Health
The People Cheering Brian Thompson’s Murder Can’t Have the Medical Utopia That They Want

Whether private or public, third-party payment for health care is a huge problem.
Evoking a collective scream of despair from socialists and anti-corporate types, police in Pennsylvania arrested Luigi Mangione, a suspect in the murder of UnitedHealthcare CEO Brian Thompson. Thompson, they insist, stood in the way of the sort of health care they think they deserve and shooting him down on the street was some sort of bloody-minded strike for justice.
The assassin’s fans—and the legal system has yet to convict anybody for the crime—are moral degenerates. But they’re also dreaming, if they think insurance executives like Thompson are all that stands between them and their visions of a single-payer medical system that satisfies every desire. While there is a lot wrong with the main way health care is paid for and delivered in the U.S., what the haters want is probably not achievable, and the means many of them prefer would make things worse.
“Unlimited Care…Free of Charge”
“It is an old joke among health policy wonks that what the American people really want from health care reform is unlimited care, from the doctor of their choice, with no wait, free of charge,” Michael Tanner, then of the Cato Institute, quipped in 2017.
The problem, no matter how health care is delivered, is that it requires labor, time, and resources that are available in finite supply. Somebody must decide how to allocate medications, treatments, physicians, and hospital beds, and how to pay for it all. A common assumption in some circles is that Americans ration medicine by price, handing an advantage to the wealthy and sticking it to the poor.
“Today, as everyone knows, health care in the US can be prohibitively expensive even for people who have insurance,” Dylan Scott sniffed this week at Vox.
The alternative, supposedly, is one where health care is “universal,” with bills paid by government so everybody has access to care. Except, most Americans rely on somebody else to pay the bulk of their medical bills just like Canadians, Germans, and Britons. And while there are huge differences among the systems presented as alternatives to the one in the U.S., third-party payers—whether governments or insurance companies—do enormous damage to the provision of health care.
Third-Party Payers, Both Public and Private, Raise Costs
“Contrary to ‘conventional wisdom,’ health insurance—private or otherwise—does not make health care more affordable,” Jeffrey Singer, a surgeon and senior fellow with the Cato Institute, wrote in 2013. “The third party payment system is the principal force behind health care price inflation.”
In the U.S., the dominance of third-party payment, whether Thompson’s UnitedHealthcare, one of its competitors, Medicare, Medicaid, or something else, makes it difficult to know the price for procedures, medicines, and treatments—because there really isn’t one price when third-party payers are involved.
Several years ago, the first Trump administration required hospitals to publish prices for services. My local hospital offers an Excel spreadsheet with wildly varying prices for procedures and services, from different categories of self-pay, Medicare, Medicaid, and negotiated rates for competing insurance plans.
“A colonoscopy might cost you or your insurer a few hundred dollars—or several thousand, depending on which hospital or insurer you use,” NPR’s Julie Appleby pointed out in 2021.
That said, savvy patients paying their own bills can usually get a lower price than that paid by insurance.
“When government, lawyers, or third party insurance is responsible for paying the bills, consumers have no incentive to control costs,” Arthur Laffer, Donna Arduin, and Wayne Winegarden wrote in the 2009 paper, The Prognosis for National Health Insurance. After all, the premium or tax is already paid, right?
Other Countries Struggle With Similar Issues
Concerns about rising costs, demand, and finite resources apply just as much when the payer is the government.
“State health insurance patients are struggling to see their doctors towards the end of every quarter, while privately insured patients get easy access,” Germany’s Deutsche Welle reported in 2018. “The researchers traced the phenomenon to Germany’s ‘budget’ system, which means that state health insurance companies only reimburse the full cost of certain treatments up to a particular number of patients or a particular monetary value.” Budgeting is quarterly, and once it’s exhausted, that’s it.
Last year in the U.K., a Healthwatch report complained: “We’re seeing a two-tier system emerge, where healthcare is accessible only to those who can afford it, with one in seven people who responded to our poll advised to seek private care by NHS [National Health Service] staff.” Britain’s NHS remains popular, but it has long struggled with the demand and expense for cancer care and other expensive treatments.
And Canada’s single-payer system famously relies heavily on long wait times to ration care. “In 2023, physicians report a median wait time of 27.7 weeks between a referral from a general practitioner and receipt of treatment,” the Fraser Institute found last year. “This represents the longest delay in the survey’s history and is 198% longer than the 9.3 weeks Canadian patients could expect to wait in 1993.”
You have to wonder what those so furious at Brian Thompson that they would applaud his murder would say about the officials managing systems elsewhere. None of them deliver “unlimited care, from the doctor of their choice, with no wait, free of charge.” Some lack the minimal discipline imposed by what competition exists among insurers in the U.S.
We Need Less Government Involvement in Medicine
“Policymakers need to understand that the key to ‘affordable health care’ is not to increase the role of health insurance in peoples’ lives, but to diminish it,” Cato’s Singer concluded.
My family found that true when we contracted with a primary care practice that refuses insurance. We pay fixed annual fees, which includes exams, laboratory services, and some procedures. My doctor caught my atrial fibrillation when he walked me across his clinic hall on a hunch to run an EKG.
The Surgery Center of Oklahoma famously follows a similar model for much more than primary care. It publishes its prices, which don’t include the overhead and uncertainty of dealing with third-party payers.
Those examples point to a better health care system than what exists in the United States—or in most other countries, for that matter. They’re probably not the whole answer, because it’s unlikely that one approach will suit millions of people with different medical concerns, incomes, and preferences. But making people more, rather than less, responsible for their own health care, and getting government and other third-parties as far out of the matter as possible, is far better than cheering the murder of people who supposedly stand between us and an imaginary medical utopia.
|
|
|
Business
National dental program likely more costly than advertised

From the Fraser Institute
By Matthew Lau
At the beginning of June, the Canadian Dental Care Plan expanded to include all eligible adults. To be eligible, you must: not have access to dental insurance, have filed your 2024 tax return in Canada, have an adjusted family net income under $90,000, and be a Canadian resident for tax purposes.
As a result, millions more Canadians will be able to access certain dental services at reduced—or no—out-of-pocket costs, as government shoves the costs onto the backs of taxpayers. The first half of the proposition, accessing services at reduced or no out-of-pocket costs, is always popular; the second half, paying higher taxes, is less so.
A Leger poll conducted in 2022 found 72 per cent of Canadians supported a national dental program for Canadians with family incomes up to $90,000—but when asked whether they would support the program if it’s paid for by an increase in the sales tax, support fell to 42 per cent. The taxpayer burden is considerable; when first announced two years ago, the estimated price tag was $13 billion over five years, and then $4.4 billion ongoing.
Already, there are signs the final cost to taxpayers will far exceed these estimates. Dr. Maneesh Jain, the immediate past-president of the Ontario Dental Association, has pointed out that according to Health Canada the average patient saved more than $850 in out-of-pocket costs in the program’s first year. However, the Trudeau government’s initial projections in the 2023 federal budget amounted to $280 per eligible Canadian per year.
Not all eligible Canadians will necessarily access dental services every year, but the massive gap between $850 and $280 suggests the initial price tag may well have understated taxpayer costs—a habit of the federal government, which over the past decade has routinely spent above its initial projections and consistently revises its spending estimates higher with each fiscal update.
To make matters worse there are also significant administrative costs. According to a story in Canadian Affairs, “Dental associations across Canada are flagging concerns with the plan’s structure and sustainability. They say the Canadian Dental Care Plan imposes significant administrative burdens on dentists, and that the majority of eligible patients are being denied care for complex dental treatments.”
Determining eligibility and coverage is a huge burden. Canadians must first apply through the government portal, then wait weeks for Sun Life (the insurer selected by the federal government) to confirm their eligibility and coverage. Unless dentists refuse to provide treatment until they have that confirmation, they or their staff must sometimes chase down patients after the fact for any co-pay or fees not covered.
Moreover, family income determines coverage eligibility, but even if patients are enrolled in the government program, dentists may not be able to access this information quickly. This leaves dentists in what Dr. Hans Herchen, president of the Alberta Dental Association, describes as the “very awkward spot” of having to verify their patients’ family income.
Dentists must also try to explain the program, which features high rejection rates, to patients. According to Dr. Anita Gartner, president of the British Columbia Dental Association, more than half of applications for complex treatment are rejected without explanation. This reduces trust in the government program.
Finally, the program creates “moral hazard” where people are encouraged to take riskier behaviour because they do not bear the full costs. For example, while we can significantly curtail tooth decay by diligent toothbrushing and flossing, people might be encouraged to neglect these activities if their dental services are paid by taxpayers instead of out-of-pocket. It’s a principle of basic economics that socializing costs will encourage people to incur higher costs than is really appropriate (see Canada’s health-care system).
At a projected ongoing cost of $4.4 billion to taxpayers, the newly expanded national dental program is already not cheap. Alas, not only may the true taxpayer cost be much higher than this initial projection, but like many other government initiatives, the dental program already seems to be more costly than initially advertised.
Business
RFK Jr. says Hep B vaccine is linked to 1,135% higher autism rate

From LifeSiteNews
By Matt Lamb
They got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data
The Centers for Disease Control and Prevention (CDC) found newborn babies who received the Hepatitis B vaccine had 1,135-percent higher autism rates than those who did not or received it later in life, Robert F. Kennedy Jr. told Tucker Carlson recently. However, the CDC practiced “trickery” in its studies on autism so as not to implicate vaccines, Kennedy said.
RFK Jr., who is the current Secretary of Health and Human Services, said the CDC buried the results by manipulating the data. Kennedy has pledged to find the causes of autism, with a particular focus on the role vaccines may play in the rise in rates in the past decades.
The Hepatitis B shot is required by nearly every state in the U.S. for children to attend school, day care, or both. The CDC recommends the jab for all babies at birth, regardless of whether their mother has Hep B, which is easily diagnosable and commonly spread through sexual activity, piercings, and tattoos.
“They kept the study secret and then they manipulated it through five different iterations to try to bury the link and we know how they did it – they got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data,” Kennedy told Carlson for an episode of the commentator’s podcast. “And they did a lot of other tricks and all of those studies were the subject of those kind of that kind of trickery.”
But now, Kennedy said, the CDC will be conducting real and honest scientific research that follows the highest standards of evidence.
“We’re going to do real science,” Kennedy said. “We’re going to make the databases public for the first time.”
He said the CDC will be compiling records from variety of sources to allow researchers to do better studies on vaccines.
“We’re going to make this data available for independent scientists so everybody can look at it,” the HHS secretary said.
— Matt Lamb (@MattLamb22) July 1, 2025
Health and Human Services also said it has put out grant requests for scientists who want to study the issue further.
Kennedy reiterated that by September there will be some initial insights and further information will come within the next six months.
Carlson asked if the answers would “differ from status quo kind of thinking.”
“I think they will,” Kennedy said. He continued on to say that people “need to stop trusting the experts.”
“We were told at the beginning of COVID ‘don’t look at any data yourself, don’t do any investigation yourself, just trust the experts,”‘ he said.
In a democracy, Kennedy said, we have the “obligation” to “do our own research.”
“That’s the way it should be done,” Kennedy said.
He also reiterated that HHS will return to “gold standard science” and publish the results so everyone can review them.
-

 Agriculture2 days ago
Agriculture2 days agoCanada’s supply management system is failing consumers
-

 Business1 day ago
Business1 day agoCanada’s loyalty to globalism is bleeding our economy dry
-

 Alberta1 day ago
Alberta1 day agoCOVID mandates protester in Canada released on bail after over 2 years in jail
-

 armed forces1 day ago
armed forces1 day agoCanada’s Military Can’t Be Fixed With Cash Alone
-
 Alberta24 hours ago
Alberta24 hours agoAlberta Next: Alberta Pension Plan
-

 International1 day ago
International1 day agoTrump transportation secretary tells governors to remove ‘rainbow crosswalks’
-
 Business1 day ago
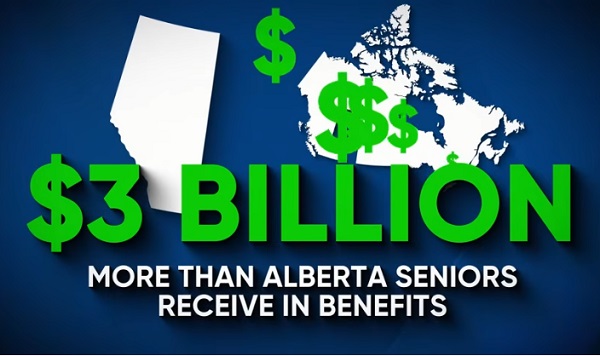
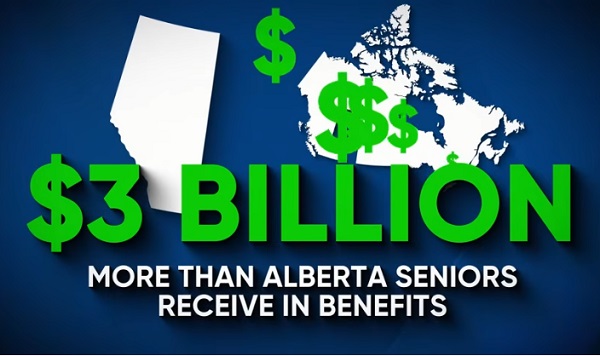
Business1 day agoCarney’s spending makes Trudeau look like a cheapskate
-

 Crime2 days ago
Crime2 days agoProject Sleeping Giant: Inside the Chinese Mercantile Machine Linking Beijing’s Underground Banks and the Sinaloa Cartel