Health
THE WPATH TAPES: Behind-The-Scenes Recordings Reveal What Top Gender Doctors Really Think About Sex Change Procedures

 From the Daily Caller News Foundation
From the Daily Caller News Foundation
By MEGAN BROCK AND KATE ANDERSON
The World Professional Association for Transgender Health (WPATH) is the leading authority in the field of gender medicine. Its guidance is routinely used by top medical associations in the U.S. and abroad, while its standards of care inform insurance companies’ approach to coverage policies.
But behind closed doors, top WPATH doctors discussed, and at times seemed to challenge, the organization’s own published guidelines for sex change procedures and acknowledged pushing experimental medical interventions that can have devastating and irreversible complications, according to exclusive footage obtained by the Daily Caller News Foundation.
WPATH published highly influential clinical guidance called “Standards of Care for the Health of Transgender and Gender Diverse People, Version 8” (SOC 8), which recommends the use of invasive medical interventions such as puberty blockers, cross-sex hormones and sex change surgeries, calling them “safe and effective.”
The DCNF filed a series of public records requests to WPATH SOC 8 co-authors who are employed at taxpayer-funded institutions, making their emails subject to open records laws. Buried in more than 100 pages of responsive records from the University of Nevada was a series of emails between prominent WPATH members and leaders, including WPATH Global Education Institute (GEI) Co-Chair Gail Knudson, that were sent in 2022. In one email, Knudson sent a colleague the link to a folder containing nearly 30 hours of recordings from WPATH’s GEI summit in September 2022 in Montreal, Canada, which included sessions on mental health, puberty blockers, cross-sex hormones and sex change surgery.
These sessions provided WPATH members with in-depth education on the clinical application of topics addressed in the SOC 8 treatment guidelines. However, the footage reveals WPATH-affiliated doctors advocating for children to undergo risky sex change procedures and even pushing for these treatments for patients struggling with severe mental health issues. Several sessions were dedicated exclusively to treating children and included recommendations for minors to receive puberty blockers, cross-sex hormones and surgeries.
For instance, WPATH guidance recommends addressing a patient’s mental health issues before giving them sex change medical interventions. However, in one recorded session, a WPATH faculty member and gender doctor claimed that mental health issues don’t necessarily affect a patient’s ability to receive cross-sex hormones.
In another video, a doctor told attendees children should be informed that cross-sex hormones will likely make them infertile but admitted that he will prescribe them anyway if a child says they want the treatment, regardless of the future consequences.
A surgeon euphemistically referred to a phalloplasty procedure, a surgical series that includes obliterating the vaginal cavity and creating a fake penis with harvested tissue, as an “adventure” for young people. He did this despite later admitting that those same procedures will “definitely” have “complications,” such as permanent issues with bladder function and tissue death.
One physician called the entire field of cross-sex hormones “off-label,” referring to the concept of drugs being used for alternative purposes than what they were approved for. The doctor went on to say that female patients might actually appreciate drug side effects that cause them to lose hair, because they’d look “more like men.”
The Food and Drug Administration says that when it approves a drug, healthcare providers generally may prescribe that drug for an unapproved use, or off-label, when “they judge that it is medically appropriate for their patient.”
In several other videos, doctors argued in favor of transitioning patients who experience psychotic episodes. One admitted that some of his patients with schizophrenia have to be careful how much cross-sex hormones they take or they can’t “keep the voices down.”
The DCNF consulted medical professionals from respected organizations, such as Do No Harm, who all argued that the comments from WPATH-affiliated doctors show that the transgender medical industry does not have patients’ best interests at heart.
While the average person, nationally and internationally, likely has never heard of WPATH, the modern medical industry is deeply tied to the organization and relies on it to dictate the standards of care for transgender medicine. WPATH’s guidelines are cited as criteria for obtaining insurance coverage by both private insurance companies and tax-funded insurance plans, positioning them as a lynchpin of the sex reassignment industry.
Additionally, their guidelines help inform policy statements from major medical and professional organizations, such as the American Academy of Pediatrics (AAP), the American Psychological Association and the Endocrine Society. The AAP is currently being sued by Isabelle Ayala, a former patient who was medically transitioned as a child, for allegedly rushing her through sex change medical procedures.
There’s been an explosion in the number of young people, including children, being put on hormones and puberty blockers and getting sex change surgeries, according to a study published in August 2023 by the JAMA Network. This surge has been fueled, in part, by groups like Planned Parenthood, which distributes cross-sex hormones to patients as young as 16. Planned Parenthood saw a roughly 125% jump in the number of transgender services it provided between 2020 and 2022.
Twenty-three states, however, have enacted legislation preventing doctors from performing sex change surgeries on minors amid backlash from concerned parents and doctors who don’t subscribe to the WPATH-endorsed “gender-affirming care” model. Gender-affirming care is another euphemism used by medical professionals to describe the idea that doctors should affirm a patient’s wish to live as the opposite biological sex through social transitioning, hormone therapy and even surgery.
The SOC 8 was released just days ahead of the 2022 symposium and contained several significant changes to how doctors and medical institutions implemented transgender medical treatment. For instance, WPATH removed minimum age requirements criteria that established when a child can or should receive transgender medical services such as puberty blockers, cross-sex hormones, and sex reassignment surgeries.
WPATH’s previous guidelines recommended that hormone therapy be given once a patient was over the age of 16, but the updated version removed this barrier and suggests hormone therapy begin at the first signs of sexual maturity.
The videos obtained by the DCNF give the first glimpse at how doctors and mental health professionals discussed implementing the new guidelines. To highlight the most significant portions of the content obtained in the records requests, the DCNF has decided to publish a series of articles collectively called “The WPATH Tapes.”
Following this release, the DCNF intends to publish all of the videos in their entirety in order to provide the public with necessary information about WPATH’s approach to medical care and shine a light on an influential organization that has largely remained anonymous until now.
The WPATH Tapes Table of Contents:
- Video Shows Prominent Doctors Acknowledging, And Even Challenging, The Experimental Nature Of Sex Change Drugs
- Top Psychiatrist Argues Schizophrenic Patients Can Consent To Sex Change Surgeries
- ‘Keep The Voices Down’: In Unearthed Video, Doctors Discuss Putting Mentally Ill Patients, Including Kids, On Hormones
- Gender Doctor Calls Genital Surgery An ‘Adventure’ For Young People While Describing Grisly Complications
- ‘No Idea About Their Fertility’: Gender Doctors Shed Light On Grim Reality Facing Kids Considering Sex Changes
- Leader Of Gender Medicine Org Says Binary Sex ‘Doesn’t Really Hold True,’ Cheers On ‘Deconstructed’ Biology
- Private Footage Reveals Leading Medical Org’s Efforts To ‘Normalize’ Gender Ideology
Business
RFK Jr. says Hep B vaccine is linked to 1,135% higher autism rate

From LifeSiteNews
By Matt Lamb
They got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data
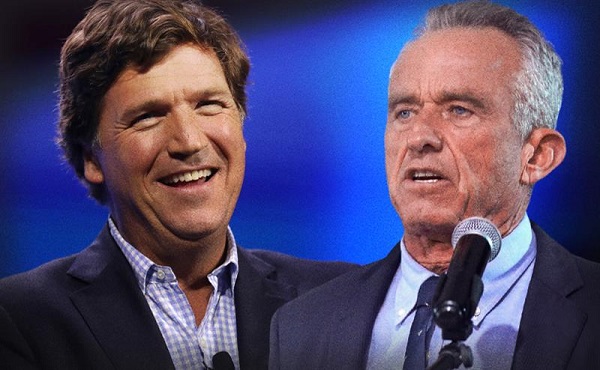
The Centers for Disease Control and Prevention (CDC) found newborn babies who received the Hepatitis B vaccine had 1,135-percent higher autism rates than those who did not or received it later in life, Robert F. Kennedy Jr. told Tucker Carlson recently. However, the CDC practiced “trickery” in its studies on autism so as not to implicate vaccines, Kennedy said.
RFK Jr., who is the current Secretary of Health and Human Services, said the CDC buried the results by manipulating the data. Kennedy has pledged to find the causes of autism, with a particular focus on the role vaccines may play in the rise in rates in the past decades.
The Hepatitis B shot is required by nearly every state in the U.S. for children to attend school, day care, or both. The CDC recommends the jab for all babies at birth, regardless of whether their mother has Hep B, which is easily diagnosable and commonly spread through sexual activity, piercings, and tattoos.
“They kept the study secret and then they manipulated it through five different iterations to try to bury the link and we know how they did it – they got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data,” Kennedy told Carlson for an episode of the commentator’s podcast. “And they did a lot of other tricks and all of those studies were the subject of those kind of that kind of trickery.”
But now, Kennedy said, the CDC will be conducting real and honest scientific research that follows the highest standards of evidence.
“We’re going to do real science,” Kennedy said. “We’re going to make the databases public for the first time.”
He said the CDC will be compiling records from variety of sources to allow researchers to do better studies on vaccines.
“We’re going to make this data available for independent scientists so everybody can look at it,” the HHS secretary said.
— Matt Lamb (@MattLamb22) July 1, 2025
Health and Human Services also said it has put out grant requests for scientists who want to study the issue further.
Kennedy reiterated that by September there will be some initial insights and further information will come within the next six months.
Carlson asked if the answers would “differ from status quo kind of thinking.”
“I think they will,” Kennedy said. He continued on to say that people “need to stop trusting the experts.”
“We were told at the beginning of COVID ‘don’t look at any data yourself, don’t do any investigation yourself, just trust the experts,”‘ he said.
In a democracy, Kennedy said, we have the “obligation” to “do our own research.”
“That’s the way it should be done,” Kennedy said.
He also reiterated that HHS will return to “gold standard science” and publish the results so everyone can review them.
International
RFK Jr. tells Tucker how Big Pharma uses ‘perverse incentives’ to get vaccines approved
From LifeSiteNews
By Matt Lamb
Kennedy defended his decision to fire all 17 members of the Advisory Committee on Immunization Practices, which he decried as a tool used to “rubber stamp” vaccines.
The vaccine approval process is a “bundle of perverse incentives” since pharmaceutical companies stand to make billions of dollars in revenue from it, Secretary of Health and Human Services Robert F. Kennedy Jr. told Tucker Carlson recently.
Kennedy appeared on Carlson’s show yesterday to discuss a variety of issues, including the potential link between autism and vaccines and his overhauling of the vaccine advisory committee at the Centers for Disease Control and Prevention last month.
Twenty years ago, Bobby Kennedy was exiled from polite society for suggesting a link between autism and vaccines. Now he’s a cabinet secretary, and still saying it.
(0:00) The Organized Opposition to RFK’s Mission
(6:46) Uncovering the Reason for Skyrocketing Rates of Autism… pic.twitter.com/g8T8te3kNC— Tucker Carlson (@TuckerCarlson) June 30, 2025
Kennedy began by explaining that Big Pharma has been targeting academic journals to ensure its products receive favorable reviews.
“The journals won’t publish anything critical of vaccines … there’s so much pressure on them. They’re funded by pharmaceutical companies, and they’ll lose advertising and revenue from reprints,” Kennedy said.
Kennedy then noted that Big Pharma will “pay to get something published in these journals,” before accusing industry leaders of pushing drugs on doctors and of hiring “mercenary scientists” to manipulate data until their product is deemed safe and effective.
The entire complex is broken due to the “perverse incentives,” he lamented.
Later in the interview, Kennedy defended his decision to fire all 17 members of the Advisory Committee on Immunization Practices (ACIP) in June, which he decried as a mere tool to “rubber stamp” vaccines.
It served as “a sock puppet for the industry that it was supposed to regulate,” Kennedy exclaimed, citing conflicts of interest for the overwhelming majority of its board members.
This sort of “agency capture” explains the lucrative nature of vaccines, he added.
— Matt Lamb (@MattLamb22) July 1, 2025
Kennedy then summarized the “perverse” process as follows:
First of all, the federal government often times actually designs the vaccine, [the National Institutes of Health] would design it, would hand it over to the pharmaceutical company. The pharmaceutical company then runs it … first through [the] FDA, then through [the] ACIP, and gets it recommended.
If you can get that recommendation you now got a billion dollars in — at least — revenues by the end of the year, every year, forever. So, there was a gold rush to add new vaccines to the schedule and ACIP never turned away a single vaccine … that came to them they recommended, and a lot of these vaccines are for diseases that are not even casually contagious.
Kennedy further pointed to the Hepatitis B shot for newborns as an example of how the industry has been corrupted.
In 1999, the CDC “looked at children who had received the hepatitis vaccine within the first 30 days of life and compared those children to children who had received the vaccine later — or not at all. And they found an 1,135% elevated risk of autism among the vaccinated children. It shocked them. They kept the study secret and manipulated it through five different iterations to try to bury the link,” he said.
“We want to protect public health,” Kennedy explained, but “these vaccines … can cause chronic disease, chronic injuries that last a lifetime.”
-
 International2 days ago
International2 days agoCBS settles with Trump over doctored 60 Minutes Harris interview
-

 Business2 days ago
Business2 days agoWhy it’s time to repeal the oil tanker ban on B.C.’s north coast
-

 Crime1 day ago
Crime1 day agoBryan Kohberger avoids death penalty in brutal killing of four Idaho students
-

 Business2 days ago
Business2 days agoLatest shakedown attempt by Canada Post underscores need for privatization
-

 Energy2 days ago
Energy2 days agoIf Canada Wants to be the World’s Energy Partner, We Need to Act Like It
-

 Alberta1 day ago
Alberta1 day agoPierre Poilievre – Per Capita, Hardisty, Alberta Is the Most Important Little Town In Canada
-

 MxM News1 day ago
MxM News1 day agoUPenn strips Lia Thomas of women’s swimming titles after Title IX investigation
-

 COVID-191 day ago
COVID-191 day agoTop COVID doctor given one of Canada’s highest honors