Addictions
The new drug agency tasked with improving Canada’s medication practices

By Alexandra Keeler
A recent report calls on the newly-created Canada’s Drug Agency to implement a strategy to improve prescription medication practices
As Canada moves toward establishing a national drug agency, a new report has outlined recommendations for a prescription medications strategy that the agency should be tasked with implementing.
The report, released July 26 by the Canadian Drug Agency Transition Office, calls on the newly established Canada’s Drug Agency to implement a nation-wide strategy for the appropriate use of prescription medications. The transition office is a temporary government initiative responsible for developing the drug agency’s mandate and plan.
“Part of the opioid crisis has been linked to prescribing particular medications, and the dependency that people can develop with respect to certain medications,” said Stephen Samis, chair of the Appropriate Use Advisory Committee, which helped guide the development of the medications strategy outlined in the report.
“If there’s a way to help get people off of those medications in a safe and effective way, and by the use of alternatives to the medication, that’s really important,” said Samis, who formerly served as deputy health minister in the Yukon.
Canada’s Drug Agency, which was first announced by Health Minister Mark Holland in December 2023, is tasked with managing and coordinating Canada’s pharmaceutical system across the provinces and territories. It has begun establishing advisory bodies, building partnerships and conducting research.
Under Canada’s proposed pharmacare legislation, the drug agency will also be responsible for identifying the essential prescription drugs to which Canadians should have access under pharmacare.
Subscribe for free to get BTN’s latest news and analysis – or donate to our investigative journalism fund.
Primary care crisis
The report proposes six guiding principles for improving Canada’s prescription and medication use practices. These include providing more personalized primary care to patients, ensuring careful oversight of prescription medications and improving coordination between health-care providers.
Currently, more than one in five Canadian adults — about 6.5 million people — lack access to primary care, according to a May 2024 study in the Canadian Medical Association Journal. Primary care refers to health care that is regular and ongoing, such as doctor check-ups or management of chronic conditions.
“The crisis in primary care right now is really one of those potential barriers to people receiving appropriate medication with a provider that they have a relationship with,” said Samis.
The lack of access to primary care can lead to problems such as inconsistent prescribing, inadequate follow-up and insufficient patient education on prescription medications, the report says.
About 1.9 million Canadian seniors use at least one prescription medication inappropriately. This costs them and the health-care system an estimated $1.4 billion in direct and indirect costs, the report says.
“Benzodiazepines, sleeping pills … even things like medications that control heartburn. If people are on them for too long, [it] can have other kinds of side effects,” said Samis.
“Same thing with opioid related medications. It’s really important that people have medications they need so that they don’t develop dependencies.”
The report also notes that fragmented information systems and poor coordination between service providers complicate medication management — resulting in duplicate prescriptions, contradictory treatment plans and gaps in care.
“What happens often is that somebody is in primary care, and their data is over here,” said Samis. “They go into long-term care, and that information doesn’t follow them. They get prescribed new things in long-term care, they go into the hospital, then the long-term care information system might not be speaking to the hospital information system.”
‘Neutral space’
Samis says he is optimistic that Canada’s Drug Agency will be able to address some of the problematic medication practices identified in the report.
Samis will co-chair a new committee responsible for assisting with the implementation of the report’s recommendations.
“We have a diverse and knowledgeable group joining our newly established Appropriate Use Advisory Committee, with the inaugural meeting to take place on September 13,” a media relations spokesperson for Canada’s Drug Agency’s told Canadian Affairs in a written statement.
Samis envisions the agency as a “neutral space” to address health-care issues and resolve conflicts between governments and health-care providers.
“This approach avoids the conflicts that often arise between jurisdictions, levels of government, or between government and [health-care] providers,” he said.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Break The Needle. Our content is always free – but if you want to help us commission more high-quality journalism, consider getting a voluntary paid subscription.
Addictions
After eight years, Canada still lacks long-term data on safer supply
By Alexandra Keeler
Canada has spent more than $100 million on safer supply programs, but has failed to research their long-term effects
Canada lacks long-term data on safer supply programs, despite funding these programs for years.
Safer supply programs dispense pharmaceutical opioids as a replacement for toxic street drugs.
There is a growing body of research on safer supply’s short-term health effects. But there are no Canadian studies that evaluate program participants’ health impacts beyond 18 months.
The absence of research into long-term data on safer supply means policymakers do not understand how safer supply affects participants’ health, substance use or social outcomes over time.
“Long-term data is important because it helps us understand not just short-term health outcomes like reduced overdoses, but also broader impacts on quality of life, stability and health care use,” said Farihah Ali, scientific lead at the Institute for Mental Health Policy Research at CAMH. The Centre for Addiction and Mental Health is one of Canada’s leading centres for addiction research and clinical care.
Pilot projects
Canada’s first safer supply programs were introduced in Ontario in 2016. Those programs were initially small in scope, intended for a small group of high-risk individuals.
In 2020, the federal government began funding safer supply pilot programs across the country. Provinces are responsible for the delivery and regulation of these programs.
B.C. introduced provincewide programs in 2021. Other provinces, such as Alberta, have restricted safer supply access to a very small number of clinics, and have generally shifted away from harm reduction models in favour of recovery-oriented approaches.
According to the Canadian Public Health Association, an advocacy organization, the original goal for safer supply was to reduce deaths and harms associated with the unregulated toxic drug supply. It was not meant to replace addiction treatment, but to rather act as a bridge to further care.
However, a 2023 report by researchers at McMaster University and Simon Fraser University noted safer supply “does not principally operate toward goals of treatment or recovery.” The report describes safer supply instead as an emergency intervention focused on stabilization and survival.
Evidence gaps
There is a small but growing body of short-term studies on the health effects of Canada’s safer supply programs. Most only track participants’ outcomes for up to 12 months.
Some of those studies suggest safer supply may reduce the immediate harms associated with drug use.
A 2024 study found a 91 per cent reduction in the risk of death among high-risk individuals receiving safer supply in B.C. Critics have raised concerns about the study’s methodology, sample size and confounding variables.
In contrast, a March study suggested B.C.’s safer supply and decriminalization policies may be associated with increased hospitalizations. These findings also sparked controversy, with experts debating how well the data isolate causal impacts.
And a comparative study released in April also showed some positive outcomes from safer supply. It too sparked significant expert debate.
‘Arms-length’
Of all the provinces, B.C. has implemented safer supply most broadly. The province’s health ministry did not directly respond when asked about the long-term goals of its safer supply program, or whether B.C. collects longitudinal data on program participants’ health outcomes.
“Evidence shows [safer supply] helps separate people from the unregulated drug supply, manage their substance use and withdrawal symptoms with regulated medications, and helps connect them to voluntary health and social supports,” a Ministry of Health spokesperson told Canadian Affairs in an email.
The ministry did not provide the evidence it referenced.
At the federal level, Health Canada confirmed that, to date, it has funded just two evaluations of safer supply programs, despite spending more than $100 million on safer supply since April 2023.
The first was a short-term study, funded by the federal government’s Substance Use and Addictions Program program. Conducted over four months, that study assessed 10 safer supply programs in Ontario, B.C., and New Brunswick. It documented initial impacts on participants’ lives and program delivery, primarily through qualitative methods such as interviews and surveys.
The second study is an ongoing, “arms-length evaluation” of 11 safer supply pilot programs funded by the Canadian Institutes of Health Research (CIHR), Canada’s federal health research agency.
When asked about long-term research on safer supply, Health Canada referred Canadian Affairs to a 2022 funding announcement about this multi-year evaluation. While the evaluation is being conducted over several years, it is unclear if it includes long-term tracking of patients’ outcomes.
Barriers and resistance
There are a number of factors that make it challenging to evaluate safer supply programs over long periods.
Ali, of CAMH, says unstable, short-term funding can disrupt long-term research.
“When programs are shut down or scaled back, we lose contact with participants and the ability to track outcomes over time,” she said.
Program participants can also be difficult to track over long periods, she says. Many struggle with housing insecurity, health instability and criminalization.
Frontline staff also face burnout and high turnover, she says, limiting support for such research activities.
Additionally, there are tradeoffs between the anonymity needed to encourage patients to access safer supply programs and the ability to collect detailed data.
“Ethical concerns — like not wanting to burden participants or risk their safety or confidentiality — require us to design studies that are trauma-informed and flexible, which adds complexity to long-term data collection,” Ali said.
Julian Somers, a clinical psychologist and professor at Simon Fraser University, says B.C.’s failure to conduct long-term evaluations of its safer supply programs is not just an oversight, but an act of negligence.
“B.C. has some of the best pharmaceutical data systems in the world,” Somers said, referring to PharmaCare and PharmaNet — databases that capture every prescription drug transaction in the province.
Somers says his team previously used PharmaNet data to examine prescribed opioids’ effects on health and social outcomes. In 2017, he proposed a long-term safer supply evaluation using these tools.
In 2017, he proposed a long-term evaluation of B.C.’s safer supply programs.
The province declined.
According to Ali, “Future research should explore how safer supply impacts people’s long-term health, stability and connection to care.”
“We also need to listen to people’s experiences, how safer supply affects their daily lives, their sense of dignity, and their relationships with care providers through qualitative mechanisms.”
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Addictions
Why B.C.’s new witnessed dosing guidelines are built to fail

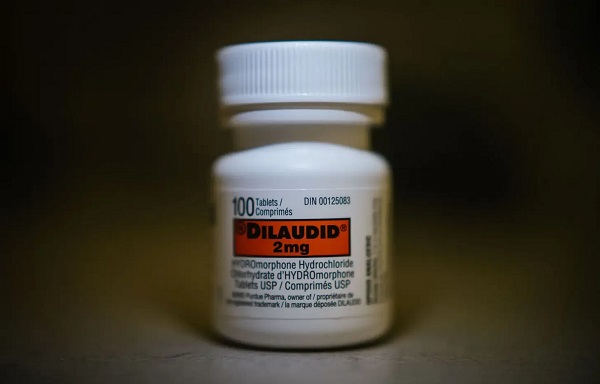
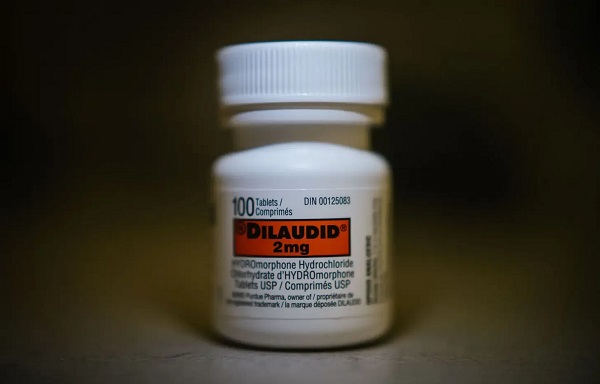
Photo by Acceptable at English Wikipedia, ‘Two 1 mg pills of Hydromorphone, prescribed to me after surgery.’ [Licensed under CC BY-SA 3.0, via Wikimedia Commons]
By Alexandra Keeler
B.C. released new witnessed dosing guidelines for safer supply opioids. Experts say they are vague, loose and toothless
This February, B.C pledged to reintroduce witnessed dosing to its controversial safer supply program.
Safer supply programs provide prescription opioids to people who use drugs. Witnessed dosing requires patients to consume those prescribed opioids under the supervision of a health-care professional, rather than taking their drugs offsite.
The province said it was reintroducing witnessed dosing to “prevent the diversion of prescribed opioids and hold bad actors accountable.”
But experts are saying the government’s interim guidelines, released April 29, are fundamentally flawed.
“These guidelines — just as any guidelines for safer supply — do not align with addiction medicine best practices, period,” said Dr. Leonara Regenstreif, a primary care physician specializing in substance use disorders. Regenstreif is a founding member of Addiction Medicine Canada, an advocacy group that represents 23 addiction specialists.
Addiction physician Dr. Michael Lester, who is also a founding member of the group, goes further.
“Tweaking a treatment protocol that should not have been implemented in the first place without prior adequate study is not much of an advancement,” he said.
Witnessed dosing
Initially, B.C.’s safer supply program was generally administered through witnessed dosing. But in 2020, to facilitate access amidst pandemic restrictions, the province moved to “take-home dosing,” allowing patients to take their prescription opioids offsite.
After pandemic restrictions were lifted, the province did not initially return to witnessed dosing. Rather, it did so only recently, after a bombshell government report alleged more than 60 B.C. pharmacies were boosting sales by encouraging patients to fill unnecessary opioid prescriptions. This incentivized patients to sell their medications on the black market.
B.C.’s interim guidelines, developed by the BC Centre on Substance Use at the government’s request, now require all new safer supply patients to begin with witnessed dosing.
But for existing patients, the guidelines say prescribers have discretion to determine whether to require witnessed dosing. The guidelines define an existing patient as someone who was dispensed prescription opioids within the past 30 days.
The guidelines say exemptions to witnessed dosing are permitted under “extraordinary circumstances,” where witnessed dosing could destabilize the patient or where a prescriber uses “best clinical judgment” and determines diversion risk is “very low.”
Holes
Clinicians say the guidelines are deliberately vague.
Regenstreif described them as “wordy, deliberately confusing.” They enable prescribers to carry on as before, she says.
Lester agrees. Prescribers would be in compliance with these guidelines even if “none of their patients are transferred to witnessed dosing,” he said.
In his view, the guidelines will fail to meet their goal of curbing diversion.
And without witnessed dosing, diversion is nearly impossible to detect. “A patient can take one dose a day and sell seven — and this would be impossible to detect through urine testing,” Lester said.
He also says the guidelines do not remove the incentive for patients to sell their drugs to others. He cites estimates from Addiction Medicine Canada that clients can earn up to $20,000 annually by selling part of their prescribed supply.
“[Prescribed safer supply] can function as a form of basic income — except that the community is being flooded with addictive and dangerous opioids,” Lester said.
Regenstreif warns that patients who had been diverting may now receive unnecessarily high doses. “Now you’re going to give people a high dose of opioids who don’t take opioids,” she said.
She also says the guidelines leave out important details on adjusting doses for patients who do shift from take-home to witnessed dosing.
“If a doctor followed [the guidelines] to the word, and the patient followed it to the word, the patient would go into withdrawal,” she said.
The guidelines assume patients will swallow their pills under supervision, but many crush and inject them instead, Regenstreif says. Because swallowing is less potent, a higher dose may be needed.
“None of that is accounted for in this document,” she said.
Survival strategy
Some harm reduction advocates oppose a return to witnessed dosing, saying it will deter people from accessing a regulated drug supply.
Some also view diversion as a life-saving practice.
Diversion is “a harm reduction practice rooted in mutual aid,” says a 2022 document developed by the National Safer Supply Community of Practice, a group of clinicians and harm reduction advocates.
The group supports take-home dosing as part of a broader strategy to improve access to safer supply medications. In their document, they say barriers to accessing safer supply programs necessitate diversion among people who use drugs — and that the benefits of diversion outweigh the risks.
However, the risks — and harms — of diversion are mounting.
People can quickly develop a tolerance to “safer” opioids and then transition to more dangerous substances. Some B.C. teenagers have said the prescription opioid Dilaudid was a stepping stone to them using fentanyl. In some cases, diversion of these drugs has led to fatal overdoses.
More recently, a Nanaimo man was sentenced to prison for running a highly organized drug operation that trafficked diverted safer supply opioids. He exchanged fentanyl and other illicit drugs for prescription pills obtained from participants in B.C.’s safer supply program.
Recovery
Lester, of Addiction Medicine Canada, believes clinical discretion has gone too far. He says take-home dosing should be eliminated.
“Best practices in addiction medicine assume physicians prescribing is based on sound and thorough research, and ensuring that their prescribing does not cause harm to the broader community, as well as the patient,” he said.
“[Safer supply] for opioids fails in both these regards.”
He also says safer supply should only be offered as a short-term bridge to patients being started on proven treatments like buprenorphine or methadone, which help reduce drug cravings and manage withdrawal symptoms.
B.C.’s witnessed dosing guidelines say prescribers can discuss such treatment options with patients. However, the guidelines remain neutral on whether safer supply is intended as a transitional step toward longer-term treatment.
Regenstreif says this neutrality undermines care.
“[M]ost patients I’ve seen with opioid use disorder don’t want to have [this disorder],” she said. “They would rather be able to set goals and do other things.”
Oversight gaps
Currently, about 3,900 people in B.C. participate in the safer supply program — down from 5,200 in March 2023.
The B.C. government has not provided data on how many have been transitioned to witnessed dosing. Investigative journalist Rob Shaw recently reported that these data do not exist.
“The government … confirmed recently they don’t have any mechanism to track which ‘safe supply’ participants are witnessed and which [are] not,” said Elenore Sturko, a Conservative MLA for Surrey-Cloverdale, who has been a vocal critic of safer supply.
“Without a public report and accountability there can be no confidence.”
The BC Centre on Substance Use, which developed the interim guidelines, says it does not oversee policy decisions or data tracking. It referred Canadian Affairs’ questions to B.C.’s Ministry of Health, which has yet to clarify whether it will track and publish transition data. The ministry did not respond to requests for comment by deadline.
B.C. has also not indicated when or whether it will release final guidelines.
Regenstreif says the flawed guidelines mean many people may be misinformed, discouraged or unsupported when trying to reduce their drug use and recover.
“We’re not listening to people with lived experience of recovery,” she said.
This article was produced through the Breaking Needles Fellowship Program, which provided a grant to Canadian Affairs, a digital media outlet, to fund journalism exploring addiction and crime in Canada. Articles produced through the Fellowship are co-published by Break The Needle and Canadian Affairs.
Subscribe to Break The Needle
-

 Energy2 days ago
Energy2 days agoIs The Carney Government Making Canadian Energy More “Investible”?
-

 Immigration2 days ago
Immigration2 days agoUnregulated medical procedures? Price Edward Islanders Want Answers After Finding Biomedical Waste From PRC-Linked Monasteries
-
 Business2 days ago
Business2 days agoDemocracy Watchdog Says PM Carney’s “Ethics Screen” Actually “Hides His Participation” In Conflicted Investments
-

 Business2 days ago
Business2 days agoCompetition Bureau is right—Canada should open up competition in the air
-

 Business2 days ago
Business2 days agoIt’s Time To End Canada’s Protectionist Supply Management Regime
-

 COVID-192 days ago
COVID-192 days agoFreedom Convoy leaders’ sentencing hearing to begin July 23 with verdict due in August
-
 Addictions2 days ago
Addictions2 days agoAfter eight years, Canada still lacks long-term data on safer supply
-

 National2 days ago
National2 days agoLiberals push to lower voting age to 16 in federal elections