Johnson objected to some of the language in the opening statement of Olienick’s counsel. Futher discussion about the appropriateness of attorney Burns’ statement to the jury is behind a publication ban, as discussions occurred without the jury present.
Justice Labrenz told the jury on July 12, “I would remind you that the presumption of innocence means that both the accused are cloaked with that presumption, unless the Crown proves beyond a reasonable doubt the essential elements of the charge(s).” He further clarified what should result if the jurors were uncertain about which narrative to believe: the account by the Crown, or the account from the accused lawyers. Labrenz stated that such ambivalence must lead to an acquittal; As such a degree of uncertainty regarding which case to trust in does not meet the “beyond a reasonable doubt” threshold for a conviction.”
On July 15, 2024, a Lethbridge jury heard evidence from a former employer of Olienicks’ named Brian Lambert. He stated that he had tasked Olienick run his sandstone quarry and mining business. He was a business partner with Olienick. In that capacity, Olienick made use of what Lambert referred to as “little firecrackers,” to quarry the sandstone and reduce it in size. Reducing the size of the stone renders it manageable to get refined and repurposed so it could be sold to buyers of stone for other uses (building construction, patio stones, etc.) Lambert explained that the “firecrackers” were “explosive devices” packaged within tubing and pipes that could also be used for plumbing. He detailed how “You make them out of ordinary plumbing pipe and use some kind of propellant like shotgun powder…” Lambert explained that the length of the pipe “…depended on how big a hole or how large a piece of stone you were going to crack. The one I saw was about six inches long … maybe an inch in diameter.”
One of Olienick’s charges is “unlawful possession of an explosive device for a dangerous purpose.” The principal evidence offered up by RCMP to the Crown is what the officers depicted as “pipe bombs” which they obtained at the residence of Anthony Olienick in Claresholm, Alberta, about a two-hour drive from Coutts. Officers entered his home after he was arrested the night of February 13, 2022. Lambert’s testimony offers a plausible common use for the “firecrackers” the RCMP referred to as “pipe bombs.” Lambert added, these “firecrackers” have a firecracker fuse, and in the world of “explosive” they are “no big deal.”
Fellow accused, Chris Carbert, is does not face the additional charge of unlawful possession of explosives for a dangerous purpose. This is the first full week of the case for the defence. The trial began on June 6 when the Crown began presenting its case.
Ray McGinnis is a Senior Fellow with the Frontier Centre for Public Policy who recently attended several days of testimony at the Coutts Two trial.
-

 International19 hours ago
International19 hours agoSecret Service Repeatedly Rejected Offers To Use Drones At Deadly Trump Rally, Whistleblower Says
-

 Alberta1 day ago
Alberta1 day ago‘Fireworks’ As Defence Opens Case In Coutts Two Trial
-

 Business1 day ago
Business1 day agoEstonia’s solution to Canada’s stagnating economic growth
-

 COVID-191 day ago
COVID-191 day agoLeaked documents: German gov’t lied about shots preventing COVID, knew lockdowns did more harm than good
-

 Business1 day ago
Business1 day agoFederal government seems committed to killing investment in Canada
-

 International1 day ago
International1 day agoSwitzerland’s new portable suicide ‘pod’ set to claim its first life ‘soon’
-
 International20 hours ago
International20 hours agoHouse Passes Bipartisan Resolution Establishing Trump Assassination Attempt Task Force
-
 Bruce Dowbiggin12 hours ago
Bruce Dowbiggin12 hours agoGarbage In, Garbage Out: The Democrats 2024 Election Coup