Health
RFK Jr on vaccinations in his own words
Historically, independent candidates running in US Presidential elections barely make a dent on the campaign. The independents aren’t just fighting for votes, they’re fighting for any attention from the media and chattering classes they can muster. As they inevitably flame out, they’ll try desperately to make the world pay attention to the one or two issues that drove them to take on the campaign in the first place.
Seemingly, this is where we are today with RFK Jr. On August 23, Robert Kennedy ponders the end of his campaign. In the final hours before he announces his decision, when his campaign arguably has the most attention, RFK decided to use the spotlight to bring attention to the issue he presumably cares about more than anything else.. the pharmaceutical industry.
Anyone paying attention will have heard over and over again that RFK is an “anti-vaxer”. Anti-Vaxer is a slang used by media and opponents to tarnish anyone who doesn’t endorse vaccines entirely. The amount of opposition, their reasons for it, are not important. A broad spectrum of people who range from those slightly suspicious of one or two vaccines, all the way to those who don’t trust any vaccines in the least (are there really any people like this?).. all painted with the same brush. All pushed into a group they likely have little affiliation with.
With the maximum attention focused on the RFK Jr campaign for a few hours, Kennedy took the opportunity to set the record straight regarding his position on all vaccines.
Why should we care? Well it’s being assumed that RFK will drop out of the race and support Donald Trump for President. If Trump wins, he’ll be indebted to RFK for his support and will very likely offer him a role in his cabinet. That role will very likely put RFK Jr in a position to do something about the pharmaceutical industry.
It’s likely any major changes in the way the industry is regulated in the US will have ripple effects around the world.
What might we expect? That will become clearer from watching Kennedy explain exactly what he things of the vaccine industry.
Today I’m going to set the record straight by explaining my exact posture, point-by-point, on what is probably the most controversial issue of my campaign—a medical safety issue that impacts every one of us. If you take a few minutes to listen, I think you might be surprised to… pic.twitter.com/FJucMmUexF
— Robert F. Kennedy Jr (@RobertKennedyJr) August 22, 2024
Business
National dental program likely more costly than advertised

From the Fraser Institute
By Matthew Lau
At the beginning of June, the Canadian Dental Care Plan expanded to include all eligible adults. To be eligible, you must: not have access to dental insurance, have filed your 2024 tax return in Canada, have an adjusted family net income under $90,000, and be a Canadian resident for tax purposes.
As a result, millions more Canadians will be able to access certain dental services at reduced—or no—out-of-pocket costs, as government shoves the costs onto the backs of taxpayers. The first half of the proposition, accessing services at reduced or no out-of-pocket costs, is always popular; the second half, paying higher taxes, is less so.
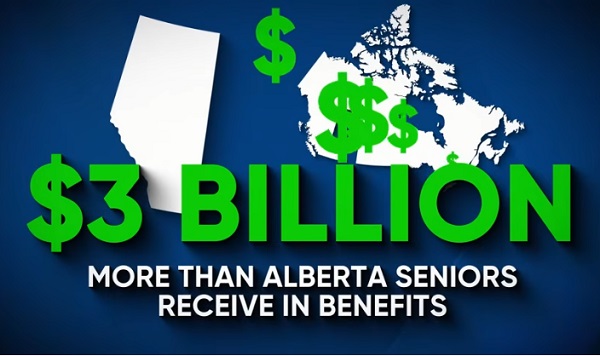
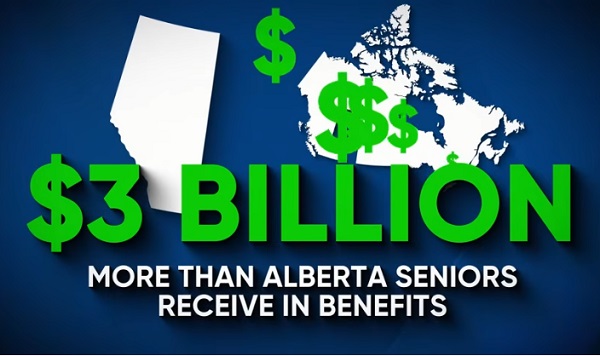
A Leger poll conducted in 2022 found 72 per cent of Canadians supported a national dental program for Canadians with family incomes up to $90,000—but when asked whether they would support the program if it’s paid for by an increase in the sales tax, support fell to 42 per cent. The taxpayer burden is considerable; when first announced two years ago, the estimated price tag was $13 billion over five years, and then $4.4 billion ongoing.
Already, there are signs the final cost to taxpayers will far exceed these estimates. Dr. Maneesh Jain, the immediate past-president of the Ontario Dental Association, has pointed out that according to Health Canada the average patient saved more than $850 in out-of-pocket costs in the program’s first year. However, the Trudeau government’s initial projections in the 2023 federal budget amounted to $280 per eligible Canadian per year.
Not all eligible Canadians will necessarily access dental services every year, but the massive gap between $850 and $280 suggests the initial price tag may well have understated taxpayer costs—a habit of the federal government, which over the past decade has routinely spent above its initial projections and consistently revises its spending estimates higher with each fiscal update.
To make matters worse there are also significant administrative costs. According to a story in Canadian Affairs, “Dental associations across Canada are flagging concerns with the plan’s structure and sustainability. They say the Canadian Dental Care Plan imposes significant administrative burdens on dentists, and that the majority of eligible patients are being denied care for complex dental treatments.”
Determining eligibility and coverage is a huge burden. Canadians must first apply through the government portal, then wait weeks for Sun Life (the insurer selected by the federal government) to confirm their eligibility and coverage. Unless dentists refuse to provide treatment until they have that confirmation, they or their staff must sometimes chase down patients after the fact for any co-pay or fees not covered.
Moreover, family income determines coverage eligibility, but even if patients are enrolled in the government program, dentists may not be able to access this information quickly. This leaves dentists in what Dr. Hans Herchen, president of the Alberta Dental Association, describes as the “very awkward spot” of having to verify their patients’ family income.
Dentists must also try to explain the program, which features high rejection rates, to patients. According to Dr. Anita Gartner, president of the British Columbia Dental Association, more than half of applications for complex treatment are rejected without explanation. This reduces trust in the government program.
Finally, the program creates “moral hazard” where people are encouraged to take riskier behaviour because they do not bear the full costs. For example, while we can significantly curtail tooth decay by diligent toothbrushing and flossing, people might be encouraged to neglect these activities if their dental services are paid by taxpayers instead of out-of-pocket. It’s a principle of basic economics that socializing costs will encourage people to incur higher costs than is really appropriate (see Canada’s health-care system).
At a projected ongoing cost of $4.4 billion to taxpayers, the newly expanded national dental program is already not cheap. Alas, not only may the true taxpayer cost be much higher than this initial projection, but like many other government initiatives, the dental program already seems to be more costly than initially advertised.
Business
RFK Jr. says Hep B vaccine is linked to 1,135% higher autism rate

From LifeSiteNews
By Matt Lamb
They got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data
The Centers for Disease Control and Prevention (CDC) found newborn babies who received the Hepatitis B vaccine had 1,135-percent higher autism rates than those who did not or received it later in life, Robert F. Kennedy Jr. told Tucker Carlson recently. However, the CDC practiced “trickery” in its studies on autism so as not to implicate vaccines, Kennedy said.
RFK Jr., who is the current Secretary of Health and Human Services, said the CDC buried the results by manipulating the data. Kennedy has pledged to find the causes of autism, with a particular focus on the role vaccines may play in the rise in rates in the past decades.
The Hepatitis B shot is required by nearly every state in the U.S. for children to attend school, day care, or both. The CDC recommends the jab for all babies at birth, regardless of whether their mother has Hep B, which is easily diagnosable and commonly spread through sexual activity, piercings, and tattoos.
“They kept the study secret and then they manipulated it through five different iterations to try to bury the link and we know how they did it – they got rid of all the older children essentially and just had younger children who were too young to be diagnosed and they stratified that, stratified the data,” Kennedy told Carlson for an episode of the commentator’s podcast. “And they did a lot of other tricks and all of those studies were the subject of those kind of that kind of trickery.”
But now, Kennedy said, the CDC will be conducting real and honest scientific research that follows the highest standards of evidence.
“We’re going to do real science,” Kennedy said. “We’re going to make the databases public for the first time.”
He said the CDC will be compiling records from variety of sources to allow researchers to do better studies on vaccines.
“We’re going to make this data available for independent scientists so everybody can look at it,” the HHS secretary said.
— Matt Lamb (@MattLamb22) July 1, 2025
Health and Human Services also said it has put out grant requests for scientists who want to study the issue further.
Kennedy reiterated that by September there will be some initial insights and further information will come within the next six months.
Carlson asked if the answers would “differ from status quo kind of thinking.”
“I think they will,” Kennedy said. He continued on to say that people “need to stop trusting the experts.”
“We were told at the beginning of COVID ‘don’t look at any data yourself, don’t do any investigation yourself, just trust the experts,”‘ he said.
In a democracy, Kennedy said, we have the “obligation” to “do our own research.”
“That’s the way it should be done,” Kennedy said.
He also reiterated that HHS will return to “gold standard science” and publish the results so everyone can review them.
-

 Agriculture2 days ago
Agriculture2 days agoCanada’s supply management system is failing consumers
-

 Business1 day ago
Business1 day agoCanada’s loyalty to globalism is bleeding our economy dry
-

 armed forces23 hours ago
armed forces23 hours agoCanada’s Military Can’t Be Fixed With Cash Alone
-

 Economy2 days ago
Economy2 days agoTrump opens door to Iranian oil exports
-

 Alberta1 day ago
Alberta1 day agoCOVID mandates protester in Canada released on bail after over 2 years in jail
-
 Alberta23 hours ago
Alberta23 hours agoAlberta Next: Alberta Pension Plan
-

 International1 day ago
International1 day agoTrump transportation secretary tells governors to remove ‘rainbow crosswalks’
-
 Business1 day ago
Business1 day agoCarney’s spending makes Trudeau look like a cheapskate