Alberta
Ottawa’s next phase of ‘plastics’ war will increase cost of fruits and vegetables
From the Fraser Institute
For decades, nutrition advocates have exhorted Canadians to eat more fresh fruits and vegetables. Canada’s Food Guide suggests that half of our meals should be fruits and veggies. Why then does the Trudeau government plan to increase fruit and vegetable waste—and increase their costs?
It’s all about the government’s war on plastics, specifically its agenda to eliminate plastic waste by 2030. Having already banned single-use plastic items such as drinking straws, stir sticks and plastic cutlery, the government plans to target plastic food packaging. And that’s going to hit consumers in the pocket.
According to a new study from the Canadian Produce Marketing Association (CPMA), under the new reduced-plastic packaging regime, food loss and waste will potentially increase 495,000 tonnes above current levels, incurring financial losses valued at $3.4 billion. These losses, at least in significant part, will ultimately be passed onto consumers. In a report by CTV, reporter Kevin Gallagher suggests that increased costs to consumers might reach 30 per cent.
The study authors suggest this estimate should be considered conservative, because it does not include the potential for single-use plastic bans causing a “complete disruption to some sectors of the fresh produce industry, and the anticipated 17.5 per cent increase in operating costs voiced by respondents that industry would incur.” And 17.5 per cent is the median—cost increases ranged from 11 per cent to 25 per cent. Assuming these increased costs are passed onto consumers, Canadians will see the price of fruits and veggies take yet another jump.
And for what reason? The Trudeau government has foolishly committed Canada to a “Zero Plastic Waste by 2030” crusade. But as I showed in a 2022 study published by the Fraser Institute, Canada does not have a significant plastic waste problem. Less than 1 per cent of plastics used in Canada end up as waste in the environment, and 99 per cent is safely buried in landfills, recycled or incinerated. Canada does not contribute a measurable part of the world’s plastic pollution.
And the government’s own analysis suggests that pursuing this war on plastics will ultimately lead to greater waste of alternative materials, which is already raising concerns among the environmentally-minded. In a separate CTV report Melanie Nagy quotes Nicole Rycroft, founder of Canopy, a forest conservation NGO, who said we should “shift away from using plastics as much as we do, but trading in plastic pollution for deforestation and forest degradation is not the answer” and we must “make sure we do not create another environmental disaster.” Rycroft added that “more than three billion trees—many of which are old-growth and endangered—are logged every year to make paper-based products like bags, straws and food containers.”
The Trudeau government’s zero plastic waste crusade was unsound policy from inception, and its own analysis showed the plan’s costs would outstrip its benefits and that it would create more waste, not less. And that most of that increased waste would come from increased consumption of wood and paper products.
Now, the government plans to ratchet up this harmful program, raising already painfully expensive produce in Canada to more painful levels. Ottawa must halt its “Zero Plastic Waste” agenda and take the entire concept back to the drawing board. It’s simply bad policy—bad for Canadian families, bad for our food sector, and as the Canopy tree people observe, bad for the environment.
Author:
Alberta
Temporary Alberta grid limit unlikely to dampen data centre investment, analyst says
From the Canadian Energy Centre
By Cody Ciona
‘Alberta has never seen this level and volume of load connection requests’
Billions of investment in new data centres is still expected in Alberta despite the province’s electric system operator placing a temporary limit on new large-load grid connections, said Carson Kearl, lead data centre analyst for Enverus Intelligence Research.
Kearl cited NVIDIA CEO Jensen Huang’s estimate from earlier this year that building a one-gigawatt data centre costs between US$60 billion and US$80 billion.
That implies the Alberta Electric System Operator (AESO)’s 1.2 gigawatt temporary limit would still allow for up to C$130 billion of investment.
“It’s got the potential to be extremely impactful to the Alberta power sector and economy,” Kearl said.
Importantly, data centre operators can potentially get around the temporary limit by ‘bringing their own power’ rather than drawing electricity from the existing grid.
In Alberta’s deregulated electricity market – the only one in Canada – large energy consumers like data centres can build the power supply they need by entering project agreements directly with electricity producers.
According to the AESO, there are 30 proposed data centre projects across the province.
The total requested power load for these projects is more than 16 gigawatts, roughly four gigawatts more than Alberta’s demand record in January 2024 during a severe cold snap.
For comparison, Edmonton’s load is around 1.4 gigawatts, the AESO said.
“Alberta has never seen this level and volume of load connection requests,” CEO Aaron Engen said in a statement.
“Because connecting all large loads seeking access would impair grid reliability, we established a limit that preserves system integrity while enabling timely data centre development in Alberta.”
As data centre projects come to the province, so do jobs and other economic benefits.
“You have all of the construction staff associated; electricians, engineers, plumbers, and HVAC people for all the cooling tech that are continuously working on a multi-year time horizon. In the construction phase there’s a lot of spend, and that is just generally good for the ecosystem,” said Kearl.
Investment in local power infrastructure also has long-term job implications for maintenance and upgrades, he said.
“Alberta is a really exciting place when it comes to building data centers,” said Beacon AI CEO Josh Schertzer on a recent ARC Energy Ideas podcast.
“It has really great access to natural gas, it does have some excess grid capacity that can be used in the short term, it’s got a great workforce, and it’s very business-friendly.”
The unaltered reproduction of this content is free of charge with attribution to the Canadian Energy Centre.
Alberta
Alberta Next: Taxation

A new video from the Alberta Next panel looks at whether Alberta should stop relying on Ottawa to collect our provincial income taxes. Quebec already does it, and Alberta already collects corporate taxes directly. Doing the same for personal income taxes could mean better tax policy, thousands of new jobs, and less federal interference. But it would take time, cost money, and require building new systems from the ground up.
-

 Uncategorized13 hours ago
Uncategorized13 hours agoCNN’s Shock Climate Polling Data Reinforces Trump’s Energy Agenda
-

 illegal immigration2 days ago
illegal immigration2 days agoICE raids California pot farm, uncovers illegal aliens and child labor
-

 Energy1 day ago
Energy1 day agoLNG Export Marks Beginning Of Canadian Energy Independence
-

 Business1 day ago
Business1 day agoCarney government should apply lessons from 1990s in spending review
-

 Entertainment1 day ago
Entertainment1 day agoStudy finds 99% of late-night TV guests in 2025 have been liberal
-

 Frontier Centre for Public Policy13 hours ago
Frontier Centre for Public Policy13 hours agoCanada’s New Border Bill Spies On You, Not The Bad Guys
-
 Opinion6 hours ago
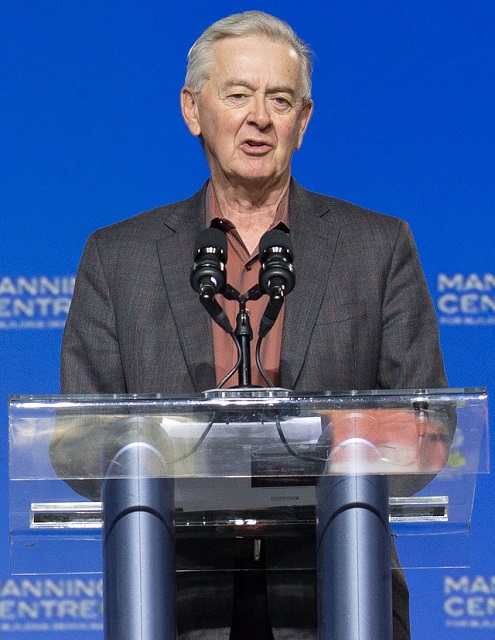
Opinion6 hours agoPreston Manning: Three Wise Men from the East, Again
-

 Addictions5 hours ago
Addictions5 hours agoWhy B.C.’s new witnessed dosing guidelines are built to fail